
Quality assessment of transperineal ultrasound in Chinese tertiary medical centers: a multicenter study
Introduction
Pelvic floor disorders (PFDs) such as pelvic organ prolapse (POP), urinary dysfunction (UD), and defecatory dysfunction (DD) impact daily activities and quality of life, affecting approximately 23.7% of women worldwide, with a high rate (11%) (1-3) of these women undergoing surgical procedures. The high reoperation rate (9.7–29%) (4-8) and low patient satisfaction rate (58.3%) (1,3,4,8-10) after surgery are particularly distressing. Therefore, the accurate assessment of PFDs is of the utmost importance for diagnosis and treatment (1,3,4). In China, due to the large population and the weakness of community health care, treatment for PFDs has typically centered on postpartum screening and prevention, including early exercise and timely rehabilitation (3,4,9).
In recent years, transperineal ultrasound (TPUS) has been increasingly applied to the assessment of pelvic floor dysfunction owing to its ability to provide unique visualization of multiple pelvic compartments (11,12). In addition to its noninvasive and real-time operation, TPUS has also shown advantages in the diagnosis of levator ani avulsion (11-14), the assessment of pelvic floor implant materials (15), and postpartum screening (16-18). The American College of Radiology (ACR) Appropriateness Criteria also state that it is one of the most promising examination methods for PFDs (1). Although most of the relevant literature indicates that TPUS is highly reproducible, with interobserver interclass correlation coefficients (ICCs) ranging from 0.75–0.92 (19-24), a few studies have reported only moderate repeatability, with an interobserver ICC of 0.61 (19-24). This discrepancy in results may be attributed to individual operator experience.
It is well-known that before a method examination can be applied to a broader scale, its quality, including its capacity for standardized management and its ability to detect abnormality, needs to be evaluated (25). As a new approach, related reports of standardized management for TPUS are scarce. Following prompting from researchers for the implementation quality assessment of ultrasonic procedures, accumulating evidence has shown that quality assessment not only improves image quality but is also valuable in the training process (26). However, it remains to be determined whether these benefits can also be achieved from the standardized management of TPUS.
This multicenter study was therefore initiated by the National Ultrasound Quality Control Center (NUQCC) with the aim of surveying the quality of postpartum TPUS in China. Continuous cases of TPUS from tertiary medical centers were collected, and the status of standardization was summarized, with an ultimate goal of providing evidence for standardized postpartum TPUS training and application.
Methods
Study design
This multicenter study was conducted at 44 tertiary medical centers (where at least 30 TPUS procedures had been completed before the initiation of this study) in China between September 2020 and September 2021. The initiating clinical center provided standardized operation training before the study in accordance with the criteria set by the ACR and International Urogynecological Association (IUGA) (11,12). All the investigators (a senior sonographer with at least 2 years of TPUS experience) involved were requested to participate in the training course for at least 3 days and were thus deemed qualified. The participating centers were required to collect at least 20 TPUS examinations and submit them to the NUQCC (www.nuqcc.cn) in a continuous manner.
This study was approved by the Human Research Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University (No. [2020] 02-156-01). All participating hospitals were informed of the study details before agreeing to participate. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013), and the need for informed consent was waived due to the retrospective nature of the study.
Study population
This multicenter study recruited data from women who had their routine pelvic floor examination within 1 year postpartum. In addition to the standard TPUS examination, they underwent a standardized clinical interview (11,12). The exclusion criteria for this study were as follows: (I) women younger than 18 years old, (II) incomplete images, and (III) women who refused to participate in this study.
Transperineal ultrasound
All TPUS examinations were performed using a Mindray ultrasound device (Resona 7T, 8T, or 9T, Mindray Medical International Ltd.) with a 4 to 8-MHz curved array volume transducer and an acquisition angle of 85°. The examination was carried out at the dorsal lithotomy position after bladder emptying and defecation if possible. According to the recommendation of criterion set by the ACR and IUGA, the examination in this study consisted of 5 parts: (I) 2-dimensional (2D) images of the midsagittal section at rest (2D-r), (II) 2D images of the midsagittal section at strain (2D-s), (III) 4-dimensional (4D) images of the levator ani hiatus (LAH), (IV) 4D images of the levator ani muscle (LAM), and (V) 4D images of the anal sphincter (AS). The Valsalva maneuver was performed for at least 6 s without levator coactivation. Imaging of the LAM and AS were performed during pelvic floor muscle contraction.
