
Contrast-enhanced computed tomography of retromandibular vein position and course patterns relative to the mandible during sagittal split ramus osteotomy
Introduction
Surgical correction of either congenic or acquired jaw deformities still are associated with certain risks, although recent developments such as ultrasonic cutting devices. As such, orthognathic surgery is a standardized worldwide procedure in oral and maxillofacial surgery. Sagittal split ramus osteotomy (SSRO) is the most commonly performed and established surgical procedure. As well, SSRO represents the most common type of mandibular osteotomy performed in our hospital (1). Intraoperative complications, such as major bleeding, lower lip paresthesia, lingual nerve paresthesia and unfavorable fractures are frequently encountered (2-5). Thorough preoperative evaluation of surgical risks is important to reduce surgical time and intraoperative blood loss and to achieve favorable outcomes. The incidence of unfavorable fractures and inferior alveolar nerve injury can be decreased by preoperative computed tomography (CT) to evaluate bone tissue and morphology. On the other hand, the risk of intraoperative bleeding caused by jeopardizing one of the vessels running through the soft tissue with unpredictable course can only be predicted preoperatively using contrast-enhanced computed tomography (CECT). In addition, the courses of various blood vessels in patients with jaw deformities differ from those in healthy individuals (6,7).
In our previous study (8), we determined the retromandibular vein (RMV) position and course patterns relative to the posterior border of the ramus using 15 cadavers (15 sides). We identified three-course patterns in the lateral view and five in the posterior view (8).
Therefore, herein, we aimed to investigate the location and pattern of RMV courses in patients with defined jaw deformities using CECT.
Methods
Study population
From October 2018 to October 2019, twenty patients aged 17–45 years were included. Skeletal classification was performed using cephalometric analysis. Patients with a cleft palate or craniofacial abnormalities were excluded. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Tokyo Dental College (Nos. 794 and 844). Written informed consent was obtained from patients or patient’s parents for the publication of this study and any accompanying images.
RMV course categorization and measurement parameters
CT scans (SOMATOM Definition AS, Siemens, Forchheim, Germany) were obtained one month before surgery, and the CT images were formatted as Digital Imaging and Communications in Medicine (DICOM) data. The CT DICOM and digital impression data were transferred to Minimics (Materialize, Leuven, Belgium) and segmented.
A baseline was created based on 5 mm above the mandibular ligula.
The types were classified based on the positional relationship between the RMV and the posterior border of the ramus on the lateral view as follows: Type A, RMV posterior to the posterior border of the ramus; Type B, RMV adjoining the posterior border of the ramus; and Type C, RMV anterior to the posterior border of the ramus (Figure 1A).
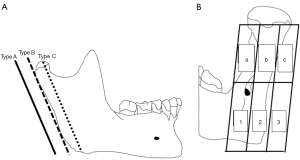
In the posterior view, the images were divided into three buccolingual sections comprising the posterior border and the buccal and lingual aspects of the ramus. These were then divided into superior and inferior sections at the height of the lingula. Based on these sections, the RMV course patterns were classified into one of nine possible categories (Figure 1B) (8). Differences in the running patterns between the left and right sides and skeletal classifications were also investigated.
Statistical analysis
Chi-square tests were compared using binomial logistic regression analysis. Differences were considered statistically significant at P<0.05. All data were processed using the IBM SPSS software package ver. 23 (SPSS ver. 23).
Results
Participant characteristics
Participant characteristics are presented in Table 1. Twenty patients aged 17–45 years (mean age: 26.0 years) were included.
