
Deep learning image reconstruction in pediatric abdominal and chest computed tomography: a comparison of image quality and radiation dose
Introduction
The radiation dose of computed tomography (CT) examination in pediatric patients is a public health concern. Cell division is higher in children than in adults because children undergo rapid growth and development, placing them at higher risk of injury from exposure to high ionizing radiation (1). In a pediatric population, it is critical to pay attention to the management of image quality and radiation dose reduction in the CT examination.
Several iterative reconstruction (IR) algorithms have emerged in recent years (2-4). Although studies have shown that the adaptive statistical iterative reconstruction-Veo (ASiR-V) algorithm can provide lower image noise and artifacts at a lower radiation dose (5-7), the nonlinear and non-stationary peculiarities of the ASiR-V algorithm may change the characteristics of image noise in the reconstructed image. The radiologist’s confidence in the image may be reduced due to changes in noise texture (8,9). The images obtained through ASiR-V algorithms may hinder interpretation of the diagnosis, thereby limiting the application of the highest iteration level and the potential for dose reduction in clinical practice (10).
With the recent development of artificial intelligence, new reconstruction methods have been gradually applied to the field of medical imaging technology (11,12). Consequently, some CT manufacturers have developed a new generation of CT image reconstruction based on deep learning. The deep learning image reconstruction (DLIR) algorithms developed by GE Healthcare and Canon Medical Systems feature a deep neural network (DNN), which is trained respectively with high-quality filtered back projection (FBP; True Fidelity™, GE Healthcare, Chicago, IL, USA) and MBIR [Advanced intelligent Clear-IQ Engine (AiCE); Canon Medical System, Tochigi, Japan] datasets to learn how to achieve dose reduction (13) and reconstruct CT images without changing noise texture or affecting anatomical structure (14,15). Recent research has suggested that DLIR enables image quality that is superior to commercial IR images during an adult CT protocol (16). A phantom study was conducted on the application of DLIR in pediatric CT examination (17); however, phantom studies are only suitable for simple and objective assessment as well as dosimetry experiments requiring repeated scans, which may be inconsistent with clinical practice. To promote the practicality of clinical research, image quality evaluations related to clinical tasks should be conducted based on the pediatric population.
Therefore, the purpose of this study was to conduct a preliminary phantom study and a practical clinical study to assess the impact on image quality and the dose reduction potential of the DLIR algorithm in the pediatric CT protocol compared to ASiR-V.
We present the following article in accordance with the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-21-936/rc).
Methods
Study design and CT protocols
Phantom study
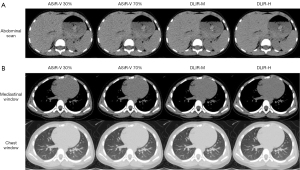
A pediatric phantom of approximately 110 cm in height and 20 kg in weight was used (PBU-70, General Boom, Figure 1). We acquired CT images of the abdomen and chest with a helical scanning on a 256-slice CT scanner (Revolution CT, GE Healthcare, Milwaukee, WI, USA). The tube voltages of 80 kVp and 70 kVp were used to acquire abdominal and chest images, respectively. Tube currents (mA) were set to automatic modulation, and noise index (NI) was divided into 6 groups (NI=5, 8, 11, 13, 15, and 18). The remaining acquisition parameters for abdominal and chest scanning were a pitch factor of 0.992, beam collimation of 0.625 mm × 40 mm and 0.625 mm × 80 mm, matrix of 512×512, and a rotation time of 0.50 seconds and 0.28 seconds, respectively. Images were reconstructed with ASiR-V 30%, ASiR-V 70%, DLIR-M (medium), and DLIR-H (high). For objective image evaluation, the axial images were reconstructed with a 0.625 mm increment and 0.625 mm slice thickness and a field of view (FOV) of 250 mm. The scan parameters are shown in Table 1.
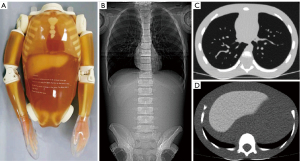
Table 1
| Scanning site | Chest | Abdomen |
|---|---|---|
| Pitch | 0.992 | |
| Size (mm) | 205×145 | 200×150 |
| Beam collimation (mm) | 0.625×80 | 0.625×40 |
| Rotation time (s) | 0.28 | 0.5 |
| Tube voltage (kVp) | 70 | 80 |
| NI | 5; 8; 11; 13; 15; 18 | 5; 8; 11; 13; 15; 18 |
| Tube current (mA) | 374; 353; 243; 198; 129; 89 | 374; 336; 193; 99; 80; 44 |
| CTDIvol (mGy) | 1.46; 1.41; 0.87; 0.75; 0.46; 0.31 | 3.89; 1.95; 1.01; 0.71; 0.53; 0.36 |
| Image reconstruction | ASiR-V 30%, ASiR-V70%, DLIR medium and high | |
CT, computed tomography; ASiR-V, adaptive statistical iterative reconstruction-V; DLIR, deep learning image reconstruction; CTDI, computed tomographic dose index; NI, noise index; CTDIvol, computed tomography dose index volume.
