
Reduction quality in lateral view of X-ray and hypoalbuminemia are associated with postoperative mortality in elderly pertrochanteric fracture patients
Introduction
Hip fragility fractures are one of the most common public health issues across the world as the population ages (1,2). According to recent studies, it is predicted that the number of hip fracture cases in China will grow six-fold from 0.7 million instances in 2013 to 4.5 million cases in 2050 (2,3).
Between 1/3 and 1/2 of all hip fractures are pertrochanteric fractures, which are a frequent injury. The mortality rate of this type of fracture at 1 year varies from 14% to 36% (4). For quick rehabilitation and healing after fractures, surgical fixation is advised. The most popular method for fixing the fractures is intramedullary nailing, particularly for unstable fractures (5). However, even after surgery, 25% of patients with these fractures need to be cared for at home, and more than 50% lose the ability to walk independently (6,7).
In prior studies, the mortality rate of pertrochanteric fracture has been linked to a variety of clinical parameters, including age, gender, American Society of Anesthesiologists (ASA) score, time to surgery, and surgeon grade (8-12). Multiple studies have also examined surgical factors, such as fracture classification, tip-apex distance (TAD), position of the lag screw, augmentation, and reduction quality, in relation to implant failure in pertrochanteric fractures (13-17). In the initial postoperative phase, surgical factors are crucial determinants of a patient’s capacity for unrestricted weight-bearing, in addition with patient-dependent factors (e.g., previous mobility and dementia). Long-term immobility compromises the dignity of elderly and weak individuals and raises the risk of post-operative complications, such as delirium, thrombosis, hospital-acquired infection, pressure-mediated skin injury, loss of muscular strength, and diminished rehabilitation potential (18). To our knowledge, despite the fact that surgical factors have been shown to be independent risk factors for implant failure, few studies have examined the association between surgical factors and post-operative mortality rate (19-21).
In this study, we aimed to examine the association between the postoperative mortality of patients with intramedullary nail-treated pertrochanteric fractures and surgical factors, including the Dorr morphology, Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association (AO/OTA) classification of fractures (22), TAD, location of the cephalic screw, reduction quality in anterior-posterior (AP) and lateral views, the integrity of the lateral wall, and the design of cephalic screws. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-424/rc).
Methods
Patients and study design
The retrospective study was approved by the Institutional Review Board (IRB) of Peking University First Hospital (No. 2021-432) and the requirement for individual consent for this retrospective analysis was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Between January 2016 and February 2021, this retrospective analysis examined the pertrochanteric fracture patients who received internal fixation with intramedullary nails at Peking University First Hospital. The inclusion criteria were as follows: (I) age ≥70 years; (II) diagnosed with pertrochanteric fracture; (III) fracture fixed using intramedullary nail. The exclusion criteria were as follows: (I) pathological fracture; (II) fracture treated with plate or hip arthroplasty; (III) fracture treated conservatively; (IV) incomplete data or lost follow-up.
Surgical and postoperative management
Prior to surgery, all patients were assessed with routine AP and lateral radiographs in bilateral hips. Upon completion of preoperative preparations, all patients had surgery as quickly as possible while under regional or general anesthesia. In a supine posture on a traction table, intramedullary nailing was performed on patients with pertrochanteric fractures. All operations were carried out under fluoroscopic supervision. Utilizing a traction table and closed manipulation procedures, patients underwent closed reduction. When the operating surgeon felt that reduction was insufficient, supplementary percutaneous or open reduction procedures were used to maximize reduction. After surgery, standard AP and lateral radiographs of the bilateral hips were acquired. Depending on the patient, fracture morphology, reduction, and implant site, the patient was able to bear no, partial, or full weight. After discharge, patients were contacted and followed up by telephone. The minimal follow-up duration was 12 months after surgery. If the patient had died before the follow-up time, the date of death was recorded.
