
Biostatistical evaluation of the effectiveness of fetal ultrasound diagnostics with application of new uncertainty factor and difficulty factor in cases of craniofacial malformations—gray zone in biostatistics for imaging procedures
Introduction
In medical science, traditional biostatistics deals with measured values or clearly distinct groups. It is problematic how to approach or ignore uncertainties, it either classifies them as negative or positive, or excludes them from further testing. In imaging procedures [ultrasound (US), X-ray, computed tomography (CT), magnetic resonance (MR)] we often encounter cases where the imaging recognizes that there is some alteration in the organ, but the final diagnosis does not match the diagnosis raised by the imaging.
In obstetric practice, in the course of ultrasound examinations during pregnancy, we often encounter the fact, that in the intrauterine fetus it is recognized, that an abnormality occurs in a given organ system, but the neonatological and pathological examinations after birth or abortion give another diagnosis. In most of the statistical processes, these cases in the “uncertain” gray zone are classified as unrecognized in the majority of publications. For biostatistics, therefore, valuable cases are lost. It is difficult to examine the subsequent development of a given diagnostic procedure (in this particular case, fetal ultrasound), to analyze later improvements in its effectiveness, to characterize the complexity of the examination method and to follow the changes.
Our aim was to develop a method to characterize the cases belonging to the so-called gray zone, making these cases worth evaluating. Subsequent changes can be analyzed. The new categories we introduce will explore the possibilities of further statistical analysis of cases in the gray zone. We can assess the uncertainty and difficulty of the tests (examinations) with them.
To demonstrate the novel biostatistical method, we investigated craniofacial disorders, which are often difficult during obstetric prenatal ultrasound examinations.
The prevalence rate of the all fetal malformations at birth is not rare, about 20–33/1,000 live birth (1-4). Malformations of the face and neck are relatively rare and their prevalence rate at birth is 1–2/1,000 live birth (4,5). Among them, the prevalence rate at birth of cleft lip and/or palate is about 1/1,000 (6-9). Facial and neck malformations are often associated with abnormalities of other organ systems and genetic disorders, most often with cerebral malformations (10-13). Malformations are screened during the prenatal period by ultrasound examinations. The sensitivity of the ultrasound in diagnosing facial and neck disorders varies widely (4,5,14,15).
In our study, our goal was to test the effectiveness of the prenatal ultrasound diagnostics in detecting the craniofacial malformations and to examine the proportion of partially recognized cases (gray zone).
Methods
In a prospective study, covering the data of a 12-year period at the 1st Department of Obstetrics and Gynecology, we have processed those cases where craniofacial malformations were diagnosed during the fetopathological or postnatal examinations. Prenatal ultrasound findings, postnatal clinical data, and fetopathological findings were processed.
The patients were divided into three groups: Group I: prenatal ultrasound examination and postnatal/fetopathological test results showed full matches (so the anomaly was fully recognized); Group II: facial and neck malformations were only partially detected; Group III: prenatal diagnosis failed to detect the malformations (true false negative cases).
Facial and neck malformations representing part of certain non-chromosomal multiple malformations or associated with chromosomal aberrations and cases where the disorders were not associated with other organ system malformations were studied separately. In the interest of literature data comparability, the abnormalities were grouped considering the criteria of EUROCAT guidelines.
The sonographic examinations were performed at the Ultrasound Laboratory of the 1st Department of Obstetrics and Gynecology using Philips® HD 11XE (Philips Ultrasound), GE Voluson® 730PRO (GE Medical System Kretztechnik GmbH & Co. OHG) and Medison SA9900 (Medison Co., LTD) ultrasound devices.
In assessing the effectiveness of fetal ultrasound diagnostics, international publications use the recognized and unrecognized category. However, we often encounter cases where the ultrasound examination recognizes the abnormalities of the particular organ system, but does not give a definitive diagnosis, and the postnatal/post abortion (post-pregnancy) tests give a different diagnosis. In these cases, we cannot say that the ultrasound did not recognize that there was a difference, only the diagnosis was not the same in the prenatal ultrasound and the neonatological/pathological/fetopathological examinations. We have introduced the “Partially Recognized” category to characterize these cases. Those cases were considered partially recognized where the abnormality of the particular organ was detected during the ultrasound examination, but the final diagnosis was different on the basis of the examinations performed after birth/abortion, compared to the presumed diagnosis. As an example, we can adduce the cerebral abnormalities when the ultrasound examinations depicted enlargement of the lateral ventricles or cerebral ventricular formal deviation, but postnatal tests have confirmed corpus callosum agenesis/dysgenesis.
