
This article has an erratum available at: http://dx.doi.org/10.21037/qims-2024-03 the article has been update on 2024-06-24 at here.
Evaluation of tubal patency based on peak injection pressure in four-dimensional hysterosalpingo-contrast sonography among infertile females: a preliminary study
Introduction
Infertility is a complex reproductive disorder that arises from various causes. Worldwide, over 10% of women of reproductive age experience infertility (1-3), and it is estimated that up to two-thirds of these cases are associated with tubal-related factors, of which patency is the most important (4,5). Therefore, the precise evaluation of tubal patency is vital in identifying the underlying cause of infertility and serves as a significant cornerstone for determining optimal treatment.
Currently, various techniques are employed to assess fallopian tubal patency of the tubes, including X-ray hysterosalpingography (HSG) (6,7), hysterosalpingo-contrast sonography (HyCoSy) (8,9), magnetic resonance hysterosalpingography (MR-HSG) (10), hysteroscopic tubal cannulation (11), and laparoscopic chromopertubation (LC) (12). Although LC has been acknowledged as the reference test, HyCoSy has been adopted as one of the first-line options for evaluating infertility due to its simplicity and high diagnostic performance (6,13). HyCoSy evaluates the patency of the fallopian tubes based on the morphology and alignment of the tubes through real-time ultrasound monitoring after injection of the contrast into the uterine cavity. This technique is safe due to its noninvasive and nonradiative nature and can be easily performed in outpatient settings (14,15). Transvaginal four-dimensional HyCoSy (4D-HyCoSy) is a diagnostic technique that can dynamically demonstrate the entire contrast flow from the uterine cavity through the bilateral uterine horns to the fallopian tubes and ultimately into the pelvic cavity (16,17). Furthermore, postcontrast imaging allows for frame-by-frame dynamic playback and segmental analysis of the area of interest, which further improves diagnostic accuracy.
However, the current assessment of tubal patency using 4D-HyCoSy is primarily based on the postimaging morphological findings of the fallopian tubes and pelvic cavity, which lacks objective or quantifiable parameters (9). Previous studies have shown a significant correlation between the volume of contrast agents in HSG and tubal patency in women who have undergone permanent contraceptive procedures. However, the diagnostic efficacy of peak uterine pressure is constrained (18,19). Theoretically, obstruction of the fallopian tubes is expected to increase injection pressure, but there is scant evidence regarding the relationship between peak injection pressure and tubal patency during 4D-HyCoSy. Qiang et al. (9) reported that the slope of the pressure curve during HyCoSy was significantly affected by the patency of fallopian tubes. However, the patency of the fallopian tubes was not confirmed by LC, and the study included a limited number of patients, especially those with obstructed fallopian tubes. Additionally, while it was suggested that the peak pressure after contrast injection was associated with patency, specific details were not provided. Therefore, we hypothesized that pressure measurement could aid in the evaluation of fallopian tube patency. We substantiated this hypothesis by examining the peak pressure values obtained during HyCoSy and their correlation with various states of fallopian tube patency. We present this article in accordance with the STARD reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1569/rc).
Methods
Research patients
This study enrolled patients who were diagnosed with infertility at West China Second Hospital of Sichuan University between 2020 and 2022. Our study included infertile patients who had undergone 4D-HyCoSy and were scheduled by their obstetricians to undergo LC as part of their diagnosis and treatment regimen. Written informed consent was obtained from each patient. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the ethics committee of West China Second Hospital of Sichuan University (2019.No.2).
Infertility is defined as the inability to achieve a spontaneous pregnancy without contraception for more than 1 year of regular sexual activity in females (20). Patients are required to be in good general health to tolerate 4D-HyCoSy, and those who underwent both HyCoSy and LC were included in the final analysis. Patients were excluded if they met any of the following criteria: (I) acute or subacute inflammation of the reproductive system, abnormal vaginal bleeding, coagulation disorders, or hemorrhagic disease; (II) history of abortion or evacuation within 3 months prior to examination; (III) presence of submucosal fibroids; (IV) history of unilateral or bilateral salpingectomy; and (V) incomplete clinical history records.