Data collection
The basic information of patients, including age and gender, ASA score, preoperative waiting time, anesthetic type, blood transfusion information, pre-operative levels of hemoglobin (Hb) and albumin (Alb), were retrieved with care from their electronic medical records. Additionally, the preoperative and postoperative radiographs were measured to establish the surgical factors. The surgical factors included the Dorr morphology, AO/OTA classification of fractures, TAD, location of the cephalic screw, reduction quality in AP and lateral views, the integrity of the lateral wall, and the design of cephalic screws. As for the measurement of surgical indicators in postoperative radiographs, 2 trained orthopedic surgeons with junior titles measured or evaluated the indicators without knowing other information of patients. If the results diverged, a senior orthopedic surgeon re-measured or re-evaluated.
The Dorr morphology was evaluated as described by Dorr et al. (23). The intramedullary canal width (B) was measured at the position of 10 cm below the mid-lesser trochanter. Also measured was the intramedullary canal diameter at the level of the mid-lesser trochanter (A). Canal-to-calcar ratio (CCR) was calculated as the ratio of B to A and was used to assess the proximal femoral morphology. The Dorr morphology was defined as follows: Type A <0.5 CCR, Type B as 0.5–0.75 CCR, and Type C >0.75 CCR (Figure 1). There was no case of Dorr Type C in our study.

The TAD was firstly described by Baumgaertner et al. in 1995 (17) and is defined as the sum of the distance from the tip of the lag screw to the apex of the femoral head measured on the AP and lateral radiograph.
On the postoperative radiographs, the location of the cephalic screw was assessed as reported by Cleveland et al. (24). On the AP and lateral radiographs, the placement of the cephalic screw in the femoral head was classified as superior, middle, or inferior. The cephalic screw in the center or inferior of the femoral head on the AP view and in center on the lateral view were defined as proper position, whereas all other positions were considered as improper.
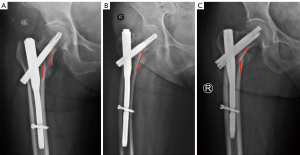
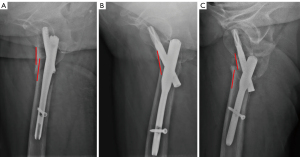
According to the studies by Baumgaertner et al. (25) and Chang et al. (26), the quality of reduction of AP and lateral fractures was assessed using AP and lateral X-rays, respectively. In the AP view, it was defined as good that the femoral neck-shaft angle was slight valgus or normal for alignment, and that the medial cortical support was positive and neutral, and no more than 4 mm of displacement of any fragment. In the lateral view, an angulation of 20° for alignment and a positive or neutral anteromedial cortical contact were considered good reduction. If the reduction did not meet the criteria in AP or lateral view, the reduction was rated poor (Figures 2,3).
On preoperative radiographs or computed tomography (CT) scans, the lateral femoral wall fracture was characterized as a fracture line that crosses the lateral wall (27). According to the difference in cephalic screws, the intramedullary nails in our research were categorized as either single blade devices (PFNa; AO Synthes, Raynham, MA, USA) or double screw devices (InterTAN; Smith & Nephew, London, UK).
Statistical analysis
The categorical variables were quantified and evaluated using the chi-square test. Continuous variables were recorded as the mean ± standard deviation and evaluated using either the Student’s t-test or the Wilcoxon rank-sum test. The Kaplan-Meier technique was used to plot survival curves. Initially, the risk factors for postoperative mortality were evaluated using a univariate Cox proportional hazards regression model with a significance level of P<0.05. The selected covariates were subsequently examined using backward stepwise multivariate Cox proportional hazards regression, and variables with P values <0.05 were determined to be the final predictors. All statistical analyses were performed using SPSS 26.0 (IBM Corp., Armonk, NY, USA).
Results
From January 2016 to February 2021, a total of 242 pertrochanteric fracture patients were treated at our institution. We excluded patients under the age of 70 (n=52), those treated with plates or arthroplasty (n=11), and those who were lost to follow-up (n=10). Finally, a total of 169 pertrochanteric fracture patients treated with intramedullary nails were included in our study, with the average age of 82.68±5.93 years (as shown in Figure 4). There were 48 males and 121 females among the participants. The Spinal anesthesia group included 120 patients (71%); the number of patients in the General anesthesia group was 49 (29%). There were 21 (12.4%) patients with open reduction and 148 (87.6%) patients with closed reduction. The basic characteristics are all shown in Table 1. The mean survival time of enrolled patients was 34.11±19.89 months, and the death rates at 3 months, 1 year, and the end of follow-up were 4.14%, 11.24%, and 26.04%, respectively (Figure 5). The specifics of assessing surgical factors, such as AO/OTA classification of fractures, Dorr morphology, TAD, location of the cephalic screw, reduction quality in the AP and lateral views, the integrity of the lateral wall, and the design of cephalic screws, are displayed in Table 1.