Table 1
| Case No. | Age (years) | Sex | Diagnosis | Left side | Right side | |||
|---|---|---|---|---|---|---|---|---|
| Type | Pattern | Type | Pattern | |||||
| 1 | 24 | F | Mandibular protrusion + maxillary retrusion | A | IV | A | II | |
| 2 | 27 | F | Mandibular protrusion + maxillary retrusion | A | II | A | III | |
| 3 | 24 | F | Mandibular protrusion + maxillary retrusion | A | II | A | IV | |
| 4 | 25 | F | Mandibular protrusion + maxillary retrusion | A | IV | A | IV | |
| 5 | 20 | F | Mandibular protrusion + maxillary retrusion | A | V | B | V | |
| 6 | 26 | F | Mandibular protrusion + maxillary retrusion | B | III | B | III | |
| 7 | 30 | F | Mandibular protrusion + maxillary retrusion | C | III | A | II | |
| 8 | 21 | M | Mandibular protrusion + maxillary retrusion | B | IV | B | IV | |
| 9 | 23 | F | Mandibular retrusion + maxillary protrusion | A | III | A | III | |
| 10 | 20 | F | Mandibular retrusion + maxillary protrusion | B | V | A | II | |
| 11 | 19 | F | Mandibular retrusion + maxillary protrusion | C | I | B | II | |
| 12 | 32 | M | Mandibular retrusion + maxillary protrusion | B | IV | A | IV | |
| 13 | 28 | F | Mandibular protrusion + maxillo-mandibular asymmetry + open bite | A | II | A | II | |
| 14 | 24 | F | Mandibular protrusion + maxillo-mandibular asymmetry + open bite | A | V | A | III | |
| 15 | 19 | F | Mandibular protrusion + maxillary retrusion + maxillo-mandibular asymmetry | C | II | A | III | |
| 16 | 17 | F | Mandibular retrusion + maxillary protrusion + open bite | A | III | A | III | |
| 17 | 19 | F | Mandibular retrusion + maxillary protrusion + open bite | B | I | B | I | |
| 18 | 26 | F | Maxillo-mandibular asymmetry | B | V | B | V | |
| 19 | 17 | F | Maxillo-mandibular asymmetry + cross bite | A | II | A | II | |
| 20 | 45 | F | Maxillo-mandibular asymmetry + open bite | A | III | A | III | |
RMV, retromandibular vein; F, female; M, male.
Course patterns
This classification of course patterns is the same as our previously reported classification of the posterior and lateral aspects of the ramus.
Course patterns lateral view (Table 1, Figure 2)
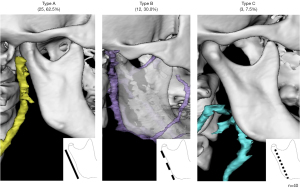
A Type A pattern (RMV positioned posterior to the posterior border of the ramus) was observed on 25 sides (62.5%), Type B (RMV adjoining the posterior border of the ramus) on 12 sides (30.0%), and Type C (RMV positioned anterior to the posterior border of the ramus) on three sides (7.5%). There were 14 cases (70.0%) of Type in which the left and right sides were the same.
Course patterns posterior view (Figure 3)

Dividing the posterior view images into three buccolingual sections comprising the posterior border and buccal and lingual aspects of the ramus, which were then divided into upper and lower sections at the height of the lingula, and classifying course patterns into one of nine possible categories, no course patterns included Block 3—inferior to the lingula and lateral to the posterior border of the ramus—regardless of the position of the course superior to the lingula. Five course patterns were identified.
- Pattern I (a-1): rectilinear course running medial to the posterior border of the ramus (n=3; 7.5%).
- Pattern II (b-1): diagonal course running medially from immediately posterior to the posterior border of the ramus (n=11; 27.5%).
- Pattern III (b-2): rectilinear course running immediately posterior to the posterior border of the ramus (n=12; 30.0%).
- Pattern IV (c-1): diagonal course running from lateral to medial in relation to the posterior border of the ramus (n=8; 20.0%).
- Pattern V (c-2): diagonal course running from lateral to immediately posterior in relation to the posterior border of the ramus (n=6; 15.0%).
In the no-course pattern, the RMV inferior to the lingula was lateral to its position and superior to that of the lingula. The bilateral type was identical in all 12 cases (60.0%).
No significant differences were observed between men and women in any of the data items, including skeletal classification.
The most common combinations of type and pattern were Type A/Pattern II and Type A/Pattern on nine sides each (22.5%). Type B/Pattern II bleeding that runs in a straight line bordering the posterior margin of the ramus requires the most attention during surgery. Both type and pattern matched in 10 cases (50%), type alone matched in 14 cases (70%), and pattern alone matched in 12 cases (60%) in the lateral and posterior views. Complete discordance was observed in 4 cases (20%). Half of the patients showed a discrepancy in the running pattern between the left and right sides. In mandibular protrusion, type and pattern were completely matched in 4 of 11 cases (36.4%), whereas only type was matched in 9 of 11 cases (81.8%). In the case of mandibular retrusion, the type and pattern matched perfectly in 3 of the 6 cases (50.0%), whereas only the type matched in 3 of the 6 cases (50.0%). The degree of accordance was higher in mandibular protrusion cases. No statistically significant relationship was found between the type of jaw deformity and the RMV course.