Patient study
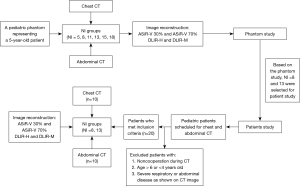
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Board of Tianjin First Central Hospital, and informed consent was provided by all the patients’ parents or legal guardians. All data in this study were exported completely anonymously for research purposes before processing. Authors have complete control over the data and information submitted for publication. For our study, raw data (June to December 2020) were obtained prospectively by using the same CT scanner with the same scanning and reconstruction protocols as in the phantom study. During the scan, the examined children did not use contrast agents or tranquilizers and breathed freely. We included patients who (I) had a similar body size and were aged 4–6 years, (II) had satisfactory cooperation during CT examination, and (III) had normal chest and abdominal CT images. Patients meeting the criteria were randomly assigned to either scanning group. In both abdominal and chest studies, NI was divided into 8 and 13 groups (representing the normal-dose and low-dose level, respectively). The difference in NI was intended to reflect the performance of ASiR-V and DLIR at different acceptable dose levels. The flow chart of the study is shown in Figure 2.
Estimation of image quality
Reading and evaluation of all images was performed on the picture archiving and communication system (PACS) viewer (Infinitt Healthcare, Seoul, Korea).
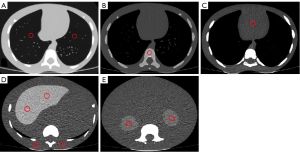
Objective evaluation
We obtained CT attenuation of abdominal and chest organs (liver, kidney, subcutaneous fat for abdomen and lung, mediastinum, and spine for chest) by sketching circular regions of interest (ROIs) on the axial images by 2 independent radiology doctors (XIE, with 8 years of experience; SHI, with 13 years of experience). The ROIs were delineated by selecting multiple layers centered on the largest layer of the organ. A total of 6 layers were drawn from the mediastinum and spine with 1 ROI on each layer, and 3 layers were drawn from abdominal organs (liver, kidney, and subcutaneous fat) and the lung with 2 ROIs on each layer. In total, 6 datasets were obtained and recorded from each organ, and the area of each ROI was 100 mm2. The outlined ROIs were as far away from the marginal portion of the tissue or organ as possible to circumvent the impact of partial volume effects (Figure 3).
The CT dose index volume (CTDIvol) of the phantom and children scans with each NI was recorded. In each NI group, 6 datasets were measured for every organ with both ASiR-V and DLIR algorithms. Image noise (N) was defined as the standard deviation of the CT attenuation of the subcutaneous fat. Signal-to-noise ratios (SNR; attenuation divided by noise) of each tissue and organs were obtained, and contrast-to-noise ratio (CNR) calculation formulas of liver and kidney (CNRliv and CNRkid) were as follows:
Subjective evaluation
The subjective image score was visually evaluated by 2 independent experienced radiologists (SHI, with 13 years of experience; SUN, with 23 years of experience). To ensure the internal evaluation of the readers was reliable, a doctor conducted a second evaluation 1 week later. The 4 reconstructed datasets (ASiR-V 30%, ASiR-V 70%, DLIR-M, and DLIR-H) were presented to each reader in random order, with the reader unaware of the reconstruction information. The levels evaluated included the thoracic entrance, largest level of the sternal stalk, tracheal bifurcation, maximum level of the heart shadow, bottom of the lung, parietal level, maximum level of the liver, floor of the liver, maximum level of the left kidney, and the largest level of the right kidney. The quality of each selected axial image was scored according to the 5-point Likert grading standard (Table S1).
Estimation of radiation dose reduction
The N value was modeled as a function of radiation dose level (D) and reconstruction level (R) of the form (18) as follows:
where N is the image noise, µ is an intercept coefficient, α is a radiation dose coefficient, and β is a reconstruction level coefficient (19) (Appendix 1).