Table 1
| Characteristics | Data, n (%) or mean ± SD |
|---|---|
| Age (years) | 82.68±5.93 |
| Gender | |
| Male | 48 (28.4) |
| Female | 121 (71.6) |
| Anesthesia | |
| Spinal | 120 (71.0) |
| General | 49 (29.0) |
| ASA score | |
| 2 | 74 (43.8) |
| 3 | 88 (52.1) |
| 4 | 7 (4.1) |
| Preoperative waiting time (days) | 4.47±2.78 |
| Blood transfusion | |
| Yes | 93 (55.0) |
| No | 76 (45.0) |
| Hemoglobin (g/L) | 111.41±16.95 |
| Albumin (g/L) | 36.15±3.73 |
| AO/OTA classification | |
| 31A1 | 31 (18.3) |
| 31A2 | 133 (78.7) |
| 31A3 | 5 (3.0) |
| Dorr morphology | |
| Type A | 68 (40.2) |
| Type B | 101 (59.8) |
| TAD (mm) | 19.93±4.29 |
| Cephalic screw position | |
| Good | 120 (71.0) |
| Poor | 49 (29.0) |
| Reduction in AP view | |
| Good | 131 (77.5) |
| Poor | 38 (22.5) |
| Reduction in lateral view | |
| Good | 156 (92.3) |
| Poor | 13 (7.7) |
| Lateral wall fracture | |
| No | 135 (79.9) |
| Yes | 34 (20.1) |
| Design of cephalic screws | |
| Single blade | 129 (76.3) |
| Double screws | 40 (23.7) |
SD, standard deviation; ASA score, American Society of Anesthesiologists score; AO/OTA, Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association; TAD, tip-apex distance; AP, anterior-posterior.
According to the univariate Cox analysis, among the basic characteristics, age [hazard ratio (HR) 1.054, 95% confidence interval (CI): 1.005–1.106, P=0.031], gender (HR 2.063, 95% CI: 1.137–3.745, P=0.017), pre-operative levels of Hb (HR 0.975, 95% CI: 0.957–0.993, P=0.006) and Alb (HR 0.825, 95% CI: 0.768–0.885, P<0.001) were associated with a poor overall survival (OS). However, there were no statistically significant differences in anesthesia type, ASA score, pre-operative waiting time, and blood transfusion (P>0.05; as shown in Table 2). For the measuring surgical factors, poor reduction in lateral view (HR 2.626, 95% CI: 1.170–5.896, P=0.019) was significantly associated with the higher overall mortality at the end of follow-up. In terms of Dorr morphology, TAD, position of cephalic screw, reduction in AP view, the integrity of lateral wall, and the design of cephalic screws, the difference had no statical significance (P>0.05; as shown in Table 3).
Table 2
| Factors | HR (95% CI) | P |
|---|---|---|
| Age (per 1-year increase) | 1.054 (1.005–1.106) | 0.031* |
| Gender | 2.063 (1.137–3.745) | 0.017* |
| Male | ||
| Female | ||
| Anesthesia | 1.444 (0.713–2.924) | 0.308 |
| Spinal | ||
| General | ||
| ASA score | ||
| 2 | 1.000 (Reference) | |
| 3 | 1.668 (0.225–12.380) | 0.617 |
| 4 | 1.533 (0.206–11.427) | 0.677 |
| Preoperative waiting time (days) | 1.027 (0.938–1.123) | 0.565 |
| Blood transfusion | 0.616 (0.333–1.140) | 0.123 |
| No | ||
| Yes | ||
| Hemoglobin (g/L) | 0.975 (0.957–0.993) | 0.006* |
| Albumin (g/L) | 0.825 (0.768–0.885) | <0.001* |
*, P<0.05 with significant difference. HR, hazard ratio; CI, confidence interval; ASA score, American Society of Anesthesiologists score.
