
Elevated 131I-MIBG activity in adrenocortical adenoma—what other imaging options do we have?
Introduction
Metaiodobenzylguanidine (MIBG) functional imaging can detect neuroblastoma with high sensitivity and specificity (1). Its diagnostic accuracy for primary pheochromocytoma (PC), malignant PC, and multiple endocrine neoplasia is also very high (2). Therefore, 131I/123I-MIBG scintigraphy is recommended to screen for PC in patients with abnormal hypertension, especially in those with suspicious adrenal lesions (3). However, adrenocortical adenoma can cause false positive results, as illustrated by this case report.
Case presentation
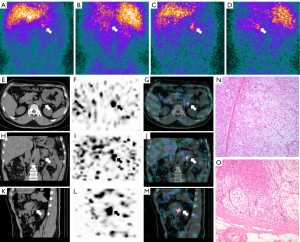
A 54-year-old man presented with repeated headaches for 6 months and hypertension. Recorded blood pressure measurements were as high as 238/138 mmHg. Laboratory testing revealed a slightly elevated plasma cortisol concentration of 569.5 nmol/L (8 AM, normal range, 171–536 nmol/L). Plasma and urinary catecholamine concentrations were within normal limits and 24-h urinary total metanephrines were 1,616nmol/d (normal range, 0–1,622nmol/d). The serum renin/aldosterone levels was 21.84 (normal range, 0–32). The 8 AM adrenocor ticotropic (ACTH) levels were also within normal limits (35.47 pg/mL, normal range, 7–64 pg/mL). The patient was 172 cm in height and weighed 87.6 kg (body mass index, 29.6 kg/m2). His physical examination was otherwise unremarkable (no signs of an excessive production of adrenocortical steroids such as in Cushing’s syndrome). Both parents had a history of hypertension. Genetic testing was not performed. Unenhanced abdominal computed tomography (CT) performed at an outside hospital revealed a small homogeneous micronodule (<1 cm) in the left adrenal. He was then referred to our hospital for 131I-MIBG scintigraphy. Scintigraphy showed elevated activity in the upper left abdomen at 24 h that was more prominent on the 72-h scan (Figure 1A-1D). Single-photon emission (SPECT)/CT imaging at 48 h confirmed uptake of 131I-MIBG in the left adrenal (Figure 1E-1M). Although PC was suspected based on the imaging findings in the presence of severe hypertension, the laboratory findings were not consistent with PC. However, the patient’s blood pressure remained poorly controlled despite medical therapy. He took perindopril (4 mg daily), indapamide sustained-release tablets (1.5 mg daily), spironolactone (40 mg daily) and bexinostat (60 mg daily) for blood control. Therefore, we elected to proceed with a left retroperitoneal laparoscopic adrenalectomy after obtaining informed consent. The final pathological diagnosis was adrenocortical adenoma (Figure 1N-1O). One month after operation, his blood pressure was controlled with bexinostat (30 mg daily) and terazosin hydrochloride (2 mg daily) and remained normal during one year of follow-up.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
A diagnosis of PC can be made when a patient has a history of hypertension, elevated serum and urinary metanephrine concentrations (catecholamine metabolites), and positive findings on MIBG scintigraphy (1,4). However, approximately 6.2% of patients with negative results for urinary metanephrines, in these patients the MIBG results could be negative or positive (5). MIBG is the first-line functional imaging agent used in neuroblastoma imaging and has high sensitivity and specificity (1). Diagnostic accuracy of MIBG is also very high for primary and malignant PC and multiple endocrine neoplasia (5). The reported specificities and sensitivities of 123/131I-MIBG scintigraphy for PC range from 77% to 100% and 85% to100%, respectively (3,6,7). Other diagnoses that may cause positive MIBG scintigraphy include normal adrenal, adrenal metastasis of choriocarcinoma, adrenocortical adenoma (8-12), focal pyelonephritis, small ischemic kidney, hepatic hemangioma, dilated renal pelvis, and adenomatous polyp of the caecum (13-15). In our patient, elevated 131I-MIBG activity was found in an adrenocortical adenoma. Previously reported adenomas causing false-positive MIBG scintigraphy were greater than 1.8 cm in diameter (10-12); however, the lesion in our patient was much smaller, measuring 0.9 cm in largest dimension. It is unusual for a lesion of this size to cause significant tracer uptake.
