
Symptomatic free-floating thrombus in the vertebral artery: a case description
Introduction
Free-floating thrombus (FFT), also known as intraluminal thrombus, is a rare but emerging imaging marker associated with ischemic stroke (1,2). About 1.6% to 3.2% of acute ischemic stroke patients were diagnosed with FFT by computed tomography angiogram (CTA) (1). The prevalence of FFT in high-grade carotid stenosis is about 14.3% (3), while FFT in the vertebrobasilar circulation is relatively rare with an incidence rate ranging from 0.3% to 0.5% (1,4). A case series reported that FFT in the posterior circulation was associated with higher mortality compared to carotid territory (4). Atherosclerosis is considered a major cause of FFT, while other possible causes include hypercoagulable states, cardiogenic embolism events and arterial dissections (1). Currently, there is no consensus regarding the optimal treatment (medical or surgical) for FFT. Here, we describe a male patient presenting with posterior circulation ischemic stroke, in which an FFT was coincidentally found in the left vertebral artery (VA). This case is expected to help radiologists and clinicians with the early recognition and management of FFT.
Case presentation
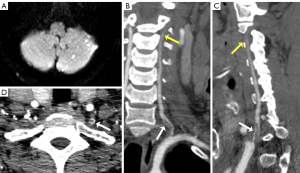
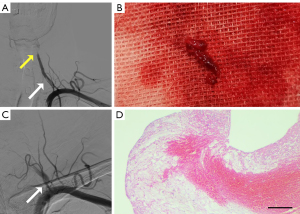
A 58-year-old male patient with no previous medical history presented to the hospital emergency department due to sudden vertigo for 10 hours. On admission, his vital signs were stable, with a recorded respiratory rate of 19 beats per minute, blood pressure of 125/74 mmHg and a pulse rate of 80 beats per minute. The neurological examination was unremarkable except for left limb ataxia. The National Institutes of Health Stroke Scale score (NIHSS) was 2 (5). Routine laboratory tests showed fasting blood glucose of 10.94 mmol/L, and remaining laboratory tests were unremarkable. Brain computed tomography (CT) showed no obvious abnormality, while magnetic resonance imaging (MRI) demonstrated restricted diffusion scattered in the left cerebellar hemisphere (Figure 1A). CTA (Figure 1B,1C) showed a long segment of strip filling defect (19.5 mm length) in the V1 segment of the left VA with V3 segment occlusion. Axial CTA (Figure 1D) showed the “donut sign” in the V1 segment of the left VA. The diagnosis of FFT in VA was made after communication with the radiologist. Arterial to arterial embolism caused by FFT was considered to be the cause of V3 occlusion of the left VA. On day 4 after symptom onset, digital subtraction angiography (DSA) further confirmed a long segment of strip filling defect in the V1 segment of the left VA with occlusion of V3 segment (Figure 2A). The patient was prepared for thrombus aspiration and further attempts to recanalize the occluded left VA by endovascular therapy. The FFT was successfully removed 14 days after onset by endovascular aspiration with a 6-F intracranial support catheter (Tonbridge, Tonbridge Medical Technology, Zhuhai, Guangzhou, China) (Figure 2B). However, the recanalization of the V3 segment of the left VA failed due to the high thrombus burden and a higher risk of developing thrombotic events, which may cause occlusion of the basilar artery and even lead to disastrous consequences. Left VA angiography showed about 50% residual stenosis at the origin of the left LV (Figure 2C). The patient had no surgical complications and was transferred to the stroke unit for close monitoring. Meanwhile, he was administered aspirin 100 mg and atorvastatin 40 mg for secondary prevention of cerebrovascular disease. His cardioembolic work-up, including transthoracic echocardiography, 12-lead electrocardiogram (ECG), and 72-hour ambulatory ECG monitoring revealed no abnormalities. Hematoxylin/eosin (HE) staining of the thrombus showed erythrocyte-rich with fibrin at the periphery (Figure 2D). At the 3-month follow-up, his symptoms were completely recovered (NIHSS score was 0), and color Doppler ultrasound of the VA also confirmed about 50% stenosis of the proximal portion of the left VA.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Two knowledge points from this clinical case are worthy of special attention: FFT, as an imaging marker associated with a high risk of early recurrent stroke, should be given attention for its early identification. The donut sign of VA axial CT angiogram plays an important role in identifying FFT.