A value of P=0.05 was considered statistically significant.
Statistical analysis
All analysis was conducted using R software (version 3.5.3; The R Foundation for Statistical Computing, Vienna, Austria). Interobserver agreement of the objective and subjective evaluations was evaluated by calculating the intraclass correlation coefficient (ICC) and Flessis’s Kappa Coefficient, respectively. In the phantom study, the CT value, N, CNR, and SNR were compared on images reconstructed with ASiR-V and with DLIR using the one-way repeated measures analysis of variance (ANOVA). In the patient study, the pairwise comparison was done using Bonferroni correction. The quality score on the phantom and patient image datasets was compared using the Wilcoxon signed-rank test. Statistical significance was considered when P<0.05.
Results
Phantom study
Objective evaluation
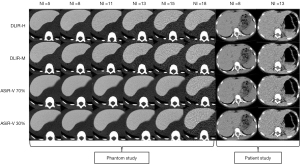
The interobserver assessment of the objective data measurement demonstrated good agreement {ICC [95% confidence interval (CI)]: 0.814 (0.732 to 0.892) for the abdomen, 0.801 (0.711 to 0.843) for the chest}. The CTDIvol of scans with NI=5, 8, 11, 13, 15, and 18 was 3.89, 1.95, 1.01, 0.75, 0.53, and 0.36 mGy for the abdomen, respectively, and 1.46, 1.41, 0.87, 0.71, 0.46, and 0.31 mGy for the chest, respectively. The results of the multiple comparison showed that in most situations within the same dose level, the N increased, while CNR and SNR decreased with the decrease of radiation dose in each reconstruction (Figure 4). The CT value remained the same (P>0.05) (Tables S2,S3). The DLIR-H most effectively reduced the noise and improved SNR and CNR. Taking the liver as an example, from ASiR-V 30% to DLIR-H in the NI=8 group, N decreased by up to 14.6 HU (58.7%), SNR increased by up to 4.8 (149.7%), and CNR increased by up to 4.8 (140.8%). Pairwise comparison of these 4 reconstructions showed that the performance of ASiR-V 70% and DLIR-M was similar (P>0.05) (Appendix 2).

Subjective evaluation
The interobserver assessment of the data measurement demonstrated moderate or substantial agreement (κ=0.660 for abdomen, 0.588 for chest). The subjective scores of DLIR were higher than those of ASiR-V. The performance of DLIR-H was the best, with a higher score than that of other groups, and the performance of DLIR-M was similar to that of ASiR-V 70% (Tables S4,S5) (P>0.05).
Radiation dose reduction
The DLIR-H exhibited the best performance when the radiation dose was reduced; it had approximately 70% (abdomen) and 60% (chest) of the dose reduction compared to ASiR-V 70% in the low reference dose group. The ability of DLIR-M and ASiR-V 70% perform with reduced radiation dose was almost the same and both fared better than ASiR-V 30% (Tables 2,3).
Table 2
| Comparison | Abdomen | ||
|---|---|---|---|
| Reference dose =4.5 mGy | Reference dose =3.0 mGy | Reference dose =1.5 mGy | |
| ASiR-V70 vs. ASiR-V30 | 53.20% | 79.80% | 159.70% |
| DLIR-M vs. ASiR-V30 | 48.70% | 73% | 146% |
| DLIR-H vs. ASiR-V30 | 73.10% | 109.60% | 219.20% |
| DLIR-M vs. ASiR-V70 | 4.60% | 6.80% | 13.70% |
| DLIR-H vs. ASiR-V70 | 24.40% | 36.60% | 73.20% |
| DLIR-H vs. DLIR-M | 19.80% | 29.80% | 59.50% |
CT, computed tomography; ASiR-V, adaptive statistical iterative reconstruction-V; DLIR-M, deep learning image reconstruction with medium degree; DLIR-H, deep learning image reconstruction with high degree.
Table 3
| Comparison | Chest | ||
|---|---|---|---|
| Reference dose =1.5 mGy | Reference dose =1.0 mGy | Reference dose =0.5 mGy | |
| ASiR-V70 vs. ASiR-V30 | 45.10% | 67.60% | 135.20% |
| DLIR-M vs. ASiR-V30 | 50.80% | 76.10% | 152.30% |
| DLIR-H vs. ASiR-V30 | 65% | 97.50% | 194.90% |
| DLIR-M vs. ASiR-V70 | 5.70% | 8.50% | 17% |
| DLIR-H vs. ASiR-V70 | 19.90% | 29.90% | 59.70% |
| DLIR-H vs. DLIR-M | 14.20% | 21.30% | 42.70% |
CT, computed tomography; ASiR-V, adaptive statistical iterative reconstruction-V; DLIR-M, deep learning image reconstruction with medium degree; DLIR-H, deep learning image reconstruction with high degree.