Table 3
| Factors | HR (95% CI) | P |
|---|---|---|
| AO/OTA classification | ||
| 31A1 | 1.000 (Reference) | |
| 31A2 | 0.374 (0.039–3.616) | 0.396 |
| 31A3 | 1.419 (0.194–10.364) | 0.730 |
| Dorr morphology (Type A/Type B) | 0.578 (0.306–1.094) | 0.092 |
| TAD, mm | 1.026 (0.961–1.095) | 0.450 |
| Cephalic screw position (Good/Poor) | 1.665 (0.800–3.465) | 0.173 |
| Reduction in AP view (Good/Poor) | 1.679 (0.890–3.167) | 0.110 |
| Reduction in lateral view (Good/Poor) | 2.626 (1.170–5.896) | 0.019* |
| Lateral wall fracture (No/Yes) | 0.695 (0.351–1.375) | 0.296 |
| Design of cephalic screws (Single blade/Double screws) |
1.526 (0.694–3.261) | 0.338 |
*, P<0.05 with significant difference. HR, hazard ratio; CI, confidence interval; TAD, tip-apex distance; AO/OTA, Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association; AP, anterior-posterior.
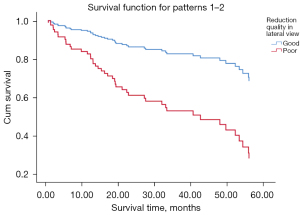
The pertinent variables discovered by univariate Cox regression analysis were included into a multivariable Cox proportional risk model. The multivariate analysis revealed that the lower pre-operative level of Alb (HR 0.851, 95% CI: 0.780–0.929, P<0.001) and the poor reduction in lateral view (HR 0.298, 95% CI: 0.129–0.689, P<0.001) were independent risk factors for poor OS (Table 4 and Figure 6).
Table 4
| Factors | HR (95% CI) | P |
|---|---|---|
| Age (per 1-year increase) | 1.027 (0.975–1.082) | 0.315 |
| Gender | 1.553 (0.791–3.051) | 0.201 |
| Hemoglobin, g/L | 0.986 (0.967–1.006) | 0.164 |
| Albumin, g/L | 0.851 (0.780–0.929) | <0.001* |
| Reduction in lateral view (good/poor) | 0.298 (0.129–0.689) | <0.001* |
*, P<0.05 with significant difference. HR, hazard ratio; CI, confidence interval.
Discussion
According to our study, the preoperative level of Alb and the reduction quality in lateral view are associated with postoperative mortality in elderly pertrochanteric fracture patients. Surgical operation is the first choice for the treatment of this type of fracture. In unstable fracture patterns, it is widely acknowledged that intramedullary fixation is superior to extramedullary implants (5). Many previous studies have investigated the prognostic factors for the postoperative mortality of pertrochanteric fracture patients, such as age, gender, ASA score, and preoperative waiting time (8-12). The relationship between mortality rate and surgical factors, which have been shown to be associated with implant failure, has not been widely investigated in prior research.
In our study, we investigated the relationship between survival of pertrochanteric fracture patients treated with intramedullary nails and surgical factors, including Dorr morphology, TAD, position of cephalic screw, reduction in AP and lateral views, the integrity of lateral wall, and the design of cephalic screws. Among the variables, fracture reduction quality in the lateral view appeared to be an important predictor of postoperative mortality in this type of fractures patients.
Some previous studies have indicated the correlation between fracture reduction quality and the postoperative survival of elderly patients with pertrochanteric fractures. He et al. (28) found that compared with patients with an excellent reduction, those with an acceptable reduction had a 1.1-fold increase in mortality at the 1-year follow-up, whereas those with a poor reduction had a 13.8-fold increase in mortality. A study including 329 patients revealed that there appeared to be a correlation between fracture reduction and postoperative survival of geriatric hip fracture patients at 1 year (20). Unlike previous investigations, we assessed the reduction quality of fracture in the AP and lateral views separately, as opposed to combining them. To our knowledge, few people have found that reduction quality in the lateral view was probably the key factor influencing the postoperative mortality of pertrochanteric fracture patients, even more than reduction quality in the AP view, which seemed to have no impact on the survival of patients. In previous studies, AP radiographs were used more often for assessing reduction quality, and there was lack of consensus regarding the quality of fracture reduction in lateral radiographs. Tsukada et al. (29) revealed that excessive sliding occurred following the surgical treatment for pertrochanteric fractures with posterior displacement of the head and neck fragment. Momii et al. (30) found that inadequate reduction on either the AP or lateral views was correlated with significant postoperative sliding. The research by Kristan et al. (14) demonstrated that reduction of pertrochanteric fractures in lateral view influenced the healing rate of fracture and walking ability after half a year. These prior studies and our own study highlight that surgeons must make every effort to improve the reduction quality of pertrochanteric fractures specially in the lateral view in clinical practice.