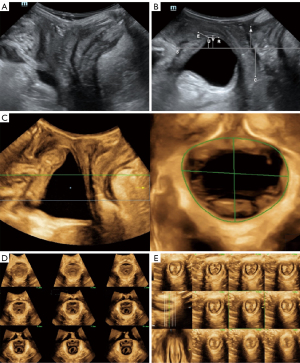
Postprocessing of images included measurements in 2D images and reconstruction in 4D images, as shown in Figure 1.

Two-dimensional images were taken at the midsagittal section of the pelvic floor at rest and at strain. A reference line for TPUS was defined as a horizontal line positioned through the posteroinferior margin of the symphysis pubis (SP). Obtaining 2D-r images requires measurement of the distance from the bladder neck to the symphysis (BSD-r), retrovesical angle (RVA), and tilt angle (TA); meanwhile, the 2D-s image requires measurement of the RVA, TA, and the descent of organs including of the bladder neck (BSD-s), cystocele, uterus, intestine, and rectal ampulla, at maximum Valsalva state. Additionally, bladder neck descent distance (BSD) and urethral rotation angle (ROA) should also be calculated, and the presence of periurethral lesions should be determined
Four-dimensional image reconstruction involves LAH, LAM, and AS. The reconstruction of LAH images requires placing the region of interest (ROI) box (width less than 2 cm) on the plane of minimal hiatal dimensions at maximum Valsalva, and the area of LAH requires measurement of the area enclosed by the inner edge of the LAM. Tomographic ultrasound imaging (TUI) is a tool for observing both the LAM and AS. Sampling lines are the key to TUI. The placement of the sampling line needs to set the starting point, stopping point, and layer spacing of the interest area so as to display the area of interest completely through the layer cut. For the TUI of LAM, the interslice interval should be set at 2.5 mm for 8 slices, and the SP in the 3 central slices (slice 4, 5, 6) should appear during the opening, closing and closed states. The 3 planes of AS should present the orthogonal views, for example, with the sphincter on horizontal on the B plane (midsagittal view of the anal canal) and vertical on the C plane (axial view of the anal canal). The TUI of AS should include 8 slices, with slice 1 being located below the internal anal sphincter (IAS) and slice 8 being located above the external anal sphincter (EAS).
Data submission
General information of patients, such as patient ID, age, body mass index (BMI), history of gestation, and symptoms of PFD, were required to be submitted. All 5 TPUS parts were required to be submitted in the format of 6 images and 4 videos with the following specifications: (I) 2D-r image without measurements, (II) 2D-r image with measurement, (III) 2D-s dynamic video under Valsalva, (IV) 2D-s image with measurements under maximum Valsalva, (V) 4D-s dynamic video under Valsalva, (VI) 4D-s reconstructed image with measurements under maximum Valsalva, (VII) 4D-LAM dynamic video during contraction, (VIII) 4D-LAM reconstructed image, (IX) 4D-AS dynamic video during contraction, and (X) 4D-AS reconstructed image.
Centers with fewer than 100 cases submitted were required to submit whatever they had until the end of the study (September 2021), while centers with more than 100 cases submitted could freely choose to either continue or stop submitting.
Quality assessment
Quality assessment was performed by 2 experts with more than 5 years of experience in TPUS (ZM and WJW). The uploaded cases were assigned to 2 experts at a 1:1 ratio for assessment. The experts logged into the NUQCC website (www.nuqcc.cn) to assess whether the 5 parts (2D-r, 2D-s, LAH, LAM, AS) of the uploaded cases were qualified. The criteria of qualified images and possible reasons for nonqualification were defined via mutual discussion of the 2 experts prior the study and included preparation during examination (less residual urine and ampulla gas, Valsalva duration of more than or equal to 6 seconds, lack of levator coactivation, etc.) and postprocessing involving 2D image measurement (key structure identification and measure cursor placement) and 4D image reconstruction (image rotation and sampling line placement, etc.). For cases in which assessment results were uncertain, the 2 experts discussed the case and made a final decision via consensus. When the experts reviewed the images, they needed to determine whether the images of each part were qualified, and then checked the reasons for nonqualification. Both experts involved were blind to organization and the uploader of the uploaded images.