4D-HyCoSy procedure and real-time injection pressure recording
HyCoSy was performed 3–7 days after menstruation. The procedure included a Voluson E8 ultrasound diagnostic instrument (GE Healthcare, Chicago, IL, USA) equipped with a RIC5-9-D probe, SonoVue contrast agent (Bracco, Milan, Italy), and a YZ-800U liquid injection device with a pressure sensor (Yilida, Zhuhai, China). The contrast agent was prepared following the instructions provided by SonoVue (21). Specifically, one injection vial containing 59 mg of SonoVue powder was suspended with 5 mL of 0.9% sterile saline, and the suspension was further diluted in 45ml of saline.
The 4D-HyCoSy procedure was similar to that in previous reports (16,22). Atropine was routinely administered via intramuscular injection approximately 30 min before HyCoSy to prevent hysterosalpingeal spasm (17). A Foley catheter (12 Fr) was inserted into the uterine cavity after sterilization the vagina, and 1.5–3.0 mL of saline was injected into the balloon (23). The automatic injection rate was set as 10 mL/min after the flux clinic system was initiated on the YZ-800U. Injection ceased automatically when the pressure reached the set threshold (600 mmHg) to ensure patients’ safety.
To begin the scan, a transverse section of the uterus was obtained at the level at which both uterine horns, and if possible, the ovaries, could be displayed (Figure S1). The view angle was adjusted to the maximum of 120° for three-dimensional (3D) imaging prescan in coded contrast imaging (CCI) mode. The probe direction was adjusted accordingly while the reconstruction frame was maximized. Dynamic imaging and injection pressure throughout the HyCoSy procedure were recorded with the luminescence clinic system in 4D mode, which captured the contrast agent’s course from its entry into the uterine cavity, through the fallopian tube, and finally into the pelvic cavity from the distal end of the fallopian tube. Upon completion of the 4D scan, the CCI mode was applied to assess encapsulation around the ovary and pelvic diffusion. Subsequently, the 3D volumetric images were analyzed.
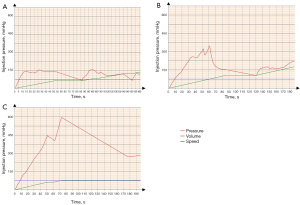
A T-shaped catheter was used for pressure measurement during HyCoSy, with its three heads connected to the uterine cavity, the pressure sensor of the YZ-800U, and the contrast medium, respectively. Injection was initiated at a constant speed of 10 mL/min, and the injection pressure was automatically recorded, generating a real-time pressure curve for further analysis. Representative images of real-time injection pressure during HyCoSy are shown in Figure 1.
Fallopian tube patency was evaluated according to the morphologic appearance of the fallopian tube (24) and categorized as obstructed, partially obstructed, or patent (Table S1). The diagnostic results were interpreted by two experienced imaging physicians. In case of any disagreement, a third physician would review and interpret the imaging data, which would be followed by a thorough discussion until a consensus were reached.
Performance of LC
LC was applied as a reference test to evaluate tubal patency. In this study, the recommended time frame for conducting the LC examination was within 3 months following HyCoSy. The patent status of the fallopian tubes was determined by the exit of methylene blue from the fallopian fimbria. An obstructed fallopian tube generally exhibits significant resistance during injection, with reflux to the cervix or vagina, and an absence of methylene blue overflow from the fallopian fimbria (25,26). To ensure the independence between 4D-HyCoSy and LC procedures, the examiners of both examinations were blinded to the results of the other examination.
Grouping scheme
Patients were divided into three groups based on the patency of both fallopian tubes determined by LC, which included the bilaterally patent, unilaterally patent, and bilaterally nonpatent groups. In the secondary outcome analysis, patients were further divided into six groups based on 4D-HyCoSy results: (I) bilaterally patent (patent/patent); (II) unilaterally patent with the other partially obstructed (patent/partially obstructed); (III) bilaterally partially obstructed (partially obstructed/partially obstructed); (IV) unilaterally obstructed with the other patent (patent/obstructed); (V) unilaterally obstructed with the other partially obstructed (partially obstructed/obstructed); and (VI) bilaterally obstructed (obstructed/obstructed).
Statistical methods
Baseline characteristics of patients were compared using the chi-square test and paired t-test. The accuracy of HyCoSy in identifying nonpatent fallopian tubes was compared with LC using the McNemar test. Discrepancies in peak pressure and contrast agent volume among patients in different tubal patency groups were analyzed using paired t-tests, and the cutoff values were determined using receiver operating characteristic (ROC) analysis. Statistical analyses were conducted using RStudio version 4.3.2 (Boston, MA, USA) and GraphPad Prism version 8.3.0 software (GraphPad Software, Inc., La Jolla, CA, USA). P<0.05 was considered statistically significant.