Patient study
Finally, a total of 20 children (12 boys) who were similar in size to the phantom were recruited and grouped. The mean age of the patients was 5.4±1.2 years.
Objective evaluation
The interobserver assessment of the data measurement demonstrated good agreement [ICC (95% CI): 0.774 (0.683 to 0.861) for the abdomen, 0.751 (0.664 to 0.844) for the chest]. For the CT scan of the abdomen in children, the CTDIvol with NI=8 and 13 were 1.79±0.05 and 0.77±0.09 mGy; and for the chest scan, the CTDIvol with NI=8 and 13 were 1.41±0.24 mGy and 0.65±0.08 mGy, respectively. In the abdominal study, DLIR-H played the greatest role in noise reduction and SNR improvement in all organs in both the NI=8 and NI=13 groups (P<0.05). In the chest study, for the tissues with extreme CT values, such as lungs and bone, the value of DLIR for image optimization was not demonstrated (Tables 4,5).
Table 4
| NI | Liver | Kidney | Fat | Subjective score | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | SNR | CNR | N | SNR | CNR | N | SNR | Abdomen | ||||
| 8 | ||||||||||||
| ASIR-V 30% | 26.0±1.4 | 2.4b,c±0.7 | 7.1±0.8 | 25.0±0.6 | 1.8±0.06 | 6.7±0.6 | 26.9±2.9 | −4.6b±0.7 | 2.2±0.1 | |||
| ASIR-V 70% | 17.7c±1.3 | 3.5a,c,d±1.0 | 10.4c±1.2 | 16.7±0.1 | 2.7c±0.04 | 10.1c±0.6 | 19.4c±2.8 | −6.4a,c±1.0 | 2.6±0.1 | |||
| DLIR-M | 19.5b±1.9 | 3.2a,b,d±0.9 | 9.5b±1.2 | 18.1±0.8 | 2.5b±0.08 | 9.3b±0.5 | 17.5b,d±2.0 | −7.0b±0.9 | 3.1±0.2 | |||
| DLIR-H | 14.5±2.1 | 4.3b,c±1.0 | 12.8±1.1 | 13.4±1.0 | 3.4±0.20 | 12.5±0.5 | 13.0c±2.0 | −9.5±1.3 | 3.8±0.2 | |||
| P value | <0.001* | 0.032* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |||
| 13 | ||||||||||||
| ASIR-V 30% | 32.8±2.0 | 2.0±0.2 | 5.6±0.4 | 33.4±1.1 | 1.4±0.1 | 4.9±0.7 | 31.9±2.1 | −4.0±0.4 | 1.5±0.1 | |||
| ASIR-V 70% | 23.6±1.7 | 2.8c±0.3 | 8.2±0.4 | 24.1±1.0 | 1.9c±0.2 | 7.1c±0.5 | 23.3c±1.7 | −5.4c±0.6 | 2.0±0.1 | |||
| DLIR-M | 26.8±1.3 | 2.5b±0.2 | 7.2±0.3 | 27.0±0.9 | 1.7b±0.1 | 6.4b±0.3 | 22.4b±2.2 | −5.7b±0.6 | 2.4±0.1 | |||
| DLIR-H | 19.2±1.0 | 3.5±0.3 | 10.1±0.5 | 19.6±1.6 | 2.4±0.2 | 8.9±0.8 | 15.7±1.7 | −8.1±0.9 | 3.2±0.2 | |||
| P value | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | |||
*, represents statistically significant difference. The level of statistical significance was set at P<0.05. The superscripts (a, b, c, d) represent the same group of the Bonferroni post hoc test (the alphabetical order indicates the order, from ASIR-V 30% to DLIR-H). NI, noise index; CT, computed tomography; ASiR-V, adaptive statistical iterative reconstruction-V; DLIR-M, deep learning image reconstruction with medium level; DLIR-H, deep learning image reconstruction with high level; N, image noise; SNR, signal-to-noise ratios; CNR, contrast-to-noise ratio.