By introducing the Uncertainty Factor, we were able to examine the ratio of the number of partially recognized to the somewhat (partially or totally) recognized ratio: Uncertainty Factor F (U) = P (Partially Recognized)/[P (Partially Recognized) + T (Totally Recognized)].
The sonographic examinations were conducted according to the professional protocols elaborated by the Hungarian Society of Obstetric and Gynecological Ultrasonography.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The work has been approved by the Ethics Committee of the Semmelweis University (Scientific Research Ethics Committee permission number: SE-TUKEB 231). Patients’ parents or legal guardians gave written informed consent to our work.
In statistical procession calculating significance the Chi-square test was used. In case of P<0.05, the anomaly was considered as statistically significant.
Results
At Semmelweis University at the 1st Department of Obstetrics and Gynaecology 41,069 newborns were delivered, and 13,491 abortions [spontaneous or termination of pregnancy (TOP)] occurred over the 12-year period. A total of 218 fetuses had some kind of craniofacial abnormality. During the reviewed period the prevalence of facial and neck malformations was 5.31/1,000 live birth. Among the 218 fetuses there were 105 boys and 101 girls, in 12 cases the sex was undetermined. The average maternal age was 31.43±6.25 years at the time of the childbirth/abortion.
Totally 123 out of 218 cases the pregnancy ended in childbirth, while in 95 cases abortion occurred. In 2 cases spontaneous miscarriage occurred, and the abortion was induced in cases of 93 fetuses.
In 78 out of 218 fetuses, the facial and neck malformation occurred by itself, in 33 cases associated with chromosomal abnormalities, and in 107 cases appeared as part of a multiplex malformation.
Prenatal ultrasound diagnosis of fetuses with facial and neck malformations completely coincided in 71/218 cases (32.6%) with postnatal/fetopathological findings. In 31/218 cases (14.2%) the detection was only partial, while in 116/218 cases, no craniofacial malformations were diagnosed prenatally (53.2%) (Table 1).
Table 1
| Type of abnormalities | Cases | I. Totally Recognized | II. Partially Recognized | II. Not Recognized | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Isolated craniofacial abnormalities | 78 | 31 | 39.7 | 7 | 9.0 | 40 | 51.3 | ||
| Associated with chromosome abnormalities | 33 | 14 | 42.4 | 7 | 21.2 | 12 | 36.4 | ||
| Part of multiple malformation (non-chromosomal) | 107 | 26 | 24.3 | 17 | 15.9 | 64 | 59.8 | ||
| Total | 218 | 71 | 32.6 | 31 | 14.2 | 116 | 53.2 | ||
In 78 cases, the craniofacial malformation was not associated with disorders of any other organs, the results of prenatal sonography tests and postnatal/post abortion examinations completely coincided in 31 fetuses (39.7%), in 7 cases (9.0%) the prenatal discovery was partial, while in 40 cases (51.3%) no malformation was detected prenatally.
The facial/neck abnormality appeared as part of a multiplex malformation in 107 cases, in 26 fetuses (24.3%) there was complete coincidence between the prenatal diagnosis and the postnatal/post abortion findings, in 17 cases the match was partial (15.9%), while in 64 fetuses (59.8%) no deviation was detected. In 57 out of 107 cases, two organ systems were affected by the detected anomalies, in 50 cases the number of affected organ systems was ≥3. The associated malformations were most commonly craniospinal malformations (47 cases), cardiovascular malformations [38], limb (extremities) disorders [33], urogenital abnormalities [25], and abdominal and abdominal wall malformations [20] were also detected. In 13 cases thoracic disorders, while in 8 cases fetal hydrops have occurred.
In 33 fetuses, the craniofacial malformation was associated with chromosomal abnormalities, in 14 cases there was trisomy 21 (Down syndrome), in 8 cases there was trisomy 13 (Patau’s syndrome), in 7 cases trisomy 18 (Edwards’s syndrome), in 2 cases there was X monosomy (Turner syndrome), in 1 case trisomy 9 and in 1 cases 22 ring chromosome were present. In 14 out of 33 fetuses (42.4%) the prenatal ultrasonography fully detected the facial/neck malformations, in 7 cases the discovery was partial (21.2%), and in 12 cases no malformation was recognized (36.4%).