Pain and biomechanics are 2 potential causes for the correlation between reduction quality of fractures and patient survival. The primary aim of pertrochanteric fracture surgery is early mobilization to prevent problems associated with bed rest and death (31). Poorly reduced fractures may be more painful than anatomically reduced fractures, resulting in delayed mobility and extended bed rest (32). Furthermore, instability caused by mal-reduction can result in limb shortening, loss of abductor function, and implant-related complications (major ones such as cut-out, or minor ones such as lateral hip pain by shortening of the column, etc.), all of which can lead to negative outcomes (33).
In addition, when patients are at a greater risk of death and it is considered more important to proceed with fixation and strive for a shorter surgical time than to continue striving to improve the reduction, surgeons may tolerate a poorer reduction. Similarly, the increased operative time, soft tissue dissection, and blood loss associated with open reduction compared to closed reduction may not be in the best interest of the patient, or their functional demands may be reduced, allowing them to accept a poor reduction. In addition, unskilled surgeons are more likely to perform a poor fracture reduction, and the surgeon’s experience, not the fracture reduction itself, may have more important impact on the patient’s outcome (20). The findings encourage us to a better fracture comprehension and especially to concentrate on the quality of the reduction (14,20).
Several previous studies have also examined the association between femoral bone quality and postoperative mortality. In the study by Nyholm et al. (34), it was found that patients with displaced femoral neck fractures with a thinner cortex had an increased risk of mortality. Nevertheless, similar to our findings, another study found that indicators of femoral bone quality, such as CCR and Dorr type, were not substantially related with the postoperative survival of patients with pertrochanteric fracture (21). This might be due to the differences in bone quality between pertrochanteric and femoral neck fracture of the femur (35). Other surgical factors involving fracture type (AO/OTA classification), implant position (TAD, position of cephalic nails), the integrity of lateral wall, and the design of cephalic screws were found to have no correlation with patient survival in our study, despite having a strong correlation with the final success of operations (36).
Numerous prior studies have demonstrated that preoperative factors such as age, gender, ASA score, and preoperative waiting time are linked with mortality risk (8-12). However, after multivariate adjustment, the preoperative level of Alb was the only factor associated with the mortality of patients in our study. Serum Alb is a routine clinical test, considered a biomarker of inflammation and nutritional status, and a reliable indicator of malnutrition. Hypoalbuminemia is considered an indicator of inflammation, hypercoagulability, and liver disease (37,38). The effect of inflammation on lower Alb levels is a major cause of morbidity and associated mortality (39-41). Therefore, serum Alb levels have been associated with a variety of diseases, and although some studies have not provided direct evidence (42), others have reported that lower serum Alb concentrations are associated with cardiovascular mortality, acute respiratory distress syndrome, acute stroke, chronic kidney disease, and other complications (43-47). In fact, a meta-analysis showed that hypoalbuminemia was an independent predictor of poor prognosis (48), which appeared to be independent of nutritional status and inflammation. Miyanishi et al. (49) demonstrated that low serum Alb level, which was considered a marker of health status, was a significant factor influencing the 4-year mortality after hip fracture. Therefore, for patients with hip fractures, preoperative hypoproteinemia is closely associated with postoperative mortality. Chang et al. (50) conducted a meta-analysis and found that delaying the operation time significantly increased mortality. We hypothesized that the small sample size and short duration of follow-up may have contributed to some of the disparities across the trials.