The mechanism responsible for abnormal MIBG uptake in adrenocortical adenoma remains unknown. Coexisting medullary hyperplasia, dense medullary granules within the nodule, and concurrent paraganglioma have been offered as possible explanations (10-12). Another possibility is disturbed cellular uptake of MIBG relative to that of noradrenaline (5,16).
Studies have shown that 18F-fluorodihydroxyphenylalanine (18F-FDOPA) positron emission tomography (PET)/CT can provide additional diagnostic and localization information regarding PCs, as 18F-FDOPA uptake may be enhanced by overactivity of catecholamine exocytosis (17,18). Moreover, 18F-FDOPA has shown better diagnostic performance than MIBG and 18F-fluorodeoxyglucose (18F-FDG), particularly for hypersecreting PCs, and has fewer drug interactions. We suggest that 18F-FDOPA be used as the first-line tracer for PC diagnosis and staging.
Other imaging techniques can also be helpful to distinguish adrenocortical adenoma. Attenuation of these lesions is typically <10 Hounsfield units on unenhanced CT (19,20). On opposed-phase magnetic resonance imaging, adrenocortical adenoma demonstrates rapid washout and loss of signal (21). 18F-FDG PET/CT can differentiate malignant lesions from adrenal adenomas using a maximum standard uptake value (SUVmax) cutoff of 3.1 (22,23). In addition, 11C-metomidate has been suggested as a tracer to distinguish cortical and non-cortical adrenal lesions and is used to evaluate incidental adrenal masses (24,25). Furthermore, 131I-6-betaiodomethyl-19-norcholesterol (NP-59) can accumulate in the adrenal cortex and has been reported to have high specificity and accuracy for identification of adrenocortical lesions, especially primary aldosteronism (PA) (26). NP‑59 SPECT/CT is safe. It can provide accurate lateralization, and can improve clinical outcome in patients with PAassociated hypertension (27). In our case, based on the symptoms of the abnormal hypertension and laboratory results, PC and PA could not be excluded. However, NP-59 scan was not available in our hospital. The patient was referred a 131I-MIBG scan to have further diagnosis.
According to the European Society of Endocrinology Clinical Practice guidelines, unilateral adrenalectomy is recommended for patients with a unilateral adrenal mass that secretes hormones or having imaging findings suspicious for malignancy (28). However, there is no clear consensus on the definition of abnormal cortisol secretion; therefore, indications for adrenalectomy remain controversial (29). Laparoscopic surgery is the standard approach for PC resection (6,7) and was utilized in our patient. Although his laboratory results were not consistent with PC, we elected to proceed with adrenalectomy because of poorly controlled hypertension. It was possible that the patient had a PC, PA, or functional adrenal mass that should have been surgically treated (6). After surgery, his blood pressure returned to normal.
Our case demonstrates that even a small adrenocortical adenoma can accumulate MIBG and cause a diagnostic dilemma when evaluating a patient for possible PC. Clinicians should be aware of other diagnostic options such as 18F-FDOPA, 18F-FDG, or 11C-metomidate PET/CT and 131I-NP-59 SPECT/CT.
Acknowledgements
We thank Matthew Wetzel, MD, from Liwen Bianji (Edanz) for editing the language of a draft of this manuscript.