Among the 218 cases of fetal craniofacial malformations, 195 cases were single, and 21 cases of twin and 2 trigemini pregnancies. In all twin and trigemini cases, only one fetus was affected by the craniofacial malformation.
A total of 242 facial and neck malformations were detected in the 218 fetuses, the differences were divided into different groups (Table 2). The cleft lip and/or palate (107 cases), micrognathia (29 cases) and choanal atresia were the most common malformation groups (26 cases). In 11 cases microphthalmos/anophthalmos, in 5 cases proptosis, while in 9 cases absent ears or deformed ears was diagnosed. Forty-five cases were included in the group of other craniofacial malformations (Table 3).
Table 2
| Type of anomalies | Cases | I. Totally Discovered | II. Partially Discovered | III. Not Detected | Uncertainty Factor F (U)* | Difficulty Factor F (D)* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | II/I + II | III/I + II | ||||||
| Abnormalities of the lip and palate, oral cavity | |||||||||||||
| Cleft lip and/or palate | 107 | 43 | 40.19 | 18 | 16.82 | 46 | 42.99 | 0.30 | 0.75 | ||||
| Cleft lip | 16 | ||||||||||||
| Cleft palate | 17 | ||||||||||||
| Cleft lip and palate | 74 | ||||||||||||
| Micrognathia | 29 | 7 | 24.14 | 6 | 20.69 | 16 | 55.17 | 0.46 | 1.23 | ||||
| Other | 10 | 2 | 20.00 | 0 | 0.00 | 8 | 80.00 | 0.00 | 4.00 | ||||
| Orbital abnormalities | |||||||||||||
| Microphthalmos/anophthalmos | 11 | 3 | 27.27 | 1 | 9.09 | 7 | 63.64 | 0.25 | 1.75 | ||||
| Proptosis | 5 | 2 | 40.00 | 0 | 0.00 | 3 | 60.00 | 0.00 | 1.50 | ||||
| Other | 4 | 1 | 25.00 | 0 | 0.00 | 3 | 75.00 | 0.00 | 3.00 | ||||
| Ear disorders | |||||||||||||
| Absent ear/dysplasia | 9 | 0 | 0.00 | 1 | 11.11 | 8 | 88.89 | 1.00 | 8.00 | ||||
| External auditory canal agenesis/dysgenesis | 3 | 0 | 0.00 | 0 | 0.00 | 3 | 100.00 | ||||||
| Other | 5 | 0 | 0.00 | 0 | 0.00 | 5 | 100.00 | ||||||
| Disorders of the nose and nasal bone | |||||||||||||
| Choanal atresia/stenosis | 26 | 0 | 0.00 | 2 | 7.69 | 24 | 92.31 | 1.00 | 12.00 | ||||
| Proboscis | 7 | 1 | 14.29 | 1 | 14.29 | 5 | 71.43 | 0.50 | 2.50 | ||||
| Other | 7 | 2 | 28.57 | 2 | 28.57 | 3 | 42.86 | 0.50 | 0.75 | ||||
| Other neck disorders | 11 | 6 | 54.55 | 2 | 18.18 | 3 | 27.27 | 0.25 | 0.38 | ||||
| Craniofacial tumors | 8 | 5 | 62.50 | 1 | 12.50 | 2 | 25.00 | 0.17 | 0.33 | ||||
| Total | 242 | 72 | 29.75 | 34 | 14.05 | 136 | 56.20 | 0.32 | 1.28 | ||||
*, <0.25 (low); 0.25≥ medium <0.5; 0.5≥ high <1; ≥1 (very high).