The study has several limitations. First, it is retrospective research and has inherent biases. Second, although Baumgaertner et al. (25) and Chang et al. (26) demonstrated their reduction quality criteria, there is no universally approved consensus for either anterior-posterior view or lateral view reduction criteria. Third, some other factors, such as following up by phone, lost cases, and so on, may have caused deviations in the results. Fourth, we included 169 patients from a single institution; this small sample size reduced the generalizability of our findings. Consequently, well-designed, multicenter investigations with larger samples are required.
Conclusions
A sufficient preoperative level of Alb and a good reduction quality in lateral view are associated with lower postoperative mortality in elderly pertrochanteric fracture patients. Geriatrics and orthopedic surgeons should notice these parameters to improve their results. Therefore, to improve the prognosis of patients, every effort should be made to optimize reduction quality of pertrochanteric fractures, particularly in lateral view.
Acknowledgments
The authors would like to thank all colleagues from the Department of Orthopedics, Peking University First Hospital, for the help and advice in data collection, analysis of results, and writing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-424/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-424/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board (IRB) of Peking University First Hospital (No. 2021-432) and the requirement for individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis. Eur J Rheumatol 2017;4:46-56. [Crossref] [PubMed]
- Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 2012;23:2239-56. [Crossref] [PubMed]
- Chang SM, Hou ZY, Hu SJ, Du SC. Intertrochanteric Femur Fracture Treatment in Asia: What We Know and What the World Can Learn. Orthop Clin North Am 2020;51:189-205. [Crossref] [PubMed]
- Yu J, Zhang C, Li L, Kwong JS, Xue L, Zeng X, Tang L, Li Y, Sun X. Internal fixation treatments for intertrochanteric fracture: a systematic review and meta-analysis of randomized evidence. Sci Rep 2015;5:18195. [Crossref] [PubMed]
- Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J 2017;99-B:128-33. [Crossref] [PubMed]
- Ariza-Vega P, Lozano-Lozano M, Olmedo-Requena R, Martín-Martín L, Jiménez-Moleón JJ. Influence of Cognitive Impairment on Mobility Recovery of Patients With Hip Fracture. Am J Phys Med Rehabil 2017;96:109-15. [Crossref] [PubMed]
- Vochteloo AJ, Moerman S, Tuinebreijer WE, Maier AB, de Vries MR, Bloem RM, Nelissen RG, Pilot P. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int 2013;13:334-41. [Crossref] [PubMed]
- O'Leary L, Jayatilaka L, Leader R, Fountain J. Poor nutritional status correlates with mortality and worse postoperative outcomes in patients with femoral neck fractures. Bone Joint J 2021;103-B:164-9. [Crossref] [PubMed]
- Cha YH, Ha YC, Ryu HJ, Lee YK, Park SH, Lee KJ, Koo KH. Effect of heart failure on postoperative short and long-term mortality in elderly patients with hip fracture. Injury 2020;51:694-8. [Crossref] [PubMed]
- Whitehouse MR, Berstock JR, Kelly MB, Gregson CL, Judge A, Sayers A, Chesser TJ. Higher 30-day mortality associated with the use of intramedullary nails compared with sliding hip screws for the treatment of trochanteric hip fractures: a prospective national registry study. Bone Joint J 2019;101-B:83-91. [Crossref] [PubMed]
- Mabry SE, Cichos KH, McMurtrie JT, Pearson JM, McGwin G Jr, Ghanem ES. Does Surgeon Fellowship Training Influence Outcomes in Hemiarthroplasty for Femoral Neck Fracture? J Arthroplasty 2019;34:1980-6. [Crossref] [PubMed]
- Sheehan KJ, Sobolev B, Guy P. Mortality by Timing of Hip Fracture Surgery: Factors and Relationships at Play. J Bone Joint Surg Am 2017;99:e106. [Crossref] [PubMed]