Table 5
| NI | Lung | Mediastinum | Spine | Subjective score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | SNR | N | SNR | N | SNR | Chest | |||||
| 8 | |||||||||||
| ASIR-V 30% | 26.3d±1.6 | −29.0b,c,d±3.6 | 21.6±1.5 | 2.5±0.3 | 43.3±1.3 | 7.5b,c,d±1.0 | 2.9±0.1 | ||||
| ASIR-V 70% | 21.9±1.8 | −34.7a±4.7 | 14.2c±1.3 | 3.8c±0.4 | 37.7c,d±2.1 | 8.6a,c,d±1.0 | 2.9±0.2 | ||||
| DLIR-M | 30.8d±1.2 | −24.5a,d±2.0 | 14.0b±1.0 | 3.8b±0.4 | 39.3b±0.7 | 8.1a,b,d±1.1 | 3.2±0.1 | ||||
| DLIR-H | 29.1a,c±1.5 | −26.0a,c±2.4 | 10.3±0.7 | 5.2±0.5 | 35.9b±0.9 | 8.9a,b,c±1.2 | 3.3±0.1 | ||||
| P value | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | 0.208 | 0.783 | ||||
| 13 | |||||||||||
| ASIR-V 30% | 32.9b,d±4.7 | −23.8b,c,d±3.7 | 28.9±1.0 | 1.8±0.1 | 44.9b,c,d±2.2 | 7.2b,c,d±1.0 | 2.8±0.1 | ||||
| ASIR-V 70% | 27.2a±4.6 | −29.0a±5.2 | 19.6c±0.9 | 2.7c±0.1 | 39.1a,c,d±3.4 | 8.2a,c,d±1.1 | 2.8±0.3 | ||||
| DLIR-M | 41.4d±4.3 | −18.8a,d±2.3 | 21.1b±1.8 | 2.6b±0.2 | 45.9a,b,d±4.1 | 7.0a,b,d±1.0 | 2.9±0.2 | ||||
| DLIR-H | 38.2a,c±3.8 | −20.2a,c±2.4 | 14.7±0.8 | 3.7±0.3 | 40.8a,b,c±5.0 | 7.9a,b,c±1.1 | 3.1±0.1 | ||||
| P value | <0.001* | 0.002* | <0.001* | <0.001* | 0.037 | 0.251 | 0.465 | ||||
*, represents statistically significant difference. The level of statistical significance was set at P<0.05. The superscripts (a, b, c, d) represent the same group of the Bonferroni post hoc test (the alphabetical order indicates the order, from ASIR-V 30% to DLIR-H). CT, computed tomography; NI, noise index; ASiR-V, adaptive statistical iterative reconstruction-V; DLIR-M, deep learning image reconstruction with medium level; DLIR-H, deep learning image reconstruction with high level; N, image noise; SNR, signal-to-noise ratios.
Subjective evaluation
The interobserver assessment of the data measurement demonstrated moderate agreement (κ=0.561 for the abdomen, 0.558 for the chest). In the abdominal study, DLIR-H had the highest subjective score and was statistically different from the other groups. In the chest study, there was no statistically significant difference in subjective scores between the 4 reconstruction methods. Figure 5 depicts a comparison of image quality at each dose level and under all DLIR and ASiR-V algorithms in the liver. For all algorithms, the image noise increased with the decrease of dose, which deteriorated the image sharpness and contrast. In the ASiR-V images, the edge blurring effect and degradation of noise texture of liver were pronounced, which caused excessive image smoothing. Compared with ASiR-V, the images obtained by DLIR were favored by radiologists because they reduced image noise without changing or blurring the texture of the liver. In the chest study, DLIR-H only played a significant role in mediastinal image optimization (Figure 6).
Discussion
In this study, the phantom and pediatric clinical patients were used to evaluate DLIR and IR algorithms. It was shown that DLIR can significantly improve image quality, reduce image noise, and reduce potential dose capacity in abdominal examination and chest mediastinal examination under the same slice thickness.
The DLIR is not based on traditional reconstruction algorithms, but rather on artificial intelligence. The DLIR reconstruction algorithm was designed to distinguish between signal and noise to reduce the noise of the reconstructed image without noise texture degradation or pixel coarseness that are often exhibited by IR algorithms (20,21). In our phantom study, we set up 6 groups of NI, which represented different radiation doses from high to low levels. The performance of DLIR-H was the best in terms of objective and subjective evaluation at the same NI group, which was consistent with Racinea et al.’s research (22). The ASiR-V 70% performed better than ASiR-V 30%, but had a similar performance to DLIR-M. Moreover, from the subjective analysis, ASiR-V 70% changed the noise texture and affected the true readability of the image, which led to a lower subjective score compared with DLIR-H. Greffier et al.’s (17) study supported our findings, but they did not further verify the results in a patient population. In our patient study, we found that compared with ASiR-V, DLIR-H had a greater role in image quality improvement in the abdomen study. This added to results previously presented by Akagi et al. (23) who, with the same DLIR algorithm, demonstrated that DLIR images in the abdominal ultra-high-spatial-resolution CT images had a lower quantum noise and were generally preferred in comparison to hybrid and model-based iterative reconstruction (hybrid-IR, MBIR).