Table 3
| Type of anomalies | Cases | I. Totally Discovered | II. Partially Discovered | III. Not Detected | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Abnormalities of the lip and palate, oral cavity | 10 | 2 | 20.00 | 0 | 0.00 | 8 | 80.00 | ||
| Macroglossia | 9 | ||||||||
| Tongue hypoplasia | 1 | ||||||||
| Orbital abnormalities | 4 | 1 | 25.00 | 0 | 0.00 | 3 | 75.00 | ||
| Aphakia (absence of eye lens) | 1 | ||||||||
| Cyclopia | 1 | ||||||||
| Dacryocystocele (benign tear duct tumor) | 2 | ||||||||
| Ear disorders | 5 | 0 | 0.00 | 0 | 0.00 | 5 | 100.00 | ||
| Preauricular fibroma | 4 | ||||||||
| Eardrum polyposis | 1 | ||||||||
| Disorders of the nose and nasal bone | 7 | 2 | 28.57 | 2 | 28.57 | 3 | 42.86 | ||
| Wide, flat nasal bridge | 5 | ||||||||
| Compressed nasal bridge | 2 | ||||||||
| Other neck disorders | 11 | 6 | 54.55 | 2 | 18.18 | 3 | 27.27 | ||
| Pterygium colli | 2 | ||||||||
| Lymphangiectasia regionalis collis | 1 | ||||||||
| Cervical cyst | 7 | ||||||||
| Laryngeal disorder | 1 | ||||||||
| Craniofacial tumors | 8 | 5 | 62.50 | 1 | 12.50 | 2 | 25.00 | ||
| Craniopharyngioma | 1 | ||||||||
| Tumor capitis | 2 | ||||||||
| Tumor on the neck | 1 | ||||||||
| Epidermoid cyst capitis | 1 | ||||||||
| Oral cavity tumor | 1 | ||||||||
| Epignathus (teratoma) | 2 | ||||||||
| Total | 45 | 16 | 35.56 | 5 | 11.11 | 24 | 53.33 | ||
Table 2 shows the sensitivity of detection in certain groups. Out of the 242 facial/neck malformations, 72 has been completely detected antenatally (29.75%), while 34 cases partially (14.05%), and 136 cases (56.2%) not at all. We could detect with high sensitivity the cleft lip and/or palate (40.19%), while the effectiveness of the ultrasound was low in the groups of choanal atresia (0%), absent ears (0%). The effectiveness of the ultrasound was moderate in cases of micrognathia (24.14%), microphthalmos/anophthalmos (27.27%), exophthalmos (40%), proboscis (14.29%) and in cases of other craniofacialis malformations (35.56%).
Table 2 shows the Uncertainty Factor F (U) and the Difficulty Factor F (D), introduced by us. When examining facial and neck malformations, the Difficulty Factor was high or very high in almost each disorder group, with a cumulative score of 1.28. The Difficulty factor was medium in other neck disorders (0.38) and in craniofacial tumors (0.33).
The Uncertainty Factor was medium in cases of cleft lip and/or palate (0.33), micrognathia (0.46), microphthalmos/anophthalmos (0.25), other neck abnormalities (0.25), and it was high in cases of proboscis and other nose and nasal bone disorders, and it was very high in cases of choanal atresia/stenosis (1.0) and in cases of absent ear/dysplasia of ear (1.0). The Uncertainty Factor cumulative score was 0.32.
Discussion
Applying the Uncertainty Factor F (U) and the Difficulty Factor F (D)
The purpose of this paper was to introduce the use of the Uncertainty Factor F (U) and the Difficulty Factor F (D) we introduced. The use of the two factors, the Uncertainty Factor F (U) and the Difficulty Factor F (D), is considered when a given diagnostic imaging procedure is inconclusive in diagnosing a particular abnormality in the organ system, but recognizes that there is a difference in the particular organ system. The “Partially Recognized” category was used in these cases. The introduction of the category is recommended because during imaging procedures, such as prenatal ultrasound in obstetrics, we often encounter cases where the ultrasound examiner, although he/she sees a difference in the particular organ system, due to its “difficulty” and “uncertainty”, a particular anomaly is not clearly recognized. Only postnatal or post abortion follow-up, pathological and fetopathological examinations can determine the exact diagnosis. This problem is often encountered in obstetric practice.
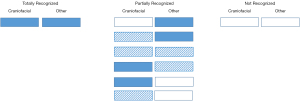
The “Partially Recognized” category is easy to apply for singular fetal abnormalities (Figure 1).