Discussion
Orthognathic surgery is widely recognized for its efficacy in oral and maxillofacial surgery in Japan. SSRO is the most commonly performed type of orthognathic surgery (1). The first surgical approach for SSRO was reported by Trauner and Obwegeser (9) in 1957. Piñeiro-Aguilar et al. (10) reported a correlation between operation time and intraoperative blood loss in SSRO. Thorough preoperative evaluation of surgical risks is important to reduce surgical time and intraoperative blood loss and to improved surgical safety. In a previous study, we investigated the location and course patterns of RMV in cadavers (8). However, in cadavers, deviations may occur due to the method and circumstances of fixation. In addition, many of the cadavers were too old and had missing teeth to enable skeletal classification. Therefore, in this study, we used CECT in patients with jaw deformities to identify the anatomy of RMV. The running patterns in both lateral and posterior views were similar in patients with jaw deformities.
In a previous study we described the RMV position and course patterns relative to the posterior border of the ramus using cadavers to facilitate the preoperative evaluation of bleeding risk in SSRO (8).
RMV course patterns have also been reported by other authors; however, most of these studies focused on its position relative to the facial nerve during parotid gland tumor resection (11,12). To date, no study has investigated the running pattern and position of the RMV in patients with jaw deformities. Focusing on orthognathic surgery, the present study examined the RMV course patterns lateral and posterior to the ramus using CECT in patients with jaw deformities. Based on measurements of the distance between the RMV and posterior border of the ramus, the levels of risk for intraoperative bleeding were also classified. In a previous study (8), we observed the same types and patterns of RMV. Type A was the most common type in cadavers, and the same was observed in patients with jaw deformities. Nevertheless, Type B was more common in our patients with jaw deformities than in our cadaver study. Pattern I, which was more common in cadavers, was less common in patients with jaw deformities, and the percentages of Patterns II and III were higher in cadavers. These results indicated that Type A-Pattern I was more common in cadavers, whereas Type A-Pattern II, followed by Type A-Pattern III, was more common in patients with jaw deformities, indicating a difference. The courses of various blood vessels in patients with jaw deformities differ from those in healthy individuals (6,7).
The RMVs below the mandibular fontanel were positioned laterally above the mandibular fontanel. Ten patients (50.0%) had the same position and running pattern in both lateral and posterior views on the left and right sides. Lohn et al. and Koh et al. reported that the facial arteries showed a discordant pattern on the left and right sides in 47% and 45.5% of cases, respectively (13,14). In the present study, half of the patients exhibited discordant running patterns of the RMV. To date, no studies have reported left-right differences of the RMV using the mandible as a reference point.
The present study focused on orthognathic surgery and examined the RMV course patterns to the ramus. On 12 sides (30%), the RMV was adjacent, whereas in others, it was positioned anterior to the posterior border of the ramus. If the RMV is damaged during SSRO, it is difficult to stop the bleeding. Pressure hemostasis is also ineffective in such situations. This demonstrates the need for a careful clearly subperiosteal approach before performing the horizontal cut at the medial aspect of the ramus during SSRO.
As in our previous cadaver investigation (8), no participant of our study exhibited a pattern involving the RMV running lateral to the ramus inferior to the lingula, which is the position of the lateral cut according to Traunerand Obwegeser’s method (9). These anomalies pose a potential risk for intraoperative bleeding. Furthermore, the high incidence of vascular variations in jaw deformity patients (6,7) necessitates extra care during mandibula osteotomy, regardless of the particular approach, such as Trauner and Obweger’s or Obwegeser’s methods.
Additionally, in cases of severe mandibular prognathism needing a long medial cut during osteotomy, the distal bone segment may be positioned posterior to the posterior border of the ramus during mandibular fixation. There were differences in both the types and patterns between the left and right sides observed for the first time in this study, and half of the cases were discordant. This indicates that even if the problem is confined to one side, the other side may exhibit a greater risk of bleeding. These findings indicate the need to preoperatively consider whether a short lingual split should be created for the medial cut in patients with a large posterior displacement.
Orthognathic surgery is a type of plastic surgery that does not usually result in serious complications. However, there are many variations in the blood vessels traveling within soft tissues, and care must be taken throughout the entire surgical process. During SSRO, the periosteum should be carefully dissected for preservation and firmly protected with a Prognathie-hook. However, in cases with large posterior mandibular movement, the choice of medial osteotomy and post-sagittal division treatment postoperative treatment should be carefully considered. The classification of these RMV types and patterns would be useful for intraoral vertical ramus osteotomy, tumor surgery, open reduction, and internal fixation.