Funding: This research was supported by National Natural Science Foundation of China (No. 81801737 and 81771863), China Scholarship Council (CSC) Visiting Scholar Grant (No. 201906165056) (to Dr. Xiaotian Xia).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-21-904/coif). XX reports that this research was supported by National Natural Science Foundation of China (No. 81801737), China Scholarship Council (CSC) and Visiting Scholar Grant (No. 201906165056). YZ reports that this research was supported by National Natural Science Foundation of China (No. 81771863). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was reviewed and approved by the Ethics Committee of Union Hospital, Tongji Medical College. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharp SE, Trout AT, Weiss BD, Gelfand MJ. MIBG in Neuroblastoma Diagnostic Imaging and Therapy. Radiographics 2016;36:258-78. [Crossref] [PubMed]
- Vallabhajosula S, Nikolopoulou A. Radioiodinated metaiodobenzylguanidine (MIBG): radiochemistry, biology, and pharmacology. Semin Nucl Med 2011;41:324-33. [Crossref] [PubMed]
- Havekes B, King K, Lai EW, Romijn JA, Corssmit EP, Pacak K. New imaging approaches to phaeochromocytomas and paragangliomas. Clin Endocrinol (Oxf) 2010;72:137-45. [Crossref] [PubMed]
- Low G, Dhliwayo H, Lomas DJ. Adrenal neoplasms. Clin Radiol 2012;67:988-1000. [Crossref] [PubMed]
- Kawashima A, Sone M, Inagaki N, Okamoto K, Tsuiki M, Izawa S, Otsuki M, Okamura S, Ichijo T, Katabami T, Takeda Y, Yoshimoto T, Naruse M, Tanabe A. Pheochromocytoma and paraganglioma with negative results for urinary metanephrines show higher risks for metastatic diseases. Endocrine 2021;74:155-62. [Crossref] [PubMed]
- Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, Naruse M, Pacak K, Young WF Jr. Endocrine Society. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2014;99:1915-42. [Crossref] [PubMed]
- Pappachan JM, Tun NN, Arunagirinathan G, Sodi R, Hanna FWF. Pheochromocytomas and Hypertension. Curr Hypertens Rep 2018;20:3. [Crossref] [PubMed]
- Kekäläinen P, Alhava E, Vanninen E, Niskanen L. A pitfall of metaiodobenzylguanidine scan: paraganglioma in close proximity to adrenocortical adenoma. Exp Clin Endocrinol Diabetes 2003;111:294-7. [Crossref] [PubMed]
- Sone H, Okuda Y, Nakamura Y, Ishikawa H, Yamaoka T, Kawakami Y, Yamashita K. Pitfalls in scanning for phaeochromocytoma. Lancet 1994;344:476-7. [Crossref] [PubMed]
- Sone H, Okuda Y, Nakamura Y, Ishikawa N, Yamaoka T, Kawakami Y, Odawara M, Matsushima T, Kawai K, Yamashita K. Radioiodinated metaiodobenzylguanidine scintigraphy for pheochromocytoma. A false-positive case of adrenocortical adenoma and literature review. Horm Res 1996;46:138-42. [Crossref] [PubMed]
- Letizia C, De Toma G, Massa R, Corsi A, Caliumi C, Subioli S, D'Erasmo E. False-positive diagnosis of adrenal pheochromocytoma on iodine-123-MIBG scan. J Endocrinol Invest 1998;21:779-83. [Crossref] [PubMed]
- Dell'Aversana S, Coppola M, Balestrieri U, Mainenti PP, Pascale C, Imbriaco M, Chianca V, Romeo V, Pellegrino T, Mainolfi C, Maurea S. Integrated Imaging Characterization of Adrenal Adenoma: False-Positive Metaiodobenzylguanidine (MIBG) Findings of Adrenal Scintigraphy. Pol J Radiol 2017;82:422-5. [Crossref] [PubMed]
- Feggi L, Degli Uberti E, Pansini GC, Transforini G, Prandini N, Ambrosio MR, D'Urso AR, Faggioli R. Pitfalls in scintigraphic detection of neuroendocrine tumours. Eur J Nucl Med 1992;19:214-8. [Crossref] [PubMed]