There is difficulty in using the “Partially Recognized” category in those cases where two or more ultrasound differences are depicted in the fetus. In such cases, there are a number of variations in the “Partially Recognized” category (see Figure 2) even in case of two deviations. In our example, a craniofacial deviation is associated with another organ system difference. If we want to consider the effectiveness of the ultrasonography for both organ systems, then “Totally Recognized” will be the case, if the differences in both organ systems were totally recognized, and it will be in the “Not Recognized” category if none of the organ system differences were detected. Accordingly, the case could be classified in the “Partially Recognized” category, if the difference in one of the organ systems was not or only partially recognized, and the difference in the other organ system was partially or completely recognized. These variations are listed in Figure 2.
Taking into account the above difficulties in classification, we have decided to examine the organ systems individually. Abnormalities were classified into six main organ system groups: craniospinal disorders, craniofacial disorders, heart and chest disorders, abdominal and abdominal wall disorders, urogenital disorders, limb and ossification disorders.
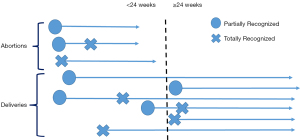
Analyzing the dynamics of ultrasonic scan detection of the anomalies during pregnancy, we encountered a number of cases in which the organ system disorder has only been partially detected in the prenatal ultrasound, and the particular disorder only during postpartum/post abortion tests. In some cases, the abnormalities of the given organ system have been fully recognized, accordingly the prenatal diagnosis was consistent with the postpartum or post abortion fetopathological diagnosis. However, there were cases where initially the abnormalities of the particular organ system were only partially recognized, and a successful diagnosis was only set up in one of the repeated ultrasound examinations performed later during pregnancy (Figure 3). The question was: how to classify these latter cases? For the purpose of statistical processing, as a correct diagnosis was made during the ultrasound examination performed during pregnancy—even if not the first time the organ system disorder arose—these cases were classified into the “Totally Recognized” category. Subsequently we plan to process the time between the partial recognition and the total recognition (delta t).
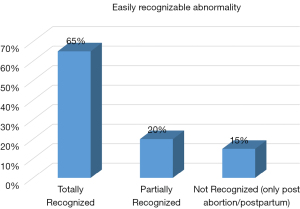
Some of the abnormalities are well recognizable during the prenatal ultrasound examinations (Figure 4). Most of them are fully recognized during the prenatal ultrasound scans. However, there are fetal abnormalities that are not characteristic of this.
In the case of some disorders, although it is recognized that there is an anomaly in the organ system, it is only partially recognized in a higher proportion during prenatal ultrasound examination (Figure 5).
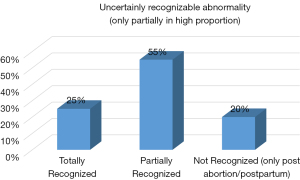
We have developed the Uncertainty Factor parameter to characterize these disorders. For the Uncertainty Factor F (U), the number of “Partially Recognized” cases was divided by the sum of “Totally Recognized” and “Partially Recognized” cases. So with this parameter, we examined how many percent of the detected cases were “only” “Partially Recognized”.
In brief:
where: P (n)—number of Partially Recognized cases; T (n)—number of Totally Recognized cases.
Some abnormalities are not recognized during prenatal ultrasound scans at a higher rate, and only postpartum/post abortion examinations reveal them (Figure 6).
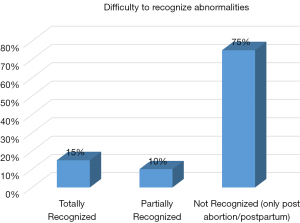
We introduced the Difficulty Factor parameter to characterize these cases. For the Difficulty Factor F (D), the number of “Not Recognized” cases was divided by the sum of “Totally Recognized” and “Partially Recognized” cases. With this second parameter, we investigated how the number of unrecognized cases was related to the number of detected cases.
In brief:
where: N (n)—number of Not Recognized cases; P (n)—number of Partially Recognized cases; T (n)—number of Totally Recognized cases.
When calculating the Uncertainty and the Difficulty factors, the value was considered low if it was less than 0.25, the value was considered medium if it was greater or equal to 0.25, but less than 0.5, and high if it was greater or equal to 0.5, but less than 1. The value was considered very high if it was greater or equal to 1.