To ensure the reliability of the assessment results, the intra- and interobserver reliability of the 2 experts (ZM and WJW) were assessed with a sample size of 40 initial participants via subjective evaluation.
Statistical analysis
The SPSS version 22 (IBM Corp.) was used for statistical analysis of the data. Continuous variables are presented as mean ± SD, and classification variables are presented as frequencies and percentages. The t test or Mann-Whitney test was used for comparisons between different groups for continuous variables, while the chi-squared test was used for the frequency distribution. All statistical tests were 2 sided, and P values <0.05 indicated statistically significant differences.
The intraobserver and interobserver reliability was assessed with Cohen’s kappa and its 95% confidence interval (CI).
Results
Patients
This study initially recruited 44 centers. However, 13 hospitals were later excluded because they had submitted fewer than 20 cases. In the end, 31 hospitals were enrolled, distributed across 20 provinces in China, with the number of cases ranging from 25 to 232.
As shown in flowchart in Figure 2, 2,259 cases were submitted from these 31 hospitals, with 8 cases being excluded due to incomplete images, bringing the total enrolment case number to 2,251 (mean age 30.93±4.16 years; range, 20–49 years). Table 1 shows the baseline characteristic of the enrolled participants.

Table 1
| Variable | Qualified | Nonqualified | P value |
|---|---|---|---|
| No. of patients | 1,201 | 1,050 | |
| Age (years) | 30.83±4.01 | 31.05±4.32 | 0.202 |
| Body mass index (kg/m2) | 23.30±3.34 | 23.29±3.23 | 0.917 |
| Parity | 1.36±0.51 | 1.39±0.53 | 0.095 |
| Delivery mode, n (%) | |||
| Vaginal | 815 (67.86) | 735 (70.00) | 0.274 |
| Vacuum | 17 (1.42) | 12 (1.14) | 0.567 |
| Forceps | 6 (0.50) | 14 (1.33) | 0.035 |
| Cesarean | 363 (30.22) | 289 (27.53) | 0.159 |
| Symptoms of PFD | |||
| Asymptomatic | 803 (66.86) | 635 (60.48) | 0.002 |
| Urinary incontinence | 293 (24.21) | 307 (29.24) | 0.001 |
| Constipation | 98 (8.16) | 78 (7.43) | 0.519 |
| Organ prolapse | 44 (3.66) | 89 (8.48) | <0.001 |
| Painful intercourse | 16 (1.33) | 17 (1.62) | 0.572 |
| Dysuria | 9 (0.74) | 3 (0.29) | 0.130 |
| Levator anal muscle avulsion | 13 (1.08) | 19 (1.81) | 0.146 |
| Anal sphincter injury | 5 (0.42) | 9 (0.86) | 0.184 |
Data are expressed as mean ± standard deviation or number (percentage). PFD, pelvic floor dysfunction.
Regarding the mode of delivery, there were 815 (67.86%) cases of vaginal delivery, 17 (1.42%) cases of vacuum delivery, 6 (0.50%) cases of forceps delivery, and 363 (30.22%) cases of cesarean delivery in the qualified group. Meanwhile, there were 735 (70.00%) cases of vaginal delivery, 12 (1.14%) cases of vacuum delivery, 14 (1.33%) cases of forceps delivery, and 289 (27.53%) cases of cesarean delivery in the nonqualified group. There were higher rates of forceps delivery in the nonqualified group (P=0.035).
In addition, there were 13 (1.08%) cases with LAM avulsion and 5 (0.42%) cases with AS injury in qualified group; meanwhile, there were 19 (1.81%) cases with LAM avulsion and 9 (0.86%) cases with AS injury in nonqualified group. These differences were not significantly significant.
Intra- and interobserver reliabilities
As shown in Table 2, the inter-observer reliabilities for all 5 parts of the examination were relatively high, with the kappa value ranging from 0.772 to 0.881 (95% CI: 0.560–1.040). Additionally, the intraobserver reliability was also good, with the kappa value ranging from 0.886 to 0.950 (95% CI: 0.733–1.053) and 0.842 to 0.900 (95% CI: 0.670–1.044) for the 2 respective experts.
