
Image quality evaluation of diffusion-weighted imaging in bladder cancer: a comparison between integrated slice-specific dynamic shimming and single-shot echo-planar imaging
Introduction
Bladder cancer (BC) is the most common malignant tumor of the urinary system and can be divided into 2 types according to the degree of muscularis propria invasion: non-muscle-invasive BC and muscle-invasive BC. Non-muscle-invasive BC is mainly treated with transurethral resection of bladder tumor. The most effective treatment of muscle-invasive BC is radical cystectomy due to its poor prognosis. Therefore, the accuracy of preoperative diagnosis of BC muscular invasion directly affects the treatment and prognosis of patients (1). Magnetic resonance imaging (MRI) has been widely used in the diagnosis and local staging of BC because it has superior soft tissue contrast that is capable of distinguishing the structure of the bladder wall without ionizing radiation. Therefore, it is important to obtain good MRI images because they will affect how well radiologists detect lesions and judge muscular invasion.
Panebianco et al. (2) designed the vesical imaging-reporting and data system. This system comprises a 5-point scale to indicate the risk of muscular invasion based on T2-weighted imaging (T2WI), diffusion-weighted imaging (DWI), and dynamic contrast-enhanced (DCE) MRI. Among them, the DWI sequence plays an instrumental role. DWI can distinguish the thickened submucosa from inflammatory changes or fibrosis beneath the tumor because this technique has superior soft tissue contrast and can reflect molecular diffusion restriction in malignant tissues. Thus, it can reduce the false-positive rates of T2WI or DCE in diagnosing muscular invasion (3). El-Assmy et al. (4) found that the accuracy of DWI was significantly higher than that of T2WI in distinguishing superficial tumors (pT1) from minimally invasive tumors (pT2; 63.6% vs. 6.1%; P< 0.001) and in overall staging (78.3% vs. 39.6%; P< 0.001). A meta-analysis reported that compared with studies using only DCE-MRI (64%), studies using only DWI-MRI (92%) had higher specificity but comparable sensitivity (86% and 90%) in differentiating T staging of BC, while studies using a 3.0T scanner and DWI sequences had the highest sensitivity (92%) and specificity (96%) among all studies (5). Previous studies have reported accuracies of BC staging on DCE-MRI ranging from 58% to 60%, but overstaging (16–32%) was the most common error (6,7). These studies indicated that DWI plays an important role in evaluating T staging of BC.
DWI reflects the Brownian motion of water molecules in living bodies. It can indirectly reflect changes in the tissue microstructure by detecting the restricted direction and degree of water molecules in vivo to diagnose the presence of diseases. Malignant tissues show much more diffusion restriction due to their dense cellularity, irregular tissue, and reduced extracellular space (8). BCs show high signal intensity (SI) on DWI and low apparent diffusion coefficient (ADC) values that restrict diffusion. When tumors invade muscularis propria, the continuous signal is interrupted.
The DWI sequence routinely adopts the single-shot echo-planar imaging (SS-EPI) technique in clinical practice. This technique is fast but is particularly sensitive to magnetic field inhomogeneity and motion. This limitation makes the DWI sequence prone to artifacts, especially those related to susceptibility mismatches, which usually arise from the surrounding intestinal gas or metal implants in the pelvis (9,10). These factors result in warping artifacts, geometric distortion, and imaging blurring, which limit the ability to identify muscular invasion and affect the detection of small lesions, thereby reducing diagnostic efficiency (11). Therefore, it is necessary to improve the DWI sequence to optimize the image quality, accurately assess muscular invasion, and choose the best treatment strategy for patients with BC.
Recently, some novel techniques have been applied to DWI. The integrated slice-specific dynamic shimming (iShim) DWI can dynamically optimize the uniform field slice-by-slice in real time so that each layer can reach the optimal field strength during image acquisition. This can reduce magnetic field inhomogeneity and geometric distortion to improve DWI image quality (12-14). This study aimed to qualitatively and quantitatively compare the image quality of DWI with iShim and SS-EPI in diagnosing BC using 3.0 T MRI and investigate the application value of iShim DWI in BC.
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Fujian Provincial Hospital (No. K2020-03-115), and informed consent was obtained from all individual participants.