The Uncertainty Factor was medium in cases of cleft lip and/or palate (0.3), micrognathia (0.46), microphthalmos/anophthalmos (0.25), and in cases of other neck disorders (0.25). The Uncertainty Factor was high in cases of proboscis (0.5) and other disorders of the nose and nasal bone (0.5), and was very high in cases of absent ear/dysplasia (1.0) and choanal atresia/stenosis (1.0).
When examining craniofacial disorders, the Difficulty Factor was high and very high in almost each group of disorders, well characterizing the difficulty of examining craniofacial disorders.
The Difficulty Factor was very high in the micrognathia (1.23), in cases of other abnormalities of the lip and palate and oral cavity (4.0), in the microphthalmos/anophthalmos (1.75), in the exophthalmus cases (1.5), and other orbital abnormalities (3.0), in cases of absent ear/dysplastic ear (8.0), in choanal atresia/stenosis (12.0), and proboscis (2.5). The lowest but still high Difficulty Factor score was found in the cleft lip and/or palate cases (0.75), and in other disorders of the nose and nasal bone (0.75). The Difficulty factor was medium in cases of other neck disorders (0.38), and in cases craniofacial tumors (0.33).
In the case of fetal abnormalities, which were very difficult to examine, a high Difficulty Factor and a high Uncertainty Factor were observed, such as choanal atresia. For choanal atresia, both the Uncertainty Factor (1.0) and the Difficulty Factor (12.0) were very high.
Prevalence
In our study, the birth prevalence of facial and neck malformations was 5.31/1,000 live birth. This significantly exceeded the prevalence data of 2.2/1,000 in Levi et al. study (5). In our study, cleft lip and/or palate was the most commonly found disorder among the craniofacial malformations, with a birth prevalence of 2.6/1,000. This exceeded the data of Mossey et al. (1.8/1,000), and it was significantly higher than the results of Stoll et al. (1.16/1,000) and of Fadda et al. (1.14/1,000) (6,10,16).
The significantly higher birth prevalence measured in our Clinic can be partly caused by the fact, that this is a central patient care clinic, so we meet proportionally more disorders than an average hospital.
Sensitivity
Out of the 242 craniofacial malformations 72 has been completely detected antenatally (29.75%), while 34 cases partially (14.05%), and 136 cases (56.2%) not at all. Levi used the data of 36 communications in his summary report, and there was a 55% cumulative efficacy in detecting facial and neck malformations within the uterus, which significantly exceeded our sensitivity data (4). Saltvedt et al. also found a better, 100% efficiency at both the 12th week and the 18th week ultrasound screen examinations in cases of neck, eye, mouth and ear malformations (15).
In our study, the highest sensitivity rate was found at the detection of cleft lip and/or palate at 40.19%. Fadda and his research team were able to detect cleft lip and /or palate before week 24 with a higher efficiency of 70.8% (6). VanDorsten et al., although in a smaller number of cases, but managed to diagnose the cleft lip and/or and palate until week 22 (3).
Chromosomal abnormalities
In our study 33 fetuses had chromosome abnormalities (15.14%). There were 13 cases of cleft lip and/or palate associated with chromosomal abnormalities, 7 cases of Patau’s syndrome, 3 cases of Edward’s syndrome, and 1 case of trisomy 9 and 1 case of 22 ring chromosome. It is known that Patau’s syndrome is commonly associated with the appearance of cleft lip and/or palate, which has been confirmed by several studies, as well as ours. Perrotin et al. found trisomy 13 in 8 out of 62 fetuses with cleft lip and/or palate (12.9%) (17). When cleft lip and/or palate occurred, Stoll et al. found chromosomal abnormalities in 8.74%, Clementi et al. in 10.12% of the cases most often trisomy 13 (10,18). In our study, in cases of cleft lip and/or palate, the occurrence of chromosomal abnormalities was 10%, similarly to the above mentioned studies.
Non-chromosomal multiple malformations
In our study, in 107 cases of craniofacial malformations, other organ systems were affected as well (49.1%). Craniospinal abnormalities were associated most often, in more than half of the cases of multiple malformations. Nicolaides et al. found 55% of multiple malformations in cases of craniofacial abnormalities, which is practically the same as our results, and in our study, the most common deviation of brain and spinal cord associated with facial anomaly (11).