The clinical and imaging features of stroke-related FFT in the carotid artery have been well described (2), but little is known about this condition in the posterior circulation. Currently, only case reports and case series have been published (4,6,7). Here, we describe a case of symptomatic FFT in the VA with detailed clinical and imaging findings. This case highlights the importance of CTA in the early identification of FFT, which is critical for the prompt management of these patients.
A recent study showed that 79.5% of patients with confirmed carotid FFT had carotid atherosclerotic plaque, 10% had atrial fibrillation with carotid plaque, 4% had carotid dissection, and 3.6% had embolic stroke of uncertain source (8). In addition, FFT has also been reported to be associated with coagulopathy and malignancy (1). Therefore, it is necessary to conduct an etiological workup to determine the underlying cause of the FFT, including echocardiography, long-term ECG monitoring, and hypercoagulopathy survey. In this case, we found no evidence of atrial fibrillation or coagulation abnormalities, except for type 2 diabetes. Therefore, we hypothesized that atherosclerosis may be involved in FFT formation.
The natural process of FFT varies from person to person; potential outcomes include distal embolization of the entire clot or fragments, disappearance, stabilization, or chronic progressive occlusion (9). A transcranial Doppler study conducted by Sitzer et al. suggested that patients with FFT have an increased risk of distal embolization (10). In our patient, we considered that the V3 segment occlusion of the left VA may be associated with embolism caused by shedding of the clot fragments from FFT.
In 2010, Menon et al. proposed that the “donut sign” of axial CTA is an image marker of intraluminal carotid thrombus, which is defined as an intraluminal filling defect completely surrounded by contrast on at least two consecutive layers (11). Moreover, a small prospective comparative study confirmed that the length of the filling defect in the proximal internal carotid artery extending cranially more than 3.8 mm on CTA has high sensitivity and specificity for the diagnosis of FFT (12). However, it should be noted that the donut sign of the VA is rarely described. In the case of this patient, he was initially considered to have a VA dissection by radiologists. In the event of a VA dissection, endovascular thrombectomy may worsen the tear. After discussion with the neurologist, the diagnosis of FFT was mainly based on the donut sign of CTA, which was finally confirmed by DSA and endovascular aspiration. Hence, the donut sign is useful for clinicians to recognize FFT and make a correct intervention.
At present, most studies on the treatment of patients with FFT have focused on the carotid system. However, there is no consensus on the standard treatment strategy for patients with FFT. Patients with FFT are associated with a high short-term risk of ischemic stroke recurrence (13), which may be due to clot dislocation, hypoperfusion, or total vessel occlusion caused by FFT. Theoretically, single antiplatelet or dual antiplatelet agents, anticoagulation, carotid endarterectomy (CEA), or endovascular therapy may be potential therapies to prevent stroke recurrence in patients with FFT, but the optimal approach remains unclear due to a lack of high-quality evidence. Singh et al. showed that patients with symptomatic carotid FFT have a favorable clinical prognosis with a high rate of thrombus resolution and low stroke recurrence when treated with heparin combined with single antiplatelet drug therapy (1). However, a systematic review analysis concluded that anticoagulation therapy did not show a significant advantage in reducing the risk of recurrent stroke or death in patients with FFT compared with carotid interventions (2). The timing of carotid revascularization is also controversial, with some experts suggesting that delaying surgery is preferable due to the higher risk of stroke associated with early intervention (3,13). Nevertheless, a recent study showed that early endovascular treatment significantly improved 90-day functional outcomes in patients with acute large vessel occlusion with FFT (14). Recently, Al-Jehani et al. reported a successful case of endovascular therapy for an asymptomatic FFT in VA (7), which we considered when deciding to execute endovascular aspiration and try to recanalize the occluded left VA. However, we had to give up continuing the operation owing to repeated failed thrombus aspiration with a high thrombus burden and potential complications. Fortunately, the prognosis of this patient was excellent. From this point of view, the recanalization of the left VA may not be necessary because the normal blood flow of the contralateral VA compensates for the blood supply of the ipsilateral VA. Therefore, individual treatment programs according to the specific clinical situations of each case may be an effective strategy to treat FFT.