Table 2
| Parts | Intraobserver reproducibility (n=40) | Interobserver reproducibility (n=40) | ||||||
|---|---|---|---|---|---|---|---|---|
| Expert 1 | Expert 2 | Expert 1 vs. Expert 2 | ||||||
| Kappa | 95% CI | Kappa | 95% CI | Kappa | 95% CI | |||
| 2D-r | 0.886 | 0.733–1.039 | 0.875 | 0.706–1.044 | 0.827 | 0.641–1.013 | ||
| 2D-s | 0.896 | 0.755–1.037 | 0.842 | 0.670–1.014 | 0.792 | 0.598–0.986 | ||
| LAH | 0.886 | 0.733–1.039 | 0.890 | 0.743–1.037 | 0.772 | 0.560–0.984 | ||
| LAM | 0.942 | 0.830–1.053 | 0.881 | 0.722–1.040 | 0.881 | 0.722–1.040 | ||
| AS | 0.950 | 0.852–1.048 | 0.900 | 0.765–1.035 | 0.850 | 0.688–1.013 | ||
2D-r, 2-dimensional image at rest; 2D-s, 2-dimensional image at strain; LAH, levator ani hiatus; LAM, levator ani muscle; AS, anal sphincter.
Quality assessment results
For each participating center, the qualified rate ranged from 12.00% to 86.92%, only 5/31 (16.13%) centers had a rate of qualification of more than 75%, and 22/31 (70.97%) centers achieved a rate of more than 50%.
Among the 2,251 enrolled cases, the rate of qualification for each part was as follows: 94.27% (2,122/2,251) for 2D-r, 78.54% (1,768/2,251) for 2D-s, 85.52% (1,925/2,251) for LAH, 93.03% (2,094/2,251) for LAM, and 88.09% (1,983/2,251) for AS.
Reasons for nonqualification
Of the nonqualified images (n=1,050), the highest proportion were from the 2D-s part, with a nonqualification rate of 46.00% (483/1,050), followed by LAH (326/1,050, 31.05%), AS (268/1,050, 25.52%), LAM (157/1,050, 14.95%), and 2D-r (129/1,050, 12.29%).
Figure 3 shows that the frequency distribution of reasons for nonqualification. The most common reason for 2D-r image nonqualification was an error in image acquisition (80/129, 62.02%). As for 2D-s images, errors in image acquisition (221/483, 45.76%) and measurement (262/483, 54.24%) were the main reasons for nonqualification. For LAH images, errors in image acquisition (275/326, 84.36%) was the main reason for nonqualification. Reconstruction errors were the most common reasons for nonqualification for LAM (133/157, 84.71%) and AS images (133/268, 49.63%).

As shown in Table 3, the reasons for the nonqualification of 2D-r images were as follow: a residual urine volume of more than 50 mL (35/129, 27.13%), distance between the probe and perineum (DPP) of more than 10 mm (30/129, 23.26%), and error in identification of the SP (15/129, 11.63%) and BN (15/129, 11.63%).
Table 3
| Part | Image acquisition | Image postprocessing | |||||
|---|---|---|---|---|---|---|---|
| N (%) | Reason | n (%) | N (%) | Reason | n (%) | ||
| 2D-r (N=129) | 80 (62.02) | RU >50 mL | 35 (27.13) | 49 (37.98) | Misidentification of SP | 15 (11.63) | |
| PSD >10 mm | 30 (23.26) | Misidentification of BN | 15 (11.63) | ||||
| Urethra unclear | 12 (9.30) | Error of RVA-r | 11 (8.53) | ||||
| Anal canal unclear | 13 (10.08) | Error of tilt angle-r | 8 (6.20) | ||||
| Too much gas in rectal ampulla | 2 (1.55) | ||||||
| 2D-s (N=483) | 221 (45.76) | RU >50 mL | 32 (6.63) | 262 (54.24) | Misidentification of SP | 23 (4.76) | |
| Too much gas in rectal ampulla | 11 (2.28) | Misidentification of BN | 35 (7.25) | ||||
| Valsalva duration <6 s | 36 (7.45) | Misidentification of bladder | 46 (9.52) | ||||
| Levator coactivation | 91 (18.84) | Misidentification of uterus | 58 (12.01) | ||||
| Pressure on perineum | 11 (2.28) | Misidentification of rectum ampulla | 100 (20.70) | ||||
| Urethra unclear | 50 (10.35) | Error of RAS-r | 47 (9.73) | ||||
| Anal canal unclear | 45 (9.32) | Error of ROA | 4 (0.83) | ||||
| Levator unclear | 3 (0.62) | ||||||
| LAH (N=326) | 275 (84.36) | RU >50 mL | 31 (9.51) | 51 (15.64) | Not on the maximum Valsalva | 6 (1.84) | |
| Too much gas in rectal ampulla | 7 (2.15) | Measurement error | 45 (13.80) | ||||