Results
We conducted 4D-HyCoSy in 359 patients who were scheduled to undergo LC as part of their diagnosis and treatment plan by their obstetricians. No serious adverse events were observed in patients following both HyCoSy and LC procedures. Among these patients, 268 who underwent LC examination within 3 months were included in the primary analysis. The age range of the 268 infertile women was 19–40 years, and the duration of infertility was 1–10 years. Based on the evaluation of fallopian tube patency by LC, the 268 patients were categorized into three groups: 153 cases in the bilaterally patent group (57.1%), 83 in the unilaterally patent group (30.9%), and 32 in the bilaterally nonpatent group (12.0%) (Figure 2).

All patients included in this study were of Asian descent. There were no significant differences in age (P=0.52), bilateral ovarian volume (P=0.59 and P=0.54), or endometrial thickness (P=0.11) among the three groups (Table 1).
Table 1
| Group | Bilaterally patent | Unilaterally patent | Bilaterally nonpatent | P value |
|---|---|---|---|---|
| Number (%) | 153 (57.1) | 83 (30.9) | 32 (12.0) | |
| Ethnicity (%) | Asian (100.0) | Asian (100.0) | Asian (100.0) | >0.99 |
| Age (mean ± SD, years) | 29.57±4.05 | 29.98±4.33 | 30.22±3.71 | 0.52 |
| Endometrial thickness (mean ± SD, cm) | 0.24±0.11 | 0.25±0.09 | 0.28±0.09 | 0.11 |
| Left ovarian volume (mean ± SD, cm3) | 15.66±17.63 | 18.33±20.96 | 16.38±8.76 | 0.59 |
| Right ovarian volume (mean ± SD, cm3) | 16.53±10.16 | 17.24±8.89 | 15.17±8.00 | 0.54 |
SD, standard deviation.
The accuracy of 4D-HyCoSy in evaluating tubal patency was evaluated by comparing its results with those of LC. From the 268 patients, 536 fallopian tubes were analyzed, among which 389 (72.6 %) were patent and 147 (27.4%) nonpatent. As shown in Table 2, 4D-HyCoSy successfully identified 370 (95.1%) patent tubes and 134 (91.1%) nonpatent tubes. The tubal patency assessed by 4D-HyCoSy had a promising concordance with LC (P=0.08).
Table 2
| 4D-HyCoSy | Laparoscopic chromopertubation | P value (McNemar test) | ||
|---|---|---|---|---|
| Patent | Obstructed | Total | ||
| Patent | 370 | 13 | 383 | 0.08 |
| Obstructed | 19 | 134 | 153 | |
| Total | 389 | 147 | 536 | |
4D-HyCoSy, 4-dimensional hysterosalpingo-contrast sonography.
In general, peak injection pressure increased gradually with decreasing tubal patency (Figure 3A). Patients with bilaterally patent tubes showed the lowest peak injection pressure (233.5±66.3 mmHg), followed by those with unilaterally patent tubes (338.8±99.8 mmHg, P<0.001). Unsurprisingly, the highest peak injection pressure was observed in patients with bilaterally nonpatent tubes (469.6±63.2 mmHg; P<0.001).

As expected, the volume of contrast agent used in patients with bilaterally nonpatent tubes was the smallest (22.7±6.3 mL), followed by those with unilaterally patent tubes (24.3±9.3 mL). Similar volumes of contrast agent were used in the bilaterally patent group (18.9±9.2 mL) and the unilaterally patent group. A significantly less amount of contrast agent was used in individuals with bilaterally nonpatent tubes than in patients from the other two groups (P=0.0045) (Figure 3B).
We further investigated the potential of peak injection pressure for identifying obstructed fallopian tubes by performing ROC analysis, which combined peak injection pressure and agent volume. As shown in Table 3 and Figure 4, the areas under the curve (AUCs) of peak injection pressure for differentiating bilaterally patent from unilaterally patent and from bilaterally nonpatent tubes were 0.827 and 0.866, respectively. When one fallopian tube was patent, the optimal cutoff value of peak injection pressure for distinguishing nonpatent from patent tubes was 254.3 mmHg, with a sensitivity of 79.8% and a specificity of 74.3%. Similarly, when one fallopian tube was nonpatent, the optimal cutoff value was 401.3 mmHg, with a sensitivity of 90.6% and a specificity of 78.3% (Table 3).