In previous adult studies, researchers demonstrated noise reduction ability through ASiR-V reconstruction algorithm (24,25). However, our study demonstrated the limitations of high-level ASiR-V (70%) in terms of texture loss and showed that related dose optimization poses a risk to image quality and diagnosis. This was a similar conclusion to that of McCollough et al. (26). In addition, it is difficult to use high-level IR reconstruction in clinical practice because of excessive image smoothing (27). The results of our study confirmed that DLIR was more valuable than ASiR-V in improving the image quality of abdominal pediatric CT examinations.
Greater focus should be given to the impacts of radiation exposure on children during CT examination than adults because radiation exposure can impact children’s development and growth. A low radiation dose during pediatric CT examination is recommended. Sun et al. (28) found that it was feasible to improve the image quality of a low radiation dose and contrast volume chest computed tomography angiography (CTA) in children using the DLIR algorithm. Furthermore, Brady et al. (29) supposed that the DLIR algorithm improved image quality without sacrificing noise texture and spatial resolution in the contrast agent-enhanced pediatric CT examinations. Our study reached similar conclusions. We first conducted the phantom study and then verified the results of the phantom study through a prospective chest-abdominal study of pediatric patients. In addition, we evaluated the radiation dose reduction of 2 reconstruction algorithms with different weights. Our phantom study results showed that DLIR-H allowed reduction of radiation dose to a greater extent compared to ASiR-V. This reduction effect was more evident in the low reference dose group. In Haggerty’s (30) study, compared with FBP, the IR algorithm reduced the radiation dose in the pediatric chest by approximately 46–56%. In our pediatric chest study, DLIR-H reduced the radiation dose by approximately 60% compared to ASiR-V70%. Shin et al. (13) found that DLIR trained with a 50% simulated radiation dose showed the best overall image quality compared to ASiR-V in the adult abdomen. In our pediatric abdominal study, DLIR-H performed the best compared to ASiR-V 70%, with a dose reduction of approximately 70%. Therefore, DLIR can balance the requirements for a lower radiation dose and higher image quality in pediatric CT scans. These findings have value for the clinical application of CT in children.
The value of this new reconstruction technique to improve image quality has not been widely confirmed. In our study, DLIR-H performed well in image optimization of children’s abdominal organs and thoracic mediastinum. This is because the DLIR algorithm can only be reconstructed under the standard kernel, which is widely used in soft tissue inspection. This indicates that DLIR may be more suitable for CT examination of soft tissues in children, such as the abdomen, and further clinical verification is needed. The application of the DLIR algorithm in routine clinical practice may mark the beginning of a new era of CT image reconstruction, clinical CT schemes, and CT diagnostic reference levels.
Our study had some limitations. First, this study was limited in terms of acquisition parameters such as tube voltage, layer thickness, and FOV. In future studies, it will be necessary to further investigate additional acquisition and/or reconstruction parameters appropriate for each clinical indication to further characterize the DLIR algorithm. Second, the number of each group was relatively small, and more comprehensive clinical data will need to be collected to improve the limitations. Third, rather than a specific disease, our study focused on the analysis of image quality and dose optimization. In future studies, we will collect data and analyze the application value of DLIR in related diseases.
Conclusions
DLIR could help to reduce the radiation dose without sacrificing the image quality during pediatric CT scans. Compared with ASiR-V, DLIR-H had the best in image quality and dose optimization, especially in abdominal applications. Further clinical validation is required.
Acknowledgments
Funding: This study was funded by the National Natural Science Fund of China (No. 81901710); the National Natural Science Fund of China (No. 81873888); the Science and Technology fund of Tianjin (No. QN20024); and the Science and Technology fund of Tianjin (No. TJWJ2021QN011). This study was funded by Tianjin Key Medical Discipline (Specialty) Construction Project.