| Valsalva duration <6 s | 26 (7.98) | ||||||
| Levator coactivation | 110 (33.74) | ||||||
| Pressure on perineum | 3 (0.92) | ||||||
| Nonmidsagittal view | 64 (19.63) | ||||||
| Levator unclear | 15 (4.60) | ||||||
| Pubic bone unclear | 3 (0.92) | ||||||
| Lateral boundary unclear | 41 (12.58) | ||||||
| LAM (N=157) | 24 (15.29) | LA unclear | 19 (12.10) | 133 (84.71) | Sampling line error | 110 (70.06) | |
| Nonmidsagittal view | 5 (3.18) | Left-right asymmetry | 20 (12.74) | ||||
| SP unclear | 3 (1.91) | ||||||
| AS (N=268) | 31 (11.57) | Poor adhesion to the anus | 15 (5.60) | 237 (88.43) | Sampling line error | 176 (65.67) | |
| Anal canal unclear | 16 (5.97) | Nonorthogonal section | 58 (21.64) | ||||
| Image overmagnification | 3 (1.12) | ||||||
2D-r, 2-dimensional image at rest; 2D-s, 2-dimensional image at strain; LAH, levator ani hiatus; LAM, levator ani muscle; AS, anal sphincter; RU, residual urine; PSD, probe to symphysis pubis distance; SP, symphysis pubis; BN, bladder neck; RVA-r, retrovesical angle at rest; RAV-s, retrovesical angle at strain; ROA, rotation angle.
As for the 2D-s images, about 45.76% (221/483) of the errors occurred during image acquisition, with reasons including LA coactivation (91/483, 18.84%), a Valsalva duration of less than 6 s (36/483, 7.45%), and an unclear urethra (50/483, 10.35%) or anal canal (45/483, 9.32%). The most common errors in measurement were misidentification of pelvic floor organs, including the ampullary rectum (100/483, 20.70%) and uterus (58/483, 12.01%).
Meanwhile, the main reasons of nonqualification for LAH images were errors in image acquisition (275/326, 84.36%) and the measurement of the area of LAH (51/326, 15.64%). Error during image acquisition included LAM coactivation (110/326, 33.73%) and loss of the midsagittal section (64/326, 19.63%).
Finally, the most common error for LAM and AS images was improper sampling line placement, with a nonqualification rate of 70.06% (110/157) and 65.67% (176/268), respectively. Images that were partially nonqualified are shown in Figure 4.
Discussion
Studies have shown that TPUS has good consistency, especially in the measurement of the LAH area (19-24). However, consistency assessment is primarily used for measurements of the structures and cannot truly reflect the standard condition of the image. To our best knowledge, the quality assessment of TPUS has not yet been reported. In this study, we enrolled 2,215 patients who received TPUS examination from 31 tertiary medical centers in China. In order to comprehensively assess the quality of TPUS, we evaluated the quality of the 5 main parts of TPUS and quality of 2 aspects relevant during clinical operation, including the image acquisition and postprocessing of each part. Furthermore, the reasons for the nonqualification of each part were analyzed. These findings may provide basis for the standardized operation and training of TPUS.
This study found that the qualification rates for the 5 parts of TPUS ranged from 78.54% to 94.27%. These results suggest that all parts of the examination exhibited relatively high qualification rates, indicating the broad applicability of TPUS, particularly in tertiary medical centers. The detailed operational requirements provided by practice guidelines likely contributed to these high rates. However, it is important to note that even in tertiary medical centers, there were significant variations in the qualification rates, ranging from 12.00% to 86.92%. This disparity in TPUS quality emphasizes the need to evaluate image quality in each center before implementing it in clinical practice. Ongoing quality management programs may be necessary for centers with lower qualification rates to ensure that consistent standards are maintained.