Table 3
| Patency of fallopian tubes | AUC | Cutoff value (mmHg) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Bilaterally patent to unilaterally patent | 0.827 | 254.3 | 79.8 | 74.3 |
| Unilaterally patent to bilaterally nonpatent | 0.866 | 401.3 | 90.6 | 78.3 |
AUC, area under the curve.

Notably, the clinical significance of obstruction and partial obstruction of fallopian tubes is quite different (27). While complete tubal obstruction generally leads to infertility, partial or incomplete obstruction could result in infertility or ectopic pregnancy, with the latter being life-threatening. We further investigated the potential of peak injection pressure for identifying partial obstruction in 4D-HyCoSy. Patients were divided into six groups based on the fallopian tube patency as determined by 4D-HyCoSy (Figure S2). Similarly, there were no significant differences in age, ovarian volume, or endometrial thickness among the six groups (P>0.05) (Table S2). Peak injection pressure in the bilaterally patent group was significantly lower than that in the group with partially obstructed tubes on either side (206.8±41.4 vs. 248.4±64.3 mmHg, P<0.001). For patients with bilaterally partially obstructed tubes, the pressure was 318.8±91.8 mmHg, which was higher than that in the patent/partially obstructed group (P=0.001). Similarly, infertile patients with partially obstructed/obstructed fallopian tubes (408.6±110.2 mmHg) had a significantly higher peak injection pressure than did individuals with patent/obstructed tubes (312.1±81.8 mmHg; P<0.001) (Figure 5A). Additionally, patients with bilaterally obstructed fallopian tubes were administered significantly lower volumes of contrast agent than patients with patent/partially obstructed tubes (P=0.03), patients with patent/obstructed tubes (P<0.01) and patients with partially obstructed/obstructed tubes (P=0.044) (Figure 5B).

After establishing that the peak injection pressure in partially obstructed fallopian tubes was significantly higher than that in patent ones, we used ROC analysis to further explore the diagnostic performance of peak injection pressure for distinguishing patency from partial obstruction when a certain side was patent, partially obstructed, or obstructed. As shown in Table 4, when a certain side was patent, partially obstructed, or obstructed, the AUCs of peak injection pressure for differentiating the patency of the other fallopian tube were 0.712, 0.753, and 0.788, respectively.
Table 4
| Patency of fallopian tubes | AUC | Cutoff value (mmHg) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Group A & Group B | 0.712 | 205.5 | 70.7 | 67.5 |
| Group B & Group C | 0.753 | 303.0 | 57.1 | 82.8 |
| Group D & Group E | 0.788 | 404.3 | 65.2 | 81.7 |
Group A, bilaterally patent (patent/patent); Group B, unilaterally patent group with the other partially obstructed (patent/partially obstructed); Group C, bilaterally partially obstructed (partially obstructed/partially obstructed); Group D, unilaterally obstructed with the other patent (patent/obstructed); Group E, unilaterally obstructed with the other partially obstructed (partially obstructed/obstructed). AUC, area under the curve.
When one fallopian tube was patent, the optimal cutoff value of peak injection pressure for distinguishing partially obstructed from patent tubes was 205.5 mmHg, with a sensitivity of 70.7% and a specificity of 67.5% (Figure 6A, Table 4). Similarly, when one fallopian tube was partially obstructed, the optimal cutoff value was found to be 303.0 mmHg, with a sensitivity of 57.1% and a specificity of 82.8% (Figure 6B). For cases where only one tube was obstructed, the optimal cutoff value for distinguishing changes in the other tube’s patency from patent to partially obstructed was 404.3 mmHg, with a sensitivity of 65.2% and a specificity of 81.7% (Figure 6C).

Discussion
With the increasing incidence of tubal infertility, assessing tubal patency has become crucial in diagnosing and treating infertility. 4D-HyCoSy has emerged as an important technique for assessing tubal patency due to its relative simplicity and cost-effectiveness (12,24,28). In our study, the sensitivity and specificity of 4D-HyCoSy for diagnosing tubal obstruction were 91.1% and 95.1%, respectively, which were consistent with previous research findings (29,30). The evaluation of tubal patency using 4D-HyCoSy depends on a comprehensive evaluation of the fallopian tubes, the contrast dispersion around the ovaries, and the contrast dispersion within the pelvis, which can lead to interobserver variability (10,14,31,32). Operator-related factors have been identified as one of the causes of misdiagnosis of tubal patency that should not be ignored (33,34). Consequently, it is necessary to explore quantitative or semiquantitative indexes for the assessment of tubal patency.