Footnote
Reporting Checklist: The authors have completed the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-21-936/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form. ZHL, SZ, and JYS report that they are employees of GE Healthcare (available at https://qims.amegroups.com/article/view/10.21037/qims-21-936/coif). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional board of Tianjin First Central Hospital, and informed consent was obtained from all the patients’ parents or legal guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Strauss KJ, Somasundaram E, Sengupta D, Marin JR, Brady SL. Radiation Dose for Pediatric CT: Comparison of Pediatric versus Adult Imaging Facilities. Radiology 2019;291:158-67. [Crossref] [PubMed]
- Geyer LL, Schoepf UJ, Meinel FG, Nance JW Jr, Bastarrika G, Leipsic JA, Paul NS, Rengo M, Laghi A, De Cecco CN. State of the Art: Iterative CT Reconstruction Techniques. Radiology 2015;276:339-57. [Crossref] [PubMed]
- Tabari A, Ramandeep S, Khera RD, Hoi Y, Angel E, Kalra MK, Madan R. Can fully iterative reconstruction technique enable routine abdominal CT at less than 1 mSv? Eur J Radiol Open 2019;6:225-30. [Crossref] [PubMed]
- Thibault JB, Sauer KD, Bouman CA, Hsieh J. A three-dimensional statistical approach to improved image quality for multislice helical CT. Med Phys 2007;34:4526-44. [Crossref] [PubMed]
- Greffier J, Frandon J, Larbi A, Beregi JP, Pereira F. CT iterative reconstruction algorithms: a task-based image quality assessment. Eur Radiol 2020;30:487-500. [Crossref] [PubMed]
- Kim HG, Lee HJ, Lee SK, Kim HJ, Kim MJ, Head CT. Image quality improvement with ASIR-V using a reduced radiation dose protocol for children. Eur Radiol 2017;27:3609-17. [Crossref] [PubMed]
- Han WK, Na JC, Park SY. Low-dose CT angiography using ASiR-V for potential living renal donors: a prospective analysis of image quality and diagnostic accuracy. Eur Radiol 2020;30:798-805. [Crossref] [PubMed]
- Verdun FR, Racine D, Ott JG, Tapiovaara MJ, Toroi P, Bochud FO, Veldkamp WJH, Schegerer A, Bouwman RW, Giron IH, Marshall NW, Edyvean S. Image quality in CT: From physical measurements to model observers. Phys Med 2015;31:823-43. [Crossref] [PubMed]
- Samei E, Richard S. Assessment of the dose reduction potential of a model-based iterative reconstruction algorithm using a task-based performance metrology. Med Phys 2015;42:314-23. [Crossref] [PubMed]
- Greffier J, Frandon J, Pereira F, Hamard A, Beregi JP, Larbi A, Omoumi P. Optimization of radiation dose for CT detection of lytic and sclerotic bone lesions: a phantom study. Eur Radiol 2020;30:1075-8. [Crossref] [PubMed]
- Dou Qi, Chen Hao, Yu Lequan, Zhao Lei, Qin Jing, Wang Defeng, Mok VC, Shi Lin. Pheng-Ann Heng. Automatic Detection of Cerebral Microbleeds From MR Images via 3D Convolutional Neural Networks. IEEE Trans Med Imaging 2016;35:1182-95. [Crossref] [PubMed]
- Roth HR, Lu L, Seff A, Cherry KM, Hoffman J, Wang S, Liu J, Turkbey E, Summers RM. A new 2.5D representation for lymph node detection using random sets of deep convolutional neural network observations. Med Image Comput Comput Assist Interv 2014;17:520-7.
- Shin YJ, Chang W, Ye JC, Kang E, Oh DY, Lee YJ, Park JH, Kim YH. Low-Dose Abdominal CT Using a Deep Learning-Based Denoising Algorithm: A Comparison with CT Reconstructed with Filtered Back Projection or Iterative Reconstruction Algorithm. Korean J Radiol 2020;21:356-64. [Crossref] [PubMed]
- Jensen CT, Liu X, Tamm EP, Chandler AG, Sun J, Morani AC, Javadi S, Wagner-Bartak NA. Image Quality Assessment of Abdominal CT by Use of New Deep Learning Image Reconstruction: Initial Experience. AJR Am J Roentgenol 2020;215:50-7. [Crossref] [PubMed]
- Shan H, Padole A, Homayounieh F, Kruger U, Khera RD, Nitiwarangkul C, Kalra MK, Wang G. Competitive performance of a modularized deep neural network compared to commercial algorithms for low-dose CT image reconstruction. Nat Mach Intell 2019;1:269-76. [Crossref] [PubMed]
- Singh R, Digumarthy SR, Muse VV, Kambadakone AR, Blake MA, Tabari A, Hoi Y, Akino N, Angel E, Madan R, Kalra MK. Image Quality and Lesion Detection on Deep Learning Reconstruction and Iterative Reconstruction of Submillisievert Chest and Abdominal CT. AJR Am J Roentgenol 2020;214:566-73. [Crossref] [PubMed]
- Greffier J, Hamard A, Pereira F, Barrau C, Pasquier H, Beregi JP, Frandon J. Image quality and dose reduction opportunity of deep learning image reconstruction algorithm for CT: a phantom study. Eur Radiol 2020;30:3951-9. [Crossref] [PubMed]
- Cameron AC, Trivedi PK. Regression analysis of count data. Cambridge.