- Schneider F, Geir F, Koidl C, Gehrer L, Runer A, Arora R. Retrospective evaluation of radiological and clinical outcomes after surgical treatment of proximal femur fractures utilizing TFNA. Arch Orthop Trauma Surg 2023;143:4165-71. [Crossref] [PubMed]
- Kristan A, Benulič Č, Jaklič M. Reduction of trochanteric fractures in lateral view is significant predictor for radiological and functional result after six months. Injury 2021;52:3036-41. [Crossref] [PubMed]
- Kammerlander C, Hem ES, Klopfer T, Gebhard F, Sermon A, Dietrich M, Bach O, Weil Y, Babst R, Blauth M. Cement augmentation of the Proximal Femoral Nail Antirotation (PFNA) - A multicentre randomized controlled trial. Injury 2018;49:1436-44. [Crossref] [PubMed]
- Hsueh KK, Fang CK, Chen CM, Su YP, Wu HF, Chiu FY. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop 2010;34:1273-6. [Crossref] [PubMed]
- Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 1995;77:1058-64. [Crossref] [PubMed]
- Li J, Zhang L, Zhang H, Yin P, Lei M, Wang G, Wang S, Tang P. Effect of reduction quality on post-operative outcomes in 31-A2 intertrochanteric fractures following intramedullary fixation: a retrospective study based on computerised tomography findings. Int Orthop 2019;43:1951-9. [Crossref] [PubMed]
- Pan L, Ning T, Wu H, Liu H, Wang H, Li X, Cao Y. Prognostic nomogram for risk of mortality after hip fracture surgery in geriatrics. Injury 2022;53:1484-9. [Crossref] [PubMed]
- Macdonald H, Brown R, Gronager M, Close J, Fleming T, Whitehouse M. Quality of fracture reduction is associated with patient survival at one year, but not 30 days, following trochanteric hip fracture fixation. A retrospective cohort study. Injury 2022;53:1160-3. [Crossref] [PubMed]
- Bayram S, Yıldırım AM, Birişik F, Salduz A. Radiological parameter associated with the survival of old patients with hip fracture. Injury 2021;52:3388-96. [Crossref] [PubMed]
- Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and Dislocation Classification Compendium-2018. J Orthop Trauma 2018;32:S1-S170. [Crossref] [PubMed]
- Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone 1993;14:231-42. [Crossref] [PubMed]
- CLEVELAND M. BOSWORTH DM, THOMPSON FR, WILSON HJ Jr, ISHIZUKA T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am 1959;41-A:1399-408.
- Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res 1998;87-94.
- Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg 2015;135:811-8. [Crossref] [PubMed]
- Fan J, Xu X, Zhou F, Zhang Z, Tian Y, Ji H, Guo Y, Lv Y, Yang Z, Hou G. Risk factors for implant failure of intertrochanteric fractures with lateral femoral wall fracture after intramedullary nail fixation. Injury 2021;52:3397-403. [Crossref] [PubMed]
- He M, Liu J, Deng X, Zhang X. The postoperative prognosis of older intertrochanteric fracture patients as evaluated by the Chang reduction quality criteria. BMC Geriatr 2022;22:928. [Crossref] [PubMed]
- Tsukada S, Okumura G, Matsueda M. Postoperative stability on lateral radiographs in the surgical treatment of pertrochanteric hip fractures. Arch Orthop Trauma Surg 2012;132:839-46. [Crossref] [PubMed]
- Momii K, Fujiwara T, Mae T, Tokunaga M, Iwasaki T, Shiomoto K, Kubota K, Onizuka T, Miura T, Hamada T, Nakamura T, Itokawa T, Iguchi T, Yamashita A, Kikuchi N, Nakaie K, Matsumoto Y, Nakashima Y. Risk factors for excessive postoperative sliding of femoral trochanteric fracture in elderly patients: A retrospective multicenter study. Injury 2021;52:3369-76. [Crossref] [PubMed]
- Song H, Chang SM, Hu SJ, Du SC, Xiong WF. Calcar fracture gapping: a reliable predictor of anteromedial cortical support failure after cephalomedullary nailing for pertrochanteric femur fractures. BMC Musculoskelet Disord 2022;23:175. [Crossref] [PubMed]