Consecutive patients with BC who were treated at Fujian Provincial Hospital between November 2019 and April 2021 were collected. The inclusion criteria were as follows: (I) patients who had BC confirmed by postoperative pathology; (II) patients who had not undergone any clinical treatment before the MRI examination; and (III) patients who did not have MRI contraindications and who had available scan sequences, including iShim DWI and SS-EPI DWI. The exclusion criteria were as follows: patients with severe chronic wasting diseases (n=2), severe urinary system complications (n=5), or other reasons (e.g., poor bladder filling, pelvic metal prosthesis, and implant artifacts) leading to either an inability to cooperate for the MRI examination (n=1) or extremely poor images (n=2). A total of 97 patients (86 male; 11 female) with BC were enrolled in the study. The mean age was 64.12±11.97 years (range, 20–88 years).
Equipment and parameters
MRI examinations were performed using a 3.0 T magnetic resonance scanner (MAGNETOM Prisma; Siemens Healthineers, Erlangen, Germany) with an 18-channel phased-array body coil and a 32-channel phased-array spine coil. Patients were scanned in the supine position. The scanning range covered the whole bladder, generally from the anterior superior iliac spine to the pubic symphysis. The scan sequences included conventional axial T1-weighted imaging, multiplanar (axial, coronal, and sagittal) fast spin-echo T2WI, multiplanar iShim DWI, axial SS-EPI DWI, and an axial fat-suppressed 3-dimensional (3D) T1-weighted volumetric interpolated breath-hold examination (T1-VIBE) DCE with multiplanar delayed images. For the multiplanar iShim DWI, only the axial plane was used in this study; the sagittal and coronal planes were used for other studies. The parameters of the iShim DWI were provided by Siemens Healthineers. The parameters of SS-EPI DWI were based on the current clinical protocol for bladder MRI examinations at our institution. The partial parameters were then matched to the iShim DWI by Siemens engineers (Table 1). iShim and SS-EPI DWI shared the same number of slices, slice thickness, and slice gap, corresponding to the T2WI.
Table 1
| Parameters | T2WI | iShim DWI | SS-EPI DWI |
|---|---|---|---|
| Scan plane | Axial, sagittal, and coronal | Axial | Axial |
| Diffusion mode | 3D diagonal | 3-scan trace | |
| Repetition time (ms) | 4280 | 3700 | 7,000 |
| Echo time (ms) | 85 | 48 | 50 |
| Field of view (mm2) | 240×240 | 240×211 | 240×211 |
| Matrix | 320×275 | 100×88 | 100×88 |
| Number of slices | 24 | 24 | 24 |
| Slice thickness (mm) | 3.5 | 3.5 | 3.5 |
| Slice gap (mm) | 0 | 0 | 0 |
| b values (s/mm2) | 50; 600; 1,200 | 50; 600; 1,200 | |
| Averages | 1 | 4; 8; 10 | 2; 3; 4 |
| Bandwidth (Hz/Px) | 200 | 2,442 | 2,442 |
| Parallel imaging | GRAPPA | GRAPPA | GRAPPA |
| Acceleration factor | 2 | 2 | 2 |
| Acquisition time | 1 min 21 s | 1 min 31 s | 3 min 44 s |
T2WI, T2-weighted imaging; DWI, diffusion-weighted imaging; iShim, integrated slice-specific dynamic shimming; SS-EPI, single-shot echo-planar imaging; GRAPPA, generalized autocalibrating partially parallel acquisition.
Patient preparation
Patients were instructed to defecate 6 hours before the MRI examination to reduce intestinal gas interference. After emptying urine 40 min before the examination, each patient was asked to drink approximately 400–800 mL of water to moderately fill their bladder.
Image analysis
All images were transferred to the postprocessing workstation (syngo.via, Siemens Healthineers). The qualitative and quantitative image quality assessment of iShim and SS-EPI DWI in 97 patients with BC was reviewed independently by urological imaging specialists (observers 1–4 with 7–12 years of working experience) who were blinded to the type of DWI and pathological results. One DWI sequence of each patient was randomly selected and assigned to group 1, while another sequence was automatically assigned to group 2.
Observers 1 and 2 were responsible for the qualitative analysis of image quality and tumor muscular invasion. Observers evaluated only 1 group at a time, and the 2 groups were read at an interval of 1 month to reduce mutual interference between assessments.