- Euler A, Solomon J, Marin D, Nelson RC, Samei E. A Third-Generation Adaptive Statistical Iterative Reconstruction Technique: Phantom Study of Image Noise, Spatial Resolution, Lesion Detectability, and Dose Reduction Potential. AJR Am J Roentgenol 2018;210:1301-8. [Crossref] [PubMed]
- Haggerty JE, Smith EA, Kunisaki SM, Dillman JR. CT imaging of congenital lung lesions: effect of iterative reconstruction on diagnostic performance and radiation dose. Pediatr Radiol 2015;45:989-97. [Crossref] [PubMed]
- JHsieh J, Liu E, Nett B. A new era of image reconstruction: TrueFidelity™. Technical white paper on deep learning image reconstruction. GE Healthcare 2019.
- Racine D, Becce F, Viry A, Monnin P, Thomsen B, Verdun FR, Rotzinger DC. Task-based characterization of a deep learning image reconstruction and comparison with filtered back-projection and a partial model-based iterative reconstruction in abdominal CT: A phantom study. Phys Med 2020;76:28-37. [Crossref] [PubMed]
- Akagi M, Nakamura Y, Higaki T, Narita K, Honda Y, Zhou J, Yu Z, Akino N, Awai K. Deep learning reconstruction improves image quality of abdominal ultra-high-resolution CT. Eur Radiol 2019;29:6163-71. [Crossref] [PubMed]
- Tang H, Liu Z, Hu Z, He T, Li D, Yu N, Jia Y, Shi H. Clinical value of a new generation adaptive statistical iterative reconstruction (ASIR-V) in the diagnosis of pulmonary nodule in low-dose chest CT. Br J Radiol 2019;92:20180909. [Crossref] [PubMed]
- Tenant S, Pang CL, Dissanayake P, Vardhanabhuti V, Stuckey C, Gutteridge C, Hyde C, Roobottom C. Intra-patient comparison of reduced-dose model-based iterative reconstruction with standard-dose adaptive statistical iterative reconstruction in the CT diagnosis and follow-up of urolithiasis. Eur Radiol 2017;27:4163-72. [Crossref] [PubMed]
- McCollough CH, Yu L, Kofler JM, Leng S, Zhang Y, Li Z, Carter RE. Degradation of CT Low-Contrast Spatial Resolution Due to the Use of Iterative Reconstruction and Reduced Dose Levels. Radiology 2015;276:499-506. [Crossref] [PubMed]
- Jensen CT, Wagner-Bartak NA, Vu LN, Liu X, Raval B, Martinez D, Wei W, Cheng Y, Samei E, Gupta S. Detection of Colorectal Hepatic Metastases Is Superior at Standard Radiation Dose CT versus Reduced Dose CT. Radiology 2019;290:400-9. [Crossref] [PubMed]
- Sun J, Li H, Li J, Yu T, Li M, Zhou Z, Peng Y. Improving the image quality of pediatric chest CT angiography with low radiation dose and contrast volume using deep learning image reconstruction. Quant Imaging Med Surg 2021;11:3051-8. [Crossref] [PubMed]
- Brady SL, Trout AT, Somasundaram E, Anton CG, Li Y, Dillman JR. Improving Image Quality and Reducing Radiation Dose for Pediatric CT by Using Deep Learning Reconstruction. Radiology 2021;298:180-8. [Crossref] [PubMed]
- Haggerty JE, Smith EA, Kunisaki SM, Dillman JR. CT imaging of congenital lung lesions: effect of iterative reconstruction on diagnostic performance and radiation dose. Pediatr Radiol 2015;45:989-97. [Crossref] [PubMed]