We hypothesized that the peak injection pressure obtained during 4D-HyCoSy in infertile patients would be elevated when fallopian tube patency decreased and thus concluded that monitoring peak injection pressure could aid in betterer distinguishing nonpatent fallopian tubes from patent ones. Our results revealed a statistically significant association between tubal patency status and the peak injection pressure during 4D-HyCoSy. The fallopian tube is an elastic tube that remains contracted in the absence of fluid. As fluid is introduced, the pressure within the uterine cavity gradually increases, and occlusion in the fallopian tube can cause a sharp increase in pressure within the uterine cavity (35,36). However, data from a previous study concerning HSG suggested no significant relation between peak intrauterine pressure and tubal patency (19). The difference in findings may be due to differences in the HSG imaging and HyCoSy procedures, including variations in the type of contrast agent, pressure injection process, and pressure measurement process (32). Moreover, Qiang et al. (9) also demonstrated the association between tubal patency and the slope of the pressure curve during HyCoSy, indicating that peak injection pressure could be used as a promising supplement indicator (18).
In our study, the AUCs of ROC curves for distinguishing patent from nonpatent fallopian tubes were greater than 0.8 regardless of the patency status of the contralateral fallopian tube. The best diagnostic performance of peak pressure was observed when a certain fallopian tube was obstructed. However, in cases where only one side was patent, the increase in peak pressure of the other obstructed tube was not statistically significant, and the sensitivity and specificity of peak pressure were limited. As expected, the change in the patency of one fallopian tube had a more significant effect on the peak pressure when the other fallopian tube was obstructed.
The fallopian tubes play an important role in the fertilization process, including egg pick-up, sperm capacitation, sperm–egg combination, and the delivery of fertilized eggs. Partial obstruction refers to the state between patency and complete obstruction (37). A partially obstructed fallopian tube can affect all of the above processes, leading to infertility or ectopic pregnancy (38). Most of studies related to partial obstruction of the fallopian tube partly obstruction have been based on HyCoSy (34,39,40). However, the accuracy of 4D-HyCoSy in diagnosing partial obstruction appears relatively low (25). It is more challenging to differentiate patent tubes from partially obstructed tubes than from obstructed tubes, and this primarily relies on the experience of clinicians (41-44). After reviewing the scan images, we noticed instances in which fallopian tubes initially identified as being partially obstructed were later confirmed to be patent due to varying spillage from the fimbriae and periovarian diffusion with increased volume of contrast agent and injection pressure. Therefore, we conducted a preliminary assessment of peak injection pressure in distinguishing partially obstructed fallopian tubes from patent ones in the subgroup analysis.
Our results indicated found that when a certain side of the fallopian tube was patent, partially obstructed, or obstructed, the peak pressure increased when the other side was patent, partially obstructed, and obstructed, respectively. This suggests the potential of peak injection pressure for identifying tubal patency, especially in cases of partial obstruction. Interestingly, the peak injection pressure in bilaterally partially obstructed fallopian tubes was higher than that of the patent/obstructed group (P=0.044). This could be due to the contrast agent’s ability to pass through the other patent side even when one side of the fallopian tube is obstructed. In the subgroup ROC analysis, the AUCs of ROC curves for distinguishing patency from partial obstruction were greater than 0.7 and markedly so when a certain side was obstructed (0.788). The best diagnostic performance of peak pressure was observed when a certain fallopian tube was obstructed. However, when a certain side is patent, a significant increase in peak pressure in the other partially obstructed tube is not expected, limiting the sensitivity and specificity of peak pressure. The diagnostic efficiency of peak pressure also needs further confirmation when a certain side is obstructed, due to the limited number of patients in this subgroup. Taken together, our findings suggest that peak injection pressure in HyCoSy may be a promising supplementary indicator for identifying partially obstructed fallopian tubes, especially when one fallopian tube is obstructed.
This study has several limitations. First, although a total of 268 patients were enrolled, only 32 patients had with bilaterally obstructed tubes, which might have introduced statistical bias. Second, the difference in peak pressure between proximal and distal obstruction in obstructed oviducts was not analyzed. Our research team is working on exploring the potential influence of uterine fibroids or other diseases on injection pressure, which was not discussed in the current study.