Two-dimensional Valsalva section plays a critical role in TPUS, particularly in the screening of SUI and the diagnosis of POP. However, this study also revealed that the qualification rate of the 2D Valsalva section was the lowest, with a rate of 78.54%. This indicates that the section has high requirements on operators. Other studies have also indicated that the 2D Valsalva section presents the greatest challenges to operators, with the lowest consistency of measurements (27). Importantly, our study determined the reasons for nonqualification, revealing that both image acquisition (45.76%) and postprocessing (54.24%) are crucial. In terms of image acquisition, levator ani coactivation (18.84%) and unclear visualization of the urethra (10.35%) and the anal canal (9.32%) were the most common reasons for nonqualified images. In postprocessing measurements, the most frequent errors occurred in identifying the structures of the 3 compartments: the bladder (9.52%), uterus (12.01%), and rectocele (20.70%). Therefore, it is urgent to improve operators’ real-time probe adjustment skills and their ability to identify pelvic floor structures in order to address these issues. Additionally, operators should receive training on how to avoid confounding factors and appropriately guide patients during Valsalva maneuvers. These findings may have the potential to improve the qualification rate of the 2D Valsalva section.
Measurements of the LAH area are considered to be a reproducible (24). However, in this study, the qualification rate of the LAH section was 85.52% (1,925/2,251), which ranked second among the parts in nonqualification rate. This result is not consistent with previous studies. This may be due to the fact that in addition to measurement, this study also involved the image acquisition and reconstruction of LAH. Moreover, in the analysis of reasons for nonqualification, it was found that errors in image acquisition (84.36%) were significantly more common than were errors in reconstruction (1.84%) and measurement (13.80%). This indicates that there are more challenges and difficulties in the process of image acquisition. In addition, the most common errors in image acquisition were excessive residual urine (11.27%), coactivation of LAM (40%), missing of the median sagittal section (23.27%), and unclear delineation of LAH borders (14.91%). These findings serve as a reminder that training in acquisition of 4D Valsalva images is a means to improving the image quality of LAH.
The pelvic floor muscles (PFMs) consist of the LAM (13) and the AS (28). Ultrasound diagnosis of PFM injuries presents challenges due to the intricate anatomy and operator expertise required. However, the introduction TUI with 3D or 4D ultrasound has enhanced the visual clarity of ultrasound images by providing tomographic slices in the axial or transverse planes of the PFMs. Through adherence with the recommended reconstruction methods outlined in practice guidelines, TUI has shown comparable diagnostic accuracy to the gold standard of magnetic resonance imaging (13,29) and transrectal ultrasound (30). This study also revealed high rates of qualification for the LAM (93.03%) and AS (88.09%). However, the primary errors in the PFM sections were linked to the placement of sampling lines, accounting for 70.06% of errors in LAM and 65.67% in AS. Correct placement of sampling lines is a crucial aspect of training and can pose difficulties. For LAM reconstruction, operators need to correctly identify the SP (31), while accurate identification of the dorsal AS is necessary for AS reconstruction (31,32).
However, there are several limitations in this study. First, in comparison to other studies, this study reported lower rates of LAM avulsion (1–36% vs. 1.42%) (33) and AS injury (0.5–17% vs. 0.62%) (34), suggesting potential overestimation of the qualification rate. Second, it is important to note that our study did not include secondary or community hospitals, which should be examined in further research. Third, the study population primarily consisted of postpartum women who were relatively young, and thus the findings may not be directly applicable to older populations where image quality is expected to be lower. To address this limitation, we are conducting another study on the current status of TPUS quality in older adult women.
Conclusions
This multicenter study assessed the quality of TPUS in tertiary medical centers in China and identified the common reasons for nonqualified images in each section. These findings may form the basis for quality control management and training for TPUS. We call for strengthening TPUS quality control, improving accuracy and reliability, enhancing standardized application, and elevating the clinical value of TPUS.