In conclusion, this case demonstrates the rare pathogenesis of ischemic stroke caused by FFT in VA. The donut sign should be paid attention to in patients suspected of FFT in VA. Early identification of FFT is critical for the initiation of individualized treatment.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1064/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Singh RJ, Chakraborty D, Dey S, Ganesh A, Al Sultan AS, Eesa M, Wong JH, Goyal M, Hill MD, Menon BK. Intraluminal Thrombi in the Cervico-Cephalic Arteries. Stroke 2019;50:357-64. [Crossref] [PubMed]
- Fridman S, Lownie SP, Mandzia J. Diagnosis and management of carotid free-floating thrombus: A systematic literature review. Int J Stroke 2019;14:247-56. [Crossref] [PubMed]
- Iwata T, Mori T, Tajiri H, Miyazaki Y, Nakazaki M. Safety and effectiveness of emergency carotid artery stenting for a high-grade carotid stenosis with intraluminal thrombus under proximal flow control in hyperacute and acute stroke. J Neurointerv Surg 2013;5:40-4. [Crossref] [PubMed]
- Buchan A, Gates P, Pelz D, Barnett HJ. Intraluminal thrombus in the cerebral circulation. Implications for surgical management. Stroke 1988;19:681-7. [Crossref] [PubMed]
- Lyden P, Brott T, Tilley B, Welch KM, Mascha EJ, Levine S, Haley EC, Grotta J, Marler J. Improved reliability of the NIH Stroke Scale using video training. NINDS TPA Stroke Study Group. Stroke 1994;25:2220-6. [Crossref] [PubMed]
- Alhashim A, Hadhiah K, Itani SA, Alshurem M, Alabdali M, Aljaafari D, AlQarni M. Management of Free-Floating Thrombus in the Vertebral Artery in a Middle-Aged Smoker with Secondary Polycythemia Vera. Int Med Case Rep J 2021;14:663-8. [Crossref] [PubMed]
- Al-Jehani H, Alhamid MA, Alkhalaf Y, Alabbas F. A Case of Coincidental Free Floating Thrombus in the Vertebral Artery in a Patient Presenting with an Anterior Circulation Stroke and Literature Review. Neurointervention 2020;15:144-53. [Crossref] [PubMed]
- Dowlatshahi D, Lum C, Menon BK, Bharatha A, Dave P, Puac-Polanco P, Blacquiere D, Stotts G, Shamy M, Momoli F, Thornhill R, Lun R, Torres C. Aetiology of extracranial carotid free-floating thrombus in a prospective multicentre cohort. Stroke Vasc Neurol 2022; Epub ahead of print. [Crossref] [PubMed]
- Yarnell P, Earnest M, Kelly G, Sanders B. Disappearing carotid defects. Stroke 1978;9:258-62. [Crossref] [PubMed]
- Sitzer M, Müller W, Siebler M, Hort W, Kniemeyer HW, Jäncke L, Steinmetz H. Plaque ulceration and lumen thrombus are the main sources of cerebral microemboli in high-grade internal carotid artery stenosis. Stroke 1995;26:1231-3. [Crossref] [PubMed]
- Menon BK, Singh J, Al-Khataami A, Demchuk AM, Goyal MCalgary CTA Study Group. The donut sign on CT angiography: an indicator of reversible intraluminal carotid thrombus? Neuroradiology 2010;52:1055-6. [Crossref] [PubMed]
- Jaberi A, Lum C, Stefanski P, Thornhill R, Iancu D, Petrcich W, Momoli F, Torres C, Dowlatshahi D. Computed tomography angiography intraluminal filling defect is predictive of internal carotid artery free-floating thrombus. Neuroradiology 2014;56:15-23. [Crossref] [PubMed]
- Vellimana AK, Kadkhodayan Y, Rich KM, Cross DT 3rd, Moran CJ, Zazulia AR, Lee JM, Chicoine MR, Dacey RG Jr, Derdeyn CP, Zipfel GJ. Symptomatic patients with intraluminal carotid artery thrombus: outcome with a strategy of initial anticoagulation. J Neurosurg 2013;118:34-41. [Crossref] [PubMed]
- Ding Y, Leng X, Nie X, Pan Y, Li J, Liu D, et al. Intraluminal Thrombus and Outcomes of Patients With Acute Large Vessel Occlusive Stroke Undergoing Endovascular Treatment. Stroke 2021;52:1473-7. [Crossref] [PubMed]