During the qualitative analysis, observers independently rated the DWI on a 5-point Likert scale of image quality features (10,14-17). These features were anatomical details, distortion, lesion conspicuity, artifacts, and overall image quality. The detailed scoring criteria are shown in Table 2.
Table 2
| Score | Anatomical details | Distortion | Lesion conspicuity | Artifacts | Overall image quality |
|---|---|---|---|---|---|
| 1 | Very poor, unrecognizable bladder contour and edge | Extremely severe | Unrecognizable | Extremely severe | Very poor, unable to diagnose |
| 2 | Poor, blurry bladder contour and edge | Severe | Slight signal difference | Severe | Poor, blurred image |
| 3 | Fair, fairly delineated bladder with a blurry edge | Moderate | Moderate signal difference | Moderate | Fir |
| 4 | Good, good delineated bladder with a sharp edge | Slight | Significant signal difference | Slight | Good, recognizable image |
| 5 | Excellent, smooth, and sharp bladder contour and edge | None | Significant signal difference with a clear lesion edge | None | Excellent, clear image |
DWI, diffusion-weighted imaging.
To assess tumor muscular invasion, observers evaluated muscular invasion based on the vesical imaging-reporting and data system (1–5 points) (2). For each patient, only the lesion with the highest point was considered, and disagreement was resolved through consensus after the 2 groups of assessments. Scores of the vesical imaging-reporting and data system ≥3 points were used as the cutoff score to define muscle-invasive BC (18).
During the quantitative analysis, observers 3 and 4 recorded the number of lesions in each group. They manually tracked the lesions and drew the regions of interest (ROIs) on one DWI with reference to the T2WI and DCE images using the postprocessing workstation. ROIs were copied to the other DWI and their corresponding ADC maps in the same location. For patients with multiple lesions, the largest lesion was selected. All ROIs, indicated by an oval shape on tumors, background tissue, and a random shape on the bladder wall, were placed on the same slice showing the maximum area of the lesion and avoiding the tumor stalk, necrosis, cystic degeneration, and any hemorrhage. The area of the ROI was 8–30 mm2. The SI of BC (SIBC) and the normal bladder wall (SIw), the standard deviation (SD) of the background tissue SI (SDnoise), and the ADC values of BC were recorded. Each index was measured 3 times per observer, and the average was regarded as the final data. The signal-to-noise ratio (SNR) and the contrast-to-noise ratio (CNR) were defined by the following formulas:
SIBC is the SI of BC, SIw is the SI of normal bladder wall away from the tumors on DWI with b =1,200 s/mm2, and SDnoise is the SD of background tissue (pelvic muscle) SI on DWI.
Reference standard
All patients underwent surgery 1 to 6 weeks after the imaging examination. Pathologists recorded the tumor numbers and sizes.
Statistical analysis
Statistical analysis was performed using SPSS 26.0 (IBM Corp, Armonk, NY, USA). Quantitative data with a normal distribution are described as the mean ± SD, and those with a nonnormal distribution are described as the median and interquartile range. Qualitative and quantitative differences in image quality were compared with the Wilcoxon rank sum test and paired-samples t-test, respectively. Inter- and intraobserver consistency was calculated with the Kappa test, and κ ≤0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, and >0.80 indicated slight, fair, moderate, good, and excellent consistency, respectively. The diagnostic performance of tumor muscular invasion on DWI was evaluated using the chi-squared test and the receiver operating characteristic (ROC) curve, which took the histopathological results as the reference standard. A P value of <0.05 was considered statistically significant.
Results
Clinical characteristics
A total of 13 patients underwent a radical cystectomy, and 84 patients underwent a transurethral resection. Pathologists found 224 tumors (58 single and 39 multiple). The maximum tumor diameter of 1 cm was chosen as a cutoff value (2,12): 145 lesions were ≥1 cm with a median of 2.2 cm (1.5–3.4 cm), and 79 lesions were <1 cm with a median of 0.6 cm (0.5–0.7 cm).
The postoperative pathology included 95 cases of urothelial carcinoma and 1 case each of adenocarcinoma and small cell carcinoma. According to pathological results, 30 cases (30.9%) were muscle-invasive BC, and 21 cases (21.7%) were non-muscle-invasive BC. The remaining 46 cases (47.4%) only indicated histological grade and were not included in the statistical category of tumor muscular invasion.