Conclusions
In conclusion, the peak injection pressure during 4D-HyCoSy is associated with the status of bilateral fallopian tube patency and is a promising indicator for distinguishing obstruction from patency. Further prospectively designed studies with larger sample sizes are warranted to improve the diagnostic performance of fallopian tube patency.
Acknowledgments
We sincerely thank Dr. Xiyue Zhang (North Sichuan Medical College, Nanchong, China) and Dr. Jingyi Huang (The Affiliated Peoples Hospital of Ningbo University, Ningbo, China) for organizing the patients’ data.
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-1569/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1569/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the ethics committee of the West China Second Hospital of Sichuan University (2019.No.2). Written informed consent was obtained from each patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhou Z, Zheng D, Wu H, Li R, Xu S, Kang Y, Cao Y, Chen X, Zhu Y, Xu S, Chen ZJ, Mol BW, Qiao J. Epidemiology of infertility in China: a population-based study. BJOG 2018;125:432-41. [Crossref] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm. Role of tubal surgery in the era of assisted reproductive technology: a committee opinion. Fertil Steril 2021;115:1143-50. [Crossref] [PubMed]
- Carson SA, Kallen AN. Diagnosis and Management of Infertility: A Review. JAMA 2021;326:65-76. [Crossref] [PubMed]
- Audu BM, Massa AA, Bukar M, El-Nafaty AU, Sa'ad ST. Prevalence of utero-tubal infertility. J Obstet Gynaecol 2009;29:326-8. [Crossref] [PubMed]
- Liang S, Chen Y, Wang Q, Chen H, Cui C, Xu X, Zhang Q, Zhang C. Prevalence and associated factors of infertility among 20-49 year old women in Henan Province, China. Reprod Health 2021;18:254. [Crossref] [PubMed]
- Grigovich M, Kacharia VS, Bharwani N, Hemingway A, Mijatovic V, Rodgers SK. Evaluating Fallopian Tube Patency: What the Radiologist Needs to Know. Radiographics 2021;41:1876-18961. [Crossref] [PubMed]
- Jagannathan D, Hithaya F. Conventional and magnetic resonance hysterosalpingography in assessing tubal patency-A comparative study. Indian J Radiol Imaging 2019;29:163-7. [Crossref] [PubMed]
- Hamed HO, Shahin AY, Elsamman AM. Hysterosalpingo-contrast sonography versus radiographic hysterosalpingography in the evaluation of tubal patency. Int J Gynaecol Obstet 2009;105:215-7. [Crossref] [PubMed]
- Qiang Y, Wu Y, Cai T. Clinical Significance of Increasing Pressure Curve's Slope When Injecting Ultrasound Contrast Agent During Evaluation of Fallopian Tubal Patency. J Ultrasound Med 2021;40:2329-38. [Crossref] [PubMed]
- Chen LS, Zhu ZQ, Li J, Wang ZT, Qiang Y, Hu XY, Zhang MM, Wang ZQ. Hysterosalpingo-contrast-sonography vs. magnetic resonance-hysterosalpingography for diagnosing fallopian tubal patency: A systematic review and meta-analysis. Eur J Radiol 2020;125:108891. [Crossref] [PubMed]
- Török P, Molnár S, Herman T, Jashanjeet S, Lampé R, Riemma G, Vitale SG. Fallopian tubal obstruction is associated with increased pain experienced during office hysteroscopy: a retrospective study. Updates Surg 2020;72:213-8. [Crossref] [PubMed]
- He Y, Geng Q, Liu H, Han X. First experience using 4-dimensional hysterosalpingo-contrast sonography with SonoVue for assessing fallopian tube patency. J Ultrasound Med 2013;32:1233-43. [Crossref] [PubMed]
- Infertility Workup for the Women's Health Specialist. ACOG Committee Opinion Summary, Number 781. Obstet Gynecol 2019;133:1294-5. [Crossref] [PubMed]
- Chen F, Quan J, Huang P, You X. Hysterosalpingo-Contrast Sonography With Four-Dimensional Technique for Screening Fallopian Tubal Patency: Let's Make an Exploration. J Minim Invasive Gynecol 2017;24:407-14. [Crossref] [PubMed]
- Salata I, Gottwald L, Sobkiewicz S. Comparison of assessing the patency of the Fallopian tubes during laparoscopy and during hysterosalpingography on television in infertile women with endometriosis. Ginekol Pol 2003;74:1014-7.
