
Risk factors for stent occlusion in the treatment of May-Thurner syndrome with iliofemoral deep venous thrombosis
I read with great interest the manuscript by Kim et al. (1) that was published recently and wanted to congratulate the authors for their excellent management of patients with May-Thurner syndrome. I wanted to clarify a few points that may be of interest to our esteemed readers:
- Severity of iliac venous stenosis has not been found to correlate with the severity of venous symptoms. Similarly, the degree of iliac venous stenosis in non-thrombotic iliac venous lesions does not appear to affect stent patency (2). However, in the aforementioned study (1), symptomatology was little discussed. Symptoms were assigned in a generic way and objective data on symptomatology seemed scarce.
- The primary determinants of stented conduit patency are the presence of an adequate inflow and outflow. This remains true for venous bypasses as well as endovenous conduits (3). The inflow can be considered as a “gate keeper” of the stent (3). All stents were placed above the inguinal ligament in this series (1). This may have led to potentially inadequate treatment of inflow lesions or injuries in the common femoral vein, resulting in impaired flow and consequently an impaired patency for the stents. Stent extension across the inguinal ligament in veins appears to be a feasible prospect based on Neglen et al.’s experience from Wallstents (4) and trial data from newer dedicated nitinol venous stents.
- Although some studies have reported incomplete thrombolysis to be a negative predictor for clinical outcomes, two recent studies from our center have called that observation into question (5). Incomplete thrombectomy, as adjudged by intravascular ultrasound (IVUS), still portended clinical improvement in symptoms and longer term venous patency (5). Therefore, partial thrombectomy may actually play a role in relieving symptoms, even if it does not restore complete patency of the vessel.
- Although catheter-directed thrombolysis (CDT) is effective, we have moved away from this modality at our center due to three primary reasons: (i) potential of complications from CDT, (ii) non-availability of intensive care unit (ICU) beds due to the COVID-19 pandemic, and (iii) presence of contraindications to the use of thrombolytic agents in many patients (5). Whenever possible, our preference now is to perform mechanical thrombectomy without CDT in a single setting that obviates the utilization of an ICU bed (5). However, although some services do not adopt thrombolysis as the first line of treatment in these cases, we should be aware that it is still the treatment of choice in most vascular surgery centers.
- When available, the use of IVUS in the detection of stent malfunction is highly preferred as multiplanar venography can underdiagnose not only the presence but also the severity of underlying chronic iliac venous lesions (6,7). However, the low availability of the exam in a large number of vascular centers poses a potential problem. The use of IVUS in all patients can potentially add to the cost and reduce the sample size.
- Venous stents such as the WallstentTM (Boston Scientific, Marlborough, MA, USA) should be slightly oversized rather than undersized due to two primary reasons. Firstly, it reduces the risk of stent embolization. Secondly, it allows for aggressive hyperdilation in the future to accommodate for the potential development of stent compression and in-stent restenosis (ISR)—a ubiquitous problem with venous stents (8).
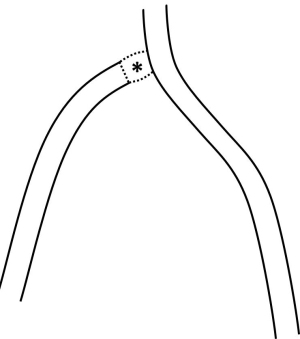
- Management of iliac-caval confluence remains a technical challenge. On the one hand, there is a risk of jailing the contralateral iliac vein orifice if the stent is extended into the inferior vena cava (IVC). On the other hand, there is risk of undertreatment if the stent is placed distally near the iliac-caval confluence. The iliac-caval confluence is a potential choke point where potential venous lesions can occur. Our modus operandi has been to use the Zenith (Z) stent at the iliac-caval confluence. This technique has several advantages—provision of stronger radial force, allowance for easier sequential bilateral stenting and avoidance of jailing of the contralateral side due to larger interstices (9). Another technique of dealing with the iliac-caval confluence is the “skip stent technique” which has been utilized by some authors without an adverse impact on stent patency (Figure 1). It involves leaving a skipped lesion at the level of iliocaval confluence (10).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-12/coif). The author has no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim MS, Park HS, Hong HP, Hyun D, Cho SK, Park KB, Shin SW, Choo SW, Do YS. Risk factors for stent occlusion after catheter-directed thrombolysis and iliac vein stenting in the treatment of May-Thurner syndrome with iliofemoral deep vein thrombosis: a retrospective cohort study. Quant Imaging Med Surg 2022;12:5420-32. [Crossref] [PubMed]
- Saleem T. Accurate and Appropriate Selection of Patients for Endovenous Iliofemoral Intervention: Are We There Yet? Eur J Vasc Endovasc Surg 2022;64:135-6. [Crossref] [PubMed]
- Saleem T. The Stent's Gatekeeper: Inflow Disease. Eur J Vasc Endovasc Surg 2022;64:738-9. [Crossref] [PubMed]
- Neglén P, Tackett TP Jr, Raju S. Venous stenting across the inguinal ligament. J Vasc Surg 2008;48:1255-61. [Crossref] [PubMed]
- Saleem T, Fuller R, Raju S. Aspiration mechanical thrombectomy for treatment of acute iliofemoral and central deep venous thrombosis. Ann Vasc Surg Brief Rep Innov 2021;1:100012. [Crossref]
- Saleem T, Raju S. Comparison of intravascular ultrasound and multidimensional contrast imaging modalities for characterization of chronic occlusive iliofemoral venous disease: A systematic review. J Vasc Surg Venous Lymphat Disord 2021;9:1545-1556.e2. [Crossref] [PubMed]
- Saleem T, Knight A, Raju S. Diagnostic yield of intravascular ultrasound in patients with clinical signs and symptoms of lower extremity venous disease. J Vasc Surg Venous Lymphat Disord 2020;8:634-9. [Crossref] [PubMed]
- Saleem T, Raju S. An overview of in-stent restenosis in iliofemoral venous stents. J Vasc Surg Venous Lymphat Disord 2022;10:492-503.e2. [Crossref] [PubMed]
- Saleem T, Raju S. Management of iatrogenic inferior vena cava perforation with composite Wallstent-Z-stent technique. J Vasc Surg Cases Innov Tech 2021;7:630-3. [Crossref] [PubMed]
- Barbati ME, Gombert A, Toonder IM, Schleimer K, Kotelis D, de Graaf R, Doganci S, Razavi MK, Jalaie H. Iliocaval Skip Stent Reconstruction Technique for Chronic Bilateral Iliocaval Venous Occlusion. J Vasc Interv Radiol 2020;31:2060-5. [Crossref] [PubMed]