Inter- and intraobserver consistency contrast of image quality ratings
The median scores of anatomical details, distortion, lesion conspicuity, artifacts, and overall image quality of iShim and SS-EPI DWI were consistent between observers 1 and 2. iShim DWI scores were 4, 5, 5, 5, and 5 points, respectively. SS-EPI DWI scores were 4, 4, 5, 4, and 4 points, respectively. The interobserver consistency of image quality ratings was good to excellent on iShim and SS-EPI DWI (κ >0.75; all P<0.001; Table 3). The intraobserver agreement was excellent (κ =0.91 and 0.88 for observers 1 and 2, respectively; both P<0.001).
Table 3
| Category | iShim DWI | SS-EPI DWI | |||
|---|---|---|---|---|---|
| κ | P value | κ | P value | ||
| Anatomic details | 0.84 | <0.001 | 0.80 | <0.001 | |
| Distortion | 0.85 | <0.001 | 0.78 | <0.001 | |
| Lesion conspicuity | 0.79 | <0.001 | 0.80 | <0.001 | |
| Artifacts | 0.76 | <0.001 | 0.80 | <0.001 | |
| Overall image quality | 0.81 | <0.001 | 0.76 | <0.001 | |
DWI, diffusion-weighted imaging; iShim, integrated slice-specific dynamic shimming; SS-EPI, single-shot echo-planar imaging.
Qualitative analysis of image quality
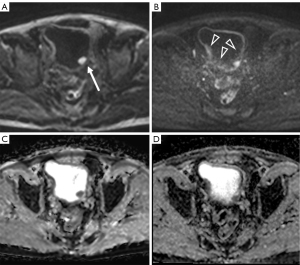
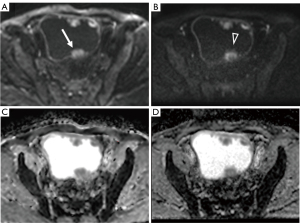
There were no significant differences in anatomic details or lesion conspicuity between iShim and SS-EPI DWI (P>0.05). The scores of iShim DWI in the other 3 aspects and total scores were significantly higher than those of SS-EPI DWI (P<0.001; Table 4; Figures 1,2).
Table 4
| Category | Observer 1 | Observer 2 | |||||
|---|---|---|---|---|---|---|---|
| iShim DWI | SS-EPI DWI | P value | iShim DWI | SS-EPI DWI | P value | ||
| Anatomic details | 4.10±0.57 | 4.04±0.50 | 0.058 | 4.12±0.62 | 4.04±0.52 | 0.059 | |
| Distortion | 4.92±0.28 | 4.10±0.42 | <0.001 | 4.94±0.24 | 4.12±0.44 | <0.001 | |
| Lesion conspicuity | 4.93±0.30 | 4.90±0.39 | 0.37 | 4.95±0.27 | 4.89±0.48 | 0.11 | |
| Artifacts | 4.72±0.45 | 3.75±0.50 | <0.001 | 4.64±0.50 | 3.71±0.48 | <0.001 | |
| Overall image quality | 4.71±0.46 | 3.93±0.30 | <0.001 | 4.67±0.47 | 3.97±0.30 | <0.001 | |
| Total | 23.38±1.26 | 20.72±1.30 | <0.001 | 23.32±1.35 | 20.73±1.36 | <0.001 | |
DWI, diffusion-weighted imaging; iShim, integrated slice-specific dynamic shimming; SS-EPI, single-shot echo-planar imaging.
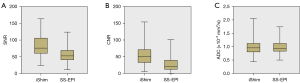
Quantitative analysis of image quality
The SNR and CNR of iShim DWI were higher than those of SS-EPI DWI (P<0.001; Table 5; Figure 3). There was no significant difference between iShim and SS-EPI in ADC values (P>0.05; Figure 4).
Table 5
| Index | iShim DWI | SS-EPI DWI | P value |
|---|---|---|---|
| SNR | 81.10±30.94 | 56.06±21.91 | <0.001 |
| CNR | 54.79±27.34 | 27.23±20.44 | <0.001 |
| ADC value (×10−3 mm2/s) | 0.98±0.25 | 0.98±0.22 | 0.673 |
Data are presented as mean ± standard deviation. DWI, diffusion-weighted imaging; iShim, integrated slice-specific dynamic shimming; SS-EPI, single-shot echo-planar imaging; SNR, signal-to-noise ratio; CNR, contrast-to-noise ratio; ADC, apparent diffusion coefficient.