- Zhang N, Liu Y, He Y, Shi J, Zhou M, Liu H. Transvaginal four-dimensional hysterosalpingo-contrast sonography: Pain perception and factors influencing pain severity. J Obstet Gynaecol Res 2021;47:302-10. [Crossref] [PubMed]
- Ma Y, Du L, Li F, Zhu Z. Use of atropine in four-dimensional hysterosalpingo-contrast sonography: Does it suppress pain during infertility examination? Clin Exp Pharmacol Physiol 2018;45:1334-40. [Crossref] [PubMed]
- Patil E, Thurmond A, Hart K, Seguin J, Edelman A, Jensen JT. Intrauterine fluid instillation to confirm tubal occlusion after transcervical permanent contraception: A pilot study. Contraception 2020;101:40-5. [Crossref] [PubMed]
- Patil E, Thurmond A, Edelman A, Fu R, Lambert W, Seguin J, Jensen JT. Pressure dynamics in the non-gravid uterus: intrauterine pressure cannot confirm tubal occlusion after non-surgical permanent contraception. Contraception 2017;96:330-5. [Crossref] [PubMed]
- Expert Panel on Women’s Imaging. Wall DJ, Reinhold C, Akin EA, Ascher SM, Brook OR, Dassel M, Henrichsen TL, Learman LA, Maturen KE, Patlas MN, Robbins JB, Sadowski EA, Saphier C, Uyeda JW, Glanc P. ACR Appropriateness Criteria® Female Infertility. J Am Coll Radiol 2020;17:S113-24. [Crossref] [PubMed]
- Lin Y, Lin L, Cheng M, Jin L, Du L, Han T, Xu L, Yu ACH, Qin P. Effect of acoustic parameters on the cavitation behavior of SonoVue microbubbles induced by pulsed ultrasound. Ultrason Sonochem 2017;35:176-84. [Crossref] [PubMed]
- Shi J, Li S, Wu H, He Y, Yi W, Xu J, Liu H, Guan Y. The Influencing Factors of Venous Intravasation During Transvaginal Four-dimensional Hysterosalpingo-contrast Sonography With SonoVue. Ultrasound Med Biol 2019;45:2273-80. [Crossref] [PubMed]
- The Team of Multi-Center Clinical Research Study of. “One-Stop” Sonography System for Female Infertility. Expert consensus on "one-stop" hysterosalpingography for infertility in women. Chinese Journal of Medical Ultrasound 2020;17:108-14. (Electronic Edition).
- He Y, Ma X, Xu J, Li S, Wu H, Liu Q, Kong L, Luo J, Liu H. Comparison of Assessment Methods for Fallopian Tubal Patency and Peritubal Adhesion Between Transvaginal 4-Dimensional Hysterosalpingo-Contrast Sonography and Laparoscopic Chromopertubation. J Ultrasound Med 2017;36:547-56. [Crossref] [PubMed]
- Wang W, Zhou Q, Gong Y, Li Y, Huang Y, Chen Z. Assessment of Fallopian Tube Fimbria Patency With 4-Dimensional Hysterosalpingo-Contrast Sonography in Infertile Women. J Ultrasound Med 2017;36:2061-9. [Crossref] [PubMed]
- Mayrhofer D, Parry JP, Hager M, Beitl K, Kurz C, Ott J. Are the Stage and the Incidental Finding of Endometriosis Associated with Fallopian Tube Occlusion? A Retrospective Cohort Study on Laparoscopic Chromopertubation in Infertile Women. J Clin Med 2022;11:3750. [Crossref] [PubMed]
- Zhang Y, Wang Q, Gao CY, Tian HJ, He WJ, Zhang X, Xiong X. Evaluation of the safety and effectiveness of tubal inflammatory drugs in patients with incomplete tubal obstruction after four-dimensional hysterosalpingo-contrast-sonography examination. BMC Pregnancy Childbirth 2022;22:395. [Crossref] [PubMed]
- Maheux-Lacroix S, Boutin A, Moore L, Bergeron ME, Bujold E, Laberge P, Lemyre M, Dodin S. Hysterosalpingosonography for diagnosing tubal occlusion in subfertile women: a systematic review with meta-analysis. Hum Reprod 2014;29:953-63. [Crossref] [PubMed]
- Wang Y, Qian L. Three- or four-dimensional hysterosalpingo contrast sonography for diagnosing tubal patency in infertile females: a systematic review with meta-analysis. Br J Radiol 2016;89:20151013. [Crossref] [PubMed]