Acknowledgments
Funding: This study was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-176/coif). MZ, JW, XL, EQ, and XZ report that this study was supported by the Municipal and University (Hospital) Joint Funding Project of Guangzhou Municipal Science and Technology Bureau (No. SL2022A03J00358), the Natural Science Foundation of Guangdong Province, China (No. 2022A1515012027), and the Fundamental Research Funds for the Central Universities, Sun Yat-sen University (No. 23qnpy142). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Human Research Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University (No. [2020] 02-156-01). All participating hospitals were informed of the study details before agreeing to participate. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The need for informed consent of patients was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Khatri G, Bhosale PR, Robbins JB, Akin EA, Ascher SM, Brook OR, Dassel M, Glanc P, Henrichsen TL, Learman LA, Sadowski EA, Saphier CJ, Wasnik AP, Maturen KE. ACR Appropriateness Criteria® Pelvic Floor Dysfunction in Females. J Am Coll Radiol 2022;19:S137-55.
- Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ. Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008;300:1311-6. [Crossref] [PubMed]
- Nygaard I, Bradley C, Brandt D. Pelvic organ prolapse in older women: prevalence and risk factors. Obstet Gynecol 2004;104:489-97. [Crossref] [PubMed]
- Zhu L, Davila GW. New considerations regarding pelvic organ prolapse treatment in China. Chin Med J (Engl) 2012;125:1209-11.
- Zhu L. Surgical Treatment of Stress Urinary Incontinence in Women in the Mainland of China: Current Status and Outlook. Chin Med J (Engl) 2017;130:1387-8. [Crossref] [PubMed]
- Zhang L, Zhu L, Chen J, Xu T, Lang JH. Tension-free polypropylene mesh-related surgical repair for pelvic organ prolapse has a good anatomic success rate but a high risk of complications. Chin Med J (Engl) 2015;128:295-300. [Crossref] [PubMed]
- Xue K, Palmer MH, Zhou F. Prevalence and associated factors of urinary incontinence in women living in China: a literature review. BMC Urol 2020;20:159. [Crossref] [PubMed]
- Hu X, Liu Y, Dang Q, Wang D, Feng S. Questionnaire survey on 2913 cases of women’s pelvic floor functional disorder. Chongqing Medical 2014;43:2181-3.
- Gomelsky A, Penson DF, Dmochowski RR. Pelvic organ prolapse (POP) surgery: the evidence for the repairs. BJU Int 2011;107:1704-19. [Crossref] [PubMed]
- Angioli R, Plotti F, Muzii L, Montera R, Panici PB, Zullo MA. Tension-free vaginal tape versus transobturator suburethral tape: five-year follow-up results of a prospective, randomised trial. Eur Urol 2010;58:671-7. [Crossref] [PubMed]
- Dietz HP. Pelvic Floor Ultrasound: A Review. Clin Obstet Gynecol 2017;60:58-81.
- AIUM/IUGA practice parameter for the performance of Urogynecological ultrasound examinations: Developed in collaboration with the ACR, the AUGS, the AUA, and the SRU. Int Urogynecol J 2019;30:1389-400.
- Van Gruting IMA, Stankiewicz A, Van Delft KWM, Doumouchtsis SK, Inthout J, Sultan AH, Thakar R. Diagnostic test accuracy of magnetic resonance imaging and pelvic floor ultrasound for diagnosis of levator ani muscle avulsion. Ultrasound Obstet Gynecol 2022;60:559-69. [Crossref] [PubMed]
- Staack A, Vitale J, Ragavendra N, Rodríguez LV. Translabial ultrasonography for evaluation of synthetic mesh in the vagina. Urology 2014;83:68-74. [Crossref] [PubMed]
- Zhang X, Xiang Y, Yao J, Hu X, Wang Y, Liu L, Wang Y, Wu Y. Automatic segmentation of the female pelvic floor muscles on MRI for pelvic floor function assessment. Quant Imaging Med Surg 2023;13:4181-95. [Crossref] [PubMed]
- Hilde G, Staer-Jensen J, Siafarikas F, Gjestland K, Ellström Engh M, Bø K. How well can pelvic floor muscles with major defects contract? A cross-sectional comparative study 6 weeks after delivery using transperineal 3D/4D ultrasound and manometer. BJOG 2013;120:1423-9. [Crossref] [PubMed]