In our study, among the groups of individual disorders, other organ systems were affected at the highest rate in the cleft lip and/or palate and the choanal atresia groups: 48.6% (52/107) fetuses were affected in the former, and 34.61% (9/26) fetuses in the latter. Most commonly (approximately 50%) cerebral malformations occurred in both groups. Similarly to our results, in case of choanal atresia Ferrarini et al. found other organ systems affected in 50%. In case of cleft lip and/or palate, Clementi et al. and Stoll and his research team found lower association rates, 26.63% and 23.94%, respectively (10,12,18). As in our study, Perrotin et al. also found that the associated malformations were most commonly craniospinal malformations in 45% of cleft lip and/or palate cases (17).
It was interesting to observe during the examination that if the craniofacial malformation occurred alone, the abnormality was detected in a higher proportion than in those fetuses where the abnormality occurred as part of multiple malformation. Out of the 107 euploid fetuses with multiple malformations, in 26 cases the abnormalities were completely detected antenatally (24.3%), while out of the 78 cases with isolated craniofacial malformations, we could detect it in 31 fetuses (39.7%) before birth/abortion. Our results could be explained by the fact that in cases where the major disorder of another organ system was present, the milder facial and neck disorders were less well-diagnosed.
Early detection
As technology advances, the malformations become detectable much earlier, even on the 11th–14th weeks of pregnancy (15). Early detection of craniofacial abnormalities is of great importance for several reasons. On the one hand, early diagnosis allows families to make informed and prudent decisions about the fate of the pregnancy, and if they decide to keep the pregnancy, they can prepare for the arrival of the sick newborn (19).
On the other hand, the early detection of facial and neck malformations in many cases can be crucial to the outcome of pregnancy, and in some cases a non-life-threatening deviation may even draw attention to an unrecognized chromosomal abnormality (10,11).
The 3-D ultrasound can be used to analyze the face of the fetus more accurately, which can be up to 100% effective in detecting the cleft lip and/or palate (20,21).
Conclusions
The detection of facial and neck malformations was low in efficiency (29.75%). Postnatally/post abortion and prenatally diagnosed fetal facial and neck malformations coincided only in about one-third of the cases. Our results have confirmed that fetal ultrasound examination plays an important role in diagnosing craniofacial malformations, however, it does not allow the detection of most of the malformations. We could conclude that fetal cleft lip and/or palate can be detected with high efficiency in fetuses in utero, while in cases of other abnormalities the ultrasound efficiency is low. Being aware of the above is important for experts performing the ultrasound examinations, health professionals providing genetic counselling and prenatal care and, also, neonatologists and paediatricians seeing newborns. During prenatal care, the expectant mother should be given adequate information about the sensitivity of the examinations. If the malformation is detected postnatally, the couple should be informed how reliably the specific malformation is detectable by prenatal sonography.
We have introduced the Uncertainty Factor F (U) and Difficulty Factor F (D), they characterized the difficulties of the prenatal ultrasound examinations well. We got high values in the cases of craniofacial malformations, belonging to the abnormalities more difficult to detect, based on the literature data.
Acknowledgments
The authors are thankful to Kutasi Aniko and Glovocz Bea genetic assistants for their valuable technical help.