- Horne T, Glaser B, Krausz Y, Rubinger D, Britton KE. Unusual causes of I-131 metaiodobenzylguanidine uptake in non-neural crest tissue. Clin Nucl Med 1991;16:239-42. [Crossref] [PubMed]
- Jacobs A, Lenoir P, Delree M, Ramet J, Piepsz A. Unusual Tc-99m MDP and I-123 MIBG images in focal pyelonephritis. Clin Nucl Med 1990;15:821-4. [Crossref] [PubMed]
- Sato H, Igarashi H, Kishimoto Y, Yamaguchi K, Saito T, Ishida H, Okada K, Okano T. Combined tumor consisting of non-functioning adrenocortical adenoma and pheochromocytoma in the same gland. Int J Urol 2002;9:398-401. [Crossref] [PubMed]
- Lugat A, Drui D, Mirallié E, Kraeber-Bodéré F, Ansquer C. 18F-FDOPA PET Compared With 123I-Metaiodobenzylguanidine Scintigraphy and 18F-FDG PET in Secreting Sporadic Pheochromocytoma. Clin Nucl Med 2019;44:738-40. [Crossref] [PubMed]
- Moog S, Houy S, Chevalier E, Ory S, Weryha G, Rame M, Klein M, Brunaud L, Gasman S, Cuny T. 18F-FDOPA PET/CT Uptake Parameters Correlate with Catecholamine Secretion in Human Pheochromocytomas. Neuroendocrinology 2018;107:228-36. [Crossref] [PubMed]
- Blake MA, Cronin CG, Boland GW. Adrenal imaging. AJR Am J Roentgenol 2010;194:1450-60. [Crossref] [PubMed]
- Corwin MT, Navarro SM, Malik DG, Loehfelm TW, Fananapazir G, Wilson M, Campbell MJ. Differences in Growth Rate on CT of Adrenal Adenomas and Malignant Adrenal Nodules. AJR Am J Roentgenol 2019;213:632-6. [Crossref] [PubMed]
- d'Amuri FV, Maestroni U, Pagnini F, Russo U, Melani E, Ziglioli F, Negrini G, Cella S, Cappabianca S, Reginelli A, Barile A, De Filippo M. Magnetic resonance imaging of adrenal gland: state of the art. Gland Surg 2019;8:S223-32. [Crossref] [PubMed]
- Metser U, Miller E, Lerman H, Lievshitz G, Avital S, Even-Sapir E. 18F-FDG PET/CT in the evaluation of adrenal masses. J Nucl Med 2006;47:32-7. [PubMed]
- Murayama R, Nishie A, Hida T, Baba S, Inokuchi J, Oda Y, Honda H. Uptake of 18F-FDG in Adrenal Adenomas Is Associated With Unenhanced CT Value and Constituent Cells. Clin Nucl Med 2019;44:943-8. [Crossref] [PubMed]
- Zettinig G, Mitterhauser M, Wadsak W, Becherer A, Pirich C, Vierhapper H, Niederle B, Dudczak R, Kletter K. Positron emission tomography imaging of adrenal masses: (18)F-fluorodeoxyglucose and the 11beta-hydroxylase tracer (11)C-metomidate. Eur J Nucl Med Mol Imaging 2004;31:1224-30. [Crossref] [PubMed]
- Bergström M, Juhlin C, Bonasera TA, Sundin A, Rastad J, Akerström G, Långström B. PET imaging of adrenal cortical tumors with the 11beta-hydroxylase tracer 11C-metomidate. J Nucl Med 2000;41:275-82. [PubMed]
- Wu MH, Liu FH, Lin KJ, Sun JH, Chen ST. Diagnostic value of adrenal iodine-131 6-beta-iodomethyl-19-norcholesterol scintigraphy for primary aldosteronism: a retrospective study at a medical center in North Taiwan. Nucl Med Commun 2019;40:568-75. [Crossref] [PubMed]
- Yen RF, Wu VC, Liu KL, Cheng MF, Wu YW, Chueh SC, Lin WC, Wu KD, Tzen KY, Lu CCTAIPAI Study Group. 131I-6beta-iodomethyl-19-norcholesterol SPECT/CT for primary aldosteronism patients with inconclusive adrenal venous sampling and CT results. J Nucl Med 2009;50:1631-7. [Crossref] [PubMed]
- Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 2016;175:G1-G34. [Crossref] [PubMed]
- Bourdeau I, El Ghorayeb N, Gagnon N, Lacroix A. MANAGEMENT OF ENDOCRINE DISEASE: Differential diagnosis, investigation and therapy of bilateral adrenal incidentalomas. Eur J Endocrinol 2018;179:R57-67. [Crossref] [PubMed]