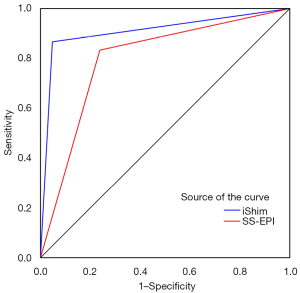
Diagnostic performance of DWI in evaluating tumor muscular invasion
The specificity and accuracy of iShim DWI in diagnosing BC muscular invasion were higher than those of SS-EPI DWI (Table 6). The area under the ROC curve of iShim DWI in diagnosing tumors muscular invasion was significantly higher than that of SS-EPI DWI (P=0.017; Figures 1,5).
Table 6
| Index | iShim DWI | SS-EPI DWI |
|---|---|---|
| Sensitivity | 86.7% (26/30) | 83.3% (25/30) |
| Specificity | 95.2% (20/21) | 76.2% (16/21) |
| Accuracy | 90.2% (46/51) | 80.4% (41/51) |
| AUC (95% CI) | 0.91 (0.80, 0.97) | 0.80 (0.66, 0.90) |
DWI, diffusion-weighted imaging; iShim, integrated slice-specific dynamic shimming; SS-EPI, single-shot echo-planar imaging; AUC, area under the curve; CI, confidence interval.
Detection ability of tumors with different sizes
Based on pathological findings, BCs with a diameter ≥1 cm were visualized on both DWI sequences with a sensitivity of 100% (145/145). Thirty-seven lesions had a diameter of ≤0.5 cm, of which 5 lesions were poorly displayed on SS-EPI DWI and were all missed by 2 observers but were detectable on iShim DWI. The sensitivity of iShim DWI and SS-EPI DWI to detect lesions less than 1 cm in diameter was 100% (79/79) and 93.7% (74/79), respectively.
Discussion
The clinical therapy of BC mainly depends on whether the lesions invade the detrusor muscle. MRI image quality affects the lesion detection rate and the tumor aggressiveness assessment. DWI can reduce overstaging by virtue of its good contrast resolution, which is why DWI shows promising application prospects in BC diagnosis and local staging. Therefore, improved DWI strategies are required to increase the accuracy of preoperative identification between non-muscle-invasive and muscle-invasive BC.
Qualitative and quantitative analysis results indicated that iShim DWI provided better image quality than did SS-EPI DWI. Without affecting the detection rate of BC, iShim DWI could more clearly show whether the detrusor muscle was infiltrated.
SS-EPI DWI was performed using the diffusion mode “3-scan trace”. However, iShim DWI, provided by Siemens, used the diffusion mode “3D diagonal” instead of “3-scan trace”. This scheme switches all 3 gradients simultaneously rather than sequentially with maximum amplitude; hence, it allows a lower echo time than does 3-scan trace and significantly reduces the scan time. Some studies reported that diagonal-DWI (d-DWI) demonstrated equivalent tumor detection, image quality, and ADC values as did the 3-scan trace DWI (t-DWI) with substantially reduced acquisition time (19,20).
This reduction of d-DWI acquisition time can be achieved at a cost of lower SNR compared to t-DWI. Theoretically, to preserve SNR, the averages of d-DWI should be increased by a factor of 3 compared to t-DWI because the loss in SNR has a factor of √3 due to the single diffusion acquisition compared with the sequential acquisition of 3 diffusion directions in t-DWI (20). Although higher averages were set for iShim DWI compared to SS-EPI DWI to compensate for the loss in SNR, Siemens engineers chose a lower number of averages by factors of 2–2.5 to shorten the total scan time. Most patients with BC are middle-aged or older adult patients; therefore, in the case of moderate bladder filling, if the scan time is too long, patients may be unable to hold urine or restrain their body movement, which affects the image quality and is not conducive to lesion display. However, if the bladder is poorly filled, it is also not conducive to visualizing lesions.