Although the number of cases in this study was low, this is the first report on RMV running patterns and positions in patients with jaw deformities. In the future, we will increase the number of cases; investigate the relationship between skeletal classification, mandibular branch morphology, and RMV running pattern and position, and identify cases requiring urgent attention during surgery.
Conclusions
We identified three types of positional relationship between the RMV and the posterior border of the ramus and five RMV course patterns using CECT in jaw deformity patients in this study. Although CECT must be taken preoperatively, the findings suggest it may be possible to predict correlations with intraoperative bleeding risk. Furthermore, additional study of a larger patient series should be conducted to validate these results.
Acknowledgments
We would like to thank the members of the Department of Oral Pathobiological Science and Surgery, Tokyo Dental College, for their cooperation. And we would like to thank Editage (www.editage.jp) for English language editing.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1301/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Tokyo Dental College (Nos. 794 and 844). Written informed consent was obtained from patients or patients’ parents for the publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDeri
References
- Hamada Y, Sugahara K, Yoshida S, Watanabe A, Bessho H, Kasahara K, Takano M, Saito C, Shibahara T, Katakura A. A 27-year retrospective clinical analysis of 2640 orthognathic surgery cases in the Tokyo Dental College. J Oral Maxillofac Surg Med Pathol 2019;31:305-10.
- Bays RA, Bouloux GF. Complications of orthognathic surgery. Oral Maxillofac Surg Clin North Am 2003;15:229-42. [Crossref] [PubMed]
- Dos Santos VDB, Queiroz SIML, da Silva AC, Silva S, da Silva JSP, Fernandes GVO, Germano AR. Evaluation of the Anatomic Position of the Mandibular Canal Regarding to the Segments of the Mandibular Sagittal Split Ramus Osteotomy to Diminish the Possibility of Injuries: a Pilot Study. J Oral Maxillofac Res 2022;13:e2. [Crossref] [PubMed]
- Panula K, Finne K, Oikarinen K. Incidence of complications and problems related to orthognathic surgery: a review of 655 patients. J Oral Maxillofac Surg 2001;59:1128-36; discussion 1137. [Crossref] [PubMed]
- Patel PK, Morris DE, Gassman A. Complications of orthognathic surgery. J Craniofac Surg 2007;18:975-85; Quiz 986-8. [Crossref] [PubMed]
- Lanigan DT, Hey JH, West RA. Major vascular complications of orthognathic surgery: false aneurysms and arteriovenous fistulas following orthognathic surgery. J Oral Maxillofac Surg 1991;49:571-7. [Crossref] [PubMed]
- Jackson IT, Jack CR, Aycock B, Dubin B, Irons GB. The management of intraosseous arteriovenous malformations in the head and neck area. Plast Reconstr Surg 1989;84:47-54. [Crossref] [PubMed]
- Sugahara K, Matsunaga S, Yamamoto M, Noguchi T, Morita S, Koyachi M, Koyama Y, Koyama T, Kasahara N, Abe S, Katakura A. Retromandibular vein position and course patterns in relation to mandible: anatomical morphologies requiring particular vigilance during sagittal split ramus osteotomy. Anat Cell Biol 2020;53:444-50. [Crossref] [PubMed]
- TRAUNER R. OBWEGESER H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol 1957;10:677-89. contd. [Crossref] [PubMed]
- Piñeiro-Aguilar A, Somoza-Martín M, Gandara-Rey JM, García-García A. Blood loss in orthognathic surgery: a systematic review. J Oral Maxillofac Surg 2011;69:885-92. [Crossref] [PubMed]
- Touré G, Vacher C. Relations of the facial nerve with the retromandibular vein: anatomic study of 132 parotid glands. Surg Radiol Anat 2010;32:957-61. [Crossref] [PubMed]
- Babademez MA, Acar B, Gunbey E, Karabulut H, Karasen RM. Anomalous relationship of the retromandibular vein to the facial nerve as a potential risk factor for facial nerve injury during parotidectomy. J Craniofac Surg 2010;21:801-2. [Crossref] [PubMed]
- Lohn JW, Penn JW, Norton J, Butler PE. The course and variation of the facial artery and vein: implications for facial transplantation and facial surgery. Ann Plast Surg 2011;67:184-8. [Crossref] [PubMed]
- Koh KS, Kim HJ, Oh CS, Chung IH. Branching patterns and symmetry of the course of the facial artery in Koreans. Int J Oral Maxillofac Surg 2003;32:414-8. [Crossref] [PubMed]