- Halle TK, Staer-Jensen J, Hilde G, Bø K, Ellström Engh M, Siafarikas F. Change in prevalence of major levator ani muscle defects from 6 weeks to 1 year postpartum, and maternal and obstetric risk factors: A longitudinal ultrasound study. Acta Obstet Gynecol Scand 2020;99:1403-10. [Crossref] [PubMed]
- Qu E, Wu J, Zhang M, Wu L, Zhang T, Xu J, Zhang X. The ultrasound diagnostic criteria for diastasis recti and its correlation with pelvic floor dysfunction in early postpartum women. Quant Imaging Med Surg 2021;11:706-13. [Crossref] [PubMed]
- Majida M, Braekken IH, Umek W, Bø K, Saltyte Benth J, Ellstrøm Engh M. Interobserver repeatability of three- and four-dimensional transperineal ultrasound assessment of pelvic floor muscle anatomy and function. Ultrasound Obstet Gynecol 2009;33:567-73. [Crossref] [PubMed]
- Eisenberg VH, Steinberg M, Weiner Z, Alcalay M, Itskovitz-Eldor J, Schiff E, Lowenstein L. Three-dimensional transperineal ultrasound for imaging mesh implants following sacrocolpopexy. Ultrasound Obstet Gynecol 2014;43:459-65. [Crossref] [PubMed]
- Dietz HP, Kamisan Atan I, Salita A. Association between ICS POP-Q coordinates and translabial ultrasound findings: implications for definition of 'normal pelvic organ support'. Ultrasound Obstet Gynecol 2016;47:363-8. [Crossref] [PubMed]
- Lone FW, Thakar R, Sultan AH, Stankiewicz A. Accuracy of assessing Pelvic Organ Prolapse Quantification points using dynamic 2D transperineal ultrasound in women with pelvic organ prolapse. Int Urogynecol J 2012;23:1555-60. [Crossref] [PubMed]
- Tan L, Shek KL, Atan IK, Rojas RG, Dietz HP. The repeatability of sonographic measures of functional pelvic floor anatomy. Int Urogynecol J 2015;26:1667-72. [Crossref] [PubMed]
- Nardos R, Thurmond A, Holland A, Gregory WT. Pelvic floor levator hiatus measurements: MRI versus ultrasound. Female Pelvic Med Reconstr Surg 2014;20:216-21. [Crossref] [PubMed]
- Salomon LJ, Bernard JP, Duyme M, Doris B, Mas N, Ville Y. Feasibility and reproducibility of an image-scoring method for quality control of fetal biometry in the second trimester. Ultrasound Obstet Gynecol 2006;27:34-40. [Crossref] [PubMed]
- van Veelen GA, Schweitzer KJ, van Delft K, Kluivers KB, Weemhoff M, van der Vaart CH. Diagnosing levator avulsions after first delivery by tomographic ultrasound: reliability between observers from different centers. Int Urogynecol J 2014;25:1501-6. [Crossref] [PubMed]
- Dietz HP, Steensma AB. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: the distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet Gynecol 2005;26:73-7. [Crossref] [PubMed]
- Dietz HP. Exoanal Imaging of the Anal Sphincters. J Ultrasound Med 2018;37:263-80.
- Yan Y, Dou C, Wang X, Xi Y, Hu B, Ma L, Ying T. Combination of tomographic ultrasound imaging and three-dimensional magnetic resonance imaging-based model to diagnose postpartum levator avulsion. Sci Rep 2017;7:11235. [Crossref] [PubMed]
- Okeahialam NA, Thakar R, Sultan AH. Comparison of diagnostic criteria for significant anal sphincter defects between endoanal and transperineal ultrasound. Ultrasound Obstet Gynecol 2022;60:793-9. [Crossref] [PubMed]
- Lee JH, Pretorius DH, Weinstein M, Guaderrama NM, Nager CW, Mittal RK. Transperineal three-dimensional ultrasound in evaluating anal sphincter muscles. Ultrasound Obstet Gynecol 2007;30:201-9. [Crossref] [PubMed]
- Dietz HP. Ultrasound imaging of maternal birth trauma. Int Urogynecol J 2021;32:1953-62.
- Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol 2012;39:372-83. [Crossref] [PubMed]
- Spinelli A, Laurenti V, Carrano FM, Gonzalez-Díaz E, Borycka-Kiciak K. Diagnosis and Treatment of Obstetric Anal Sphincter Injuries: New Evidence and Perspectives. J Clin Med 2021;10:3261. [Crossref] [PubMed]