- Qu E, Zhang M, Ju J, Chen Y, Lin X, Zhang X. Is Hysterosalpingo-Contrast Sonography (HyCoSy) Using Sulfur Hexafluoride Microbubbles (SonoVue) Sufficient for the Assessment of Fallopian Tube Patency? A Systematic Review and Meta-Analysis. J Ultrasound Med 2023;42:7-15. [Crossref] [PubMed]
- Zhao X, Fei L, Gu P, Xu D, Zhang B, Yang Y. A model established for predicting natural pregnancy possibility based on the imaging characteristics of 4-dimensional hysterosalpingo-contrast sonography. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2022;47:1600-7. [Crossref] [PubMed]
- Kong D, Dong X, Wang Z, Zhang L, Shao X, Qi Y. Four-dimensional hysterosalpingo-contrast sonography with auxiliary hydrogen peroxide examination for the diagnosis of fallopian tube patency following interventional treatment of ovarian ectopic cysts. Arch Gynecol Obstet 2017;295:519-26. [Crossref] [PubMed]
- Shah SM, Towobola OA, Masihleho M. Diagnosis of fallopian tube patency. East Afr Med J 2005;82:457-62. [Crossref] [PubMed]
- Liang N, Wu QQ, Li JH, Gao FY, Sun FL, Guo CX. Causes of misdiagnosis in assessing tubal patency by transvaginal real-time three-dimensional hysterosalpingo-contrast sonography. Rev Assoc Med Bras (1992) 2019;65:1055-60. [Crossref] [PubMed]
- Thurmond AS, Machan LS, Maubon AJ, Rouanet JP, Hovsepian DM, Moore A, Zagoria RJ, Dickey KW, Bass JC. A review of selective salpingography and fallopian tube catheterization. Radiographics 2000;20:1759-68. [Crossref] [PubMed]
- Patil E, Thurmond A. The history and current status of fallopian tube pressures - developing alternate methods for confirmation of tubal occlusion. Contraception 2015;92:124-7. [Crossref] [PubMed]
- Hunter RH. Human sperm reservoirs and Fallopian tube function: a rôle for the intra-mural portion? Acta Obstet Gynecol Scand 1995;74:677-81. [Crossref] [PubMed]
- Xu Z, Wang Y, Sun J, Chen S, Yan Z, Lin C, Shu J. Evaluation of tubal patency by hysterosalpingo-contrast Sonography (HyCoSy): Controversies, dilemmas and considerations. Heliyon 2023;9:e17461. [Crossref] [PubMed]
- Zhou L, Zhang X, Chen X, Liao L, Pan R, Zhou N, Di N. Value of three-dimensional hysterosalpingo-contrast sonography with SonoVue in the assessment of tubal patency. Ultrasound Obstet Gynecol 2012;40:93-8. [Crossref] [PubMed]
- Wang J, Li J, Yu L, Han S, Shen X, Jia X. Application of 3D-HyCoSy in the diagnosis of oviduct obstruction. Exp Ther Med 2017;13:966-70. [Crossref] [PubMed]
- Pei R. Comparison of Effectiveness as well as Advantages and Disadvantages of Different Dimensions of Hysterosalpingo-Contrast Sonography for Diagnosis of Lesions Associated with Female Infertility. Comput Math Methods Med 2022;2022:7508880. [Crossref] [PubMed]
- Bisogni FA, Galanti F, Riccio S, Yacoub V, Carletti V, Morgani C, Grilli D, Schiavi MC, Rago R. 4D-HyCoSy performed in a reproductive center: retrospective analysis of pain perception, complications and spontaneous pregnancy rate after the technique. Eur Rev Med Pharmacol Sci 2021;25:7468-75. [Crossref] [PubMed]
- Gu P, Yang X, Zhao X, Xu D. The value of transvaginal 4-dimensional hysterosalpingo-contrast sonography in predicting the necessity of assisted reproductive technology for women with tubal factor infertility. Quant Imaging Med Surg 2021;11:3698-714. [Crossref] [PubMed]
- Liu Y, Zhang N, He Y, Shi J, Zhou M, Xu J, Liu H. Spontaneous conception outcome in infertile women after four-dimensional hysterosalpingo-contrast-sonography. BMC Pregnancy Childbirth 2020;20:638. [Crossref] [PubMed]