- Huang JW, Gao XS, Yang YF. Risk factors for cut-outs in geriatric intertrochanteric fractures with cephalomedullary nailing after obtaining acceptable reduction: a case-control study. BMC Musculoskelet Disord 2022;23:354. [Crossref] [PubMed]
- Gilat R, Lubovsky O, Atoun E, Debi R, Cohen O, Weil YA. Proximal Femoral Shortening After Cephalomedullary Nail Insertion for Intertrochanteric Fractures. J Orthop Trauma 2017;31:311-5. [Crossref] [PubMed]
- Nyholm AM, Palm H, Sandholdt H, Troelsen A, Gromov K. Risk of reoperation within 12 months following osteosynthesis of a displaced femoral neck fracture is linked mainly to initial fracture displacement while risk of death may be linked to bone quality: a cohort study from Danish Fracture Database. Acta Orthop 2020;91:1-75. [Crossref] [PubMed]
- Li M, Lv HC, Liu JH, Cui X, Sun GF, Hu JW, Zhang LC, Tang PF. Differences in Bone Mineral Density and Hip Geometry in Trochanteric and Cervical Hip Fractures in Elderly Chinese Patients. Orthop Surg 2019;11:263-9. [Crossref] [PubMed]
- Herman A, Landau Y, Gutman G, Ougortsin V, Chechick A, Shazar N. Radiological evaluation of intertrochanteric fracture fixation by the proximal femoral nail. Injury 2012;43:856-63. [Crossref] [PubMed]
- Folsom AR, Lutsey PL, Heckbert SR, Cushman M. Serum albumin and risk of venous thromboembolism. Thromb Haemost 2010;104:100-4. [Crossref] [PubMed]
- Phillips A, Shaper AG, Whincup PH. Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 1989;2:1434-6. [Crossref] [PubMed]
- Kim S, Kang S. Serum albumin levels: a simple answer to a complex problem? Are we on the right track of assessing metabolic syndrome? Endocrinol Metab (Seoul) 2013;28:17-9. [Crossref] [PubMed]
- Friedman AN, Fadem SZ. Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol 2010;21:223-30. [Crossref] [PubMed]
- Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial 2004;17:432-7. [Crossref] [PubMed]
- Law MR, Morris JK, Wald NJ, Hale AK. Serum albumin and mortality in the BUPA study. British United Provident Association. Int J Epidemiol 1994;23:38-41. [Crossref] [PubMed]
- Ronit A, Kirkegaard-Klitbo DM, Dohlmann TL, Lundgren J, Sabin CA, Phillips AN, Nordestgaard BG, Afzal S. Plasma Albumin and Incident Cardiovascular Disease: Results From the CGPS and an Updated Meta-Analysis. Arterioscler Thromb Vasc Biol 2020;40:473-82. [Crossref] [PubMed]
- Jiang C, Wang B, Li Y, Xie L, Zhang X, Wang J, Yu Y, Song Y, Liang M, Wang G, Li J, Zhang Y, Liu L, Liu C, Tang G, Huo Y, Xu X, Qin X. U-shaped association between serum albumin and development of chronic kidney disease in general hypertensive patients. Clin Nutr 2020;39:258-64. [Crossref] [PubMed]
- Famakin B, Weiss P, Hertzberg V, McClellan W, Presley R, Krompf K, Karp H, Frankel MR. Hypoalbuminemia predicts acute stroke mortality: Paul Coverdell Georgia Stroke Registry. J Stroke Cerebrovasc Dis 2010;19:17-22. [Crossref] [PubMed]
- Djoussé L, Rothman KJ, Cupples LA, Levy D, Ellison RC. Serum albumin and risk of myocardial infarction and all-cause mortality in the Framingham Offspring Study. Circulation 2002;106:2919-24. [Crossref] [PubMed]
- Reuben DB, Ferrucci L, Wallace R, Tracy RP, Corti MC, Heimovitz H, Harris TB. The prognostic value of serum albumin in healthy older persons with low and high serum interleukin-6 (IL-6) levels. J Am Geriatr Soc 2000;48:1404-7. [Crossref] [PubMed]
- Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg 2003;237:319-34. [Crossref] [PubMed]
- Miyanishi K, Jingushi S, Torisu T. Mortality after hip fracture in Japan: the role of nutritional status. J Orthop Surg (Hong Kong) 2010;18:265-70. [Crossref] [PubMed]
- Chang W, Lv H, Feng C, Yuwen P, Wei N, Chen W, Zhang Y. Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis. Int J Surg 2018;52:320-8. [Crossref] [PubMed]