Both iShim and SS-EPI DWI used parallel acquisition techniques in our study, which could shorten the echo-train length and reduce the time of phase encoding and acquisition (8,21). It also reduced the acquisition window, which in turn decreased the distortion and susceptibility and magnetic field inhomogeneity-related artifacts (8,9). Minimum repetition time was set for DWI sequences to shorten the scan time. Due to an instrument problem, the item “echo time” was locked in the DWI sequence for any body part (bladder, head, liver, etc.), so it could not be modified manually. When other parameters were set, the echo time was generated automatically, so iShim and SS-EPI DWI had different echo time.
SS-EPI DWI has some limitations, such as strong susceptibility artifacts, geometric distortion, and image blurring, which increase the difficulty of detecting small lesions and sometimes make it impossible to determine whether the tumor edge invades the bladder muscle layer (12). These limitations affect the accurate preoperative staging of BC. Our study found that SS-EPI DWI could detect all lesions with diameters ≥1 cm. However, some lesions less than 1 cm were poorly displayed, which was in accordance with the findings of previous literature (12). In addition, the specificity and accuracy of SS-EPI DWI (76.2% and 80.4%, respectively) in diagnosing tumor muscular invasion were significantly lower than those of iShim DWI (95.2% and 90.2%, respectively).
Moderate bladder filling facilitates good visualization of bladder lesions, which is the key to the success of MRI examinations. However, because the bladder is located in the anterior hypogastrium and close to the anterior abdominal wall, it may be disturbed by respiratory movements, adjacent intestinal peristalsis, and gas. Moreover, bladder peristalsis and urine flow can lead to inhomogeneous magnetic fields, lower image resolution, and severe distortion.
The inhomogeneity of the main magnetic field B0 can be reduced by dynamic frequency adjustment and slice-selective shimming (10). Hence, iShim DWI can achieve optimal field strength in each slice during the image acquisition process and reduce phase loss. In doing so, iShim DWI can reduce local susceptibility artifacts and geometric distortion to ameliorate the problem of image distortion (14,22). In our study, the SNR and CNR of iShim DWI were higher than those of SS-EPI DWI (P<0.001). The increased image resolution facilitated the detection of small lesions (<1 cm). iShim DWI was characterized by good image quality, less geometric distortion, slight artifacts, and great clinical application value in heart, rectum, and whole-body applications (10,13,22). Our study also concluded that iShim DWI could provide better image quality.
Although iShim DWI applied the spectral attenuated inversion recovery technique, it had worse fat suppression performance, especially in subcutaneous tissue. As the suppressed fat signal was constantly superimposed on iShim DWI, the high-channel coil received the signal more readily when the tissue was closer to the coil, whereas more signal was lost in the center. This process resulted in the surrounding high signal and poor background suppression. This was a limitation of iShim DWI. However, insufficient fat suppression did not affect image interpretation or diagnosis.
Great inter and intraobserver consistency of image quality ratings indicated that our study’s scores were highly reliable. The anatomical structure of the bladder contour and lesions could be clearly identified on iShim DWI, with relatively slight image distortion and artifacts. Therefore, the overall image quality was relatively good. ADC values can distinguish benign from malignant tumors, predict tumor grade (23), and assess cancer chemotherapy response. In this study, the ADC values of BC were not significantly different between iShim and SS-EPI DWI (P>0.05), indicating that the iShim DWI technique had no effect on ADC values, which was consistent with the findings of previous studies (15-17). With the increased iShim DWI image resolution, the diagnostic performance of tumor aggressiveness assessment improved. The area under the ROC curve of iShim DWI in distinguishing muscle-invasive and non-muscle-invasive BC was much higher than that of SS-EPI DWI (P=0.017). This finding helped differentiate superficial tumors (pT1) from invasive tumors (≥ pT2). By distinguishing between superficial and invasive tumors, iShim DWI can help in the clinical selection of the appropriate treatment.
In our study, the urine signal was completely suppressed on b =1,200 s/mm2 DWI images, and lesions and edges could be clearly visualized. However, only 2 b values (0 and 1,000 s/mm2) were used by Li et al. (12). Lesions may be masked by insufficient urine suppression on high b value DWI. Therefore, the sensitivity, specificity, and accuracy of iShim DWI in differentiating superficial and invasive tumors were slightly higher in our study (86.7% vs. 84.0%, 95.2% vs. 93.3%, and 90.2% vs. 89.1%, respectively). In addition, the iShim scanning time was significantly shorter in our study (1 min 31 s vs. 4 min 1 s) due to the different parameter settings (e.g., the different diffusion modes, the introduction of parallel acquisition techniques, and a smaller matrix), but did not result in reduced SNR or image quality.