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1074/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Boyd PA, Haeusler M, Barisic I, Loane M, Garne E, Dolk H. Paper 1: The EUROCAT network--organization and processes. Birth Defects Res A Clin Mol Teratol 2011;91:S2-15. [Crossref] [PubMed]
- Crane JP, LeFevre ML, Winborn RC, Evans JK, Ewigman BG, Bain RP, Frigoletto FD, McNellis D. A randomized trial of prenatal ultrasonographic screening: impact on the detection, management, and outcome of anomalous fetuses. The RADIUS Study Group. Am J Obstet Gynecol 1994;171:392-9. [Crossref] [PubMed]
- VanDorsten JP, Hulsey TC, Newman RB, Menard MK. Fetal anomaly detection by second-trimester ultrasonography in a tertiary center. Am J Obstet Gynecol 1998;178:742-9. [Crossref] [PubMed]
- Levi S. Ultrasound in prenatal diagnosis: polemics around routine ultrasound screening for second trimester fetal malformations. Prenat Diagn 2002;22:285-95. [Crossref] [PubMed]
- Levi S, Hyjazi Y, Schaapst JP, Defoort P, Coulon R, Buekens P. Sensitivity and specificity of routine antenatal screening for congenital anomalies by ultrasound: the Belgian Multicentric Study. Ultrasound Obstet Gynecol 1991;1:102-10. [Crossref] [PubMed]
- Fadda GM, Capobianco G, Balata A, Litta P, Ambrosini G, D'Antona D, Cosmi E, Dessole S. Routine second trimester ultrasound screening for prenatal detection of fetal malformations in Sassari University Hospital, Italy: 23 years of experience in 42,256 pregnancies. Eur J Obstet Gynecol Reprod Biol 2009;144:110-4. [Crossref] [PubMed]
- FitzPatrick DR, Raine PA, Boorman JG. Facial clefts in the west of Scotland in the period 1980-1984: epidemiology and genetic diagnoses. J Med Genet 1994;31:126-9. [Crossref] [PubMed]
- Derijcke A, Eerens A, Carels C. The incidence of oral clefts: a review. Br J Oral Maxillofac Surg 1996;34:488-94. [Crossref] [PubMed]
- Stoll C, Dott B, Alembik Y, Roth M. Evaluation of prenatal diagnosis of cleft lip/palate by foetal ultrasonographic examination. Ann Genet 2000;43:11-4. [Crossref] [PubMed]
- Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in cases with oral clefts. Cleft Palate Craniofac J 2000;37:41-7. [Crossref] [PubMed]
- Nicolaides KH, Salvesen DR, Snijders RJ, Gosden CM. Fetal facial defects: associated malformations and chromosomal abnormalities. Fetal Diagn Ther 1993;8:1-9. [Crossref] [PubMed]
- Ferrarini A, Osterheld MC, Vial Y, de Viragh PA, Cotting J, Martinet D, Beckmann JS, Fellmann F. Familial occurrence of an association of multiple intestinal atresia and choanal atresia: a new syndrome? Am J Med Genet A 2009;149A:2661-5. [Crossref] [PubMed]
- Goodacre T, Swan MC. Cleft lip and palate: current management. Paediatr Child Health 2008;22:283-92. [Crossref]
- Boyd PA, Rounding C, Chamberlain P, Wellesley D, Kurinczuk JJ. The evolution of prenatal screening and diagnosis and its impact on an unselected population over an 18-year period. BJOG 2012;119:1131-40. [Crossref] [PubMed]
- Saltvedt S, Almström H, Kublickas M, Valentin L, Grunewald C. Detection of malformations in chromosomally normal fetuses by routine ultrasound at 12 or 18 weeks of gestation-a randomised controlled trial in 39,572 pregnancies. BJOG 2006;113:664-74. [Crossref] [PubMed]
- Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet 2009;374:1773-85. [Crossref] [PubMed]
- Perrotin F, de Poncheville LM, Marret H, Paillet C, Lansac J, Body G. Chromosomal defects and associated malformations in fetal cleft lip with or without cleft palate. Eur J Obstet Gynecol Reprod Biol 2001;99:19-24. [Crossref] [PubMed]
- Clementi M, Tenconi R, Bianchi F, Stoll C. Evaluation of prenatal diagnosis of cleft lip with or without cleft palate and cleft palate by ultrasound: experience from 20 European registries. EUROSCAN study group. Prenat Diagn 2000;20:870-5. [Crossref] [PubMed]
- Ensing S, Kleinrouweler CE, Maas SM, Bilardo CM, Van der Horst CM, Pajkrt E. Influence of the 20-week anomaly scan on prenatal diagnosis and management of fetal facial clefts. Ultrasound Obstet Gynecol 2014;44:154-9. [Crossref] [PubMed]
- Bäumler M, Faure JM, Bigorre M, Bäumler-Patris C, Boulot P, Demattei C, Captier G. Accuracy of prenatal three-dimensional ultrasound in the diagnosis of cleft hard palate when cleft lip is present. Ultrasound Obstet Gynecol 2011;38:440-4. [Crossref] [PubMed]
- Martinez-Ten P, Adiego B, Illescas T, Bermejo C, Wong AE, Sepulveda W. First-trimester diagnosis of cleft lip and palate using three-dimensional ultrasound. Ultrasound Obstet Gynecol 2012;40:40-6. [Crossref] [PubMed]