This study had some limitations. First, some iShim and SS-EPI DWI parameters were inconsistent, which might have affected the resulting image quality. However, the parameters were continuously debugged and tried in healthy volunteers and patients with BC by Siemens engineers before the experiment, which enabled us to scan the best images with each technique. We also tried to scan 3 patients with BC with the same parameters (Figure S1, Tables S1,S2). We also found that the image quality of iShim DWI was better than that of SS-EPI DWI. Second, the quantitative image indices were measured manually, and several ROIs were small due to the thin bladder wall and small lesions, which increased the possibility of sampling errors. To compensate, we used multiple measurements and took the average to minimize information bias as much as possible. In order to provide a firmer basis to validate the results of this research, we aim to perform more studies in the future, including a comparative study between iShim and SS-EPI using d-DWI with the same parameters and a comparative study of the differences of iShim using d-DWI and t-DWI in bladder MRI.
Conclusions
Compared with SS-EPI DWI, iShim DWI provided higher image quality. iShim DWI effectively detected BC and better identified muscular invasion, which may be conducive to guiding the clinical selection of appropriate treatment.
Acknowledgments
We greatly appreciate the help all the participants included in the study.
Funding: This work was supported by the Middle-aged Backbone Project Health and Family Planning Commission (No. 2020GGB052) and the Fujian Natural Science Foundation (No. 2021J01359, No. 2022J05211).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-851/coif). Yongbao Wei reports that this work was supported by the Middle-aged Backbone Project Health and Family Planning Commission (No. 2020GGB052) and the Fujian Natural Science Foundation (No. 2021J01359, No. 2022J05211). The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lenis AT, Lec PM, Chamie K, Mshs MD. Bladder Cancer: A Review. JAMA 2020;324:1980-91. [Crossref] [PubMed]
- Panebianco V, Narumi Y, Altun E, Bochner BH, Efstathiou JA, Hafeez S, Huddart R, Kennish S, Lerner S, Montironi R, Muglia VF, Salomon G, Thomas S, Vargas HA, Witjes JA, Takeuchi M, Barentsz J, Catto JWF. Multiparametric Magnetic Resonance Imaging for Bladder Cancer: Development of VI-RADS (Vesical Imaging-Reporting And Data System). Eur Urol 2018;74:294-306. [Crossref] [PubMed]
- Takeuchi M, Sasaki S, Naiki T, Kawai N, Kohri K, Hara M, Shibamoto Y. MR imaging of urinary bladder cancer for T-staging: a review and a pictorial essay of diffusion-weighted imaging. J Magn Reson Imaging 2013;38:1299-309. [Crossref] [PubMed]
- El-Assmy A, Abou-El-Ghar ME, Mosbah A, El-Nahas AR, Refaie HF, Hekal IA, El-Diasty T. Ibrahiem el H. Bladder tumour staging: comparison of diffusion- and T2-weighted MR imaging. Eur Radiol 2009;19:1575-81. [Crossref] [PubMed]
- Huang L, Kong Q, Liu Z, Wang J, Kang Z, Zhu Y. The Diagnostic Value of MR Imaging in Differentiating T Staging of Bladder Cancer: A Meta-Analysis. Radiology 2018;286:502-11. [Crossref] [PubMed]
- Watanabe H, Kanematsu M, Kondo H, Goshima S, Tsuge Y, Onozuka M, Moriyama N. Preoperative T staging of urinary bladder cancer: does diffusion-weighted MRI have supplementary value? AJR Am J Roentgenol 2009;192:1361-6. [Crossref] [PubMed]
- Tekes A, Kamel I, Imam K, Szarf G, Schoenberg M, Nasir K, Thompson R, Bluemke D. Dynamic MRI of bladder cancer: evaluation of staging accuracy. AJR Am J Roentgenol 2005;184:121-7. [Crossref] [PubMed]
- Padhani AR, Liu G, Koh DM, Chenevert TL, Thoeny HC, Takahara T, Dzik-Jurasz A, Ross BD, Van Cauteren M, Collins D, Hammoud DA, Rustin GJ, Taouli B, Choyke PL. Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia 2009;11:102-25. [Crossref] [PubMed]
- van der Pol CB, Chung A, Lim C, Gandhi N, Tu W, McInnes MDF, Schieda N. Update on multiparametric MRI of urinary bladder cancer. J Magn Reson Imaging 2018;48:882-96. [Crossref] [PubMed]
- Qiu J, Liu J, Bi Z, Sun X, Wang X, Zhang J, Liu C, Zhu J, Qin N. Integrated slice-specific dynamic shimming diffusion weighted imaging (DWI) for rectal Cancer detection and characterization. Cancer Imaging 2021;21:32. [Crossref] [PubMed]
- Yeom KW, Holdsworth SJ, Van AT, Iv M, Skare S, Lober RM, Bammer R. Comparison of readout-segmented echo-planar imaging (EPI) and single-shot EPI in clinical application of diffusion-weighted imaging of the pediatric brain. AJR Am J Roentgenol 2013;200:W437-43. [Crossref] [PubMed]
- Li H, Liu L, Shi Q, Stemmer A, Zeng H, Li Y, Zhang M. Bladder cancer: detection and image quality compared among iShim, RESOLVE, and ss-EPI diffusion-weighted MR imaging with high b value at 3.0 T MRI. Medicine (Baltimore) 2017;96:e9292. [Crossref] [PubMed]
- Xiang SF, Zhang XQ, Yang SJ, Gao YY, Gao BL, Shi QL, Li S. Intravoxel Incoherent Motion Magnetic Resonance Imaging with Integrated Slice-specific Shimming for old myocardial infarction: A Pilot Study. Sci Rep 2019;9:19766. [Crossref] [PubMed]
- Stocker D, Manoliu A, Becker AS, Barth BK, Nanz D, Klarhöfer M, Donati OF. Image Quality and Geometric Distortion of Modern Diffusion-Weighted Imaging Sequences in Magnetic Resonance Imaging of the Prostate. Invest Radiol 2018;53:200-6. [Crossref] [PubMed]
- Xie M, Ren Z, Bian D, Li D, Yu L, Zhu F, Huang R, Zhang Z, Suye S, Fu C. High resolution diffusion-weighted imaging with readout segmentation of long variable echo-trains for determining myometrial invasion in endometrial carcinoma. Cancer Imaging 2020;20:66. [Crossref] [PubMed]
- Xia CC, Liu X, Peng WL, Li L, Zhang JG, Meng WJ, Deng XB, Zuo PL, Li ZL. Readout-segmented echo-planar imaging improves the image quality of diffusion-weighted MR imaging in rectal cancer: Comparison with single-shot echo-planar diffusion-weighted sequences. Eur J Radiol 2016;85:1818-23. [Crossref] [PubMed]
- Bogner W, Pinker-Domenig K, Bickel H, Chmelik M, Weber M, Helbich TH, Trattnig S, Gruber S. Readout-segmented echo-planar imaging improves the diagnostic performance of diffusion-weighted MR breast examinations at 3.0 T. Radiology 2012;263:64-76. [Crossref] [PubMed]
- Del Giudice F, Barchetti G, De Berardinis E, Pecoraro M, Salvo V, Simone G, Sciarra A, Leonardo C, Gallucci M, Catalano C, Catto JWF, Panebianco V. Prospective Assessment of Vesical Imaging Reporting and Data System (VI-RADS) and Its Clinical Impact on the Management of High-risk Non-muscle-invasive Bladder Cancer Patients Candidate for Repeated Transurethral Resection. Eur Urol 2020;77:101-9. [Crossref] [PubMed]
- Corcuera-Solano I, Wagner M, Hectors S, Lewis S, Titelbaum N, Stemmer A, Rastinehad A, Tewari A, Taouli B. DWI of the prostate: Comparison of a faster diagonal acquisition to standard three-scan trace acquisition. J Magn Reson Imaging 2017;46:1767-75. [Crossref] [PubMed]
- Hectors SJ, Wagner M, Corcuera-Solano I, Kang M, Stemmer A, Boss MA, Taouli B. Comparison Between 3-Scan Trace and Diagonal Body Diffusion-Weighted Imaging Acquisitions: A Phantom and Volunteer Study. Tomography 2016;2:411-20. [Crossref] [PubMed]
- Xu L, Xu J, Zheng Q, Yuan J, Liu J. A miniature U-net for k-space-based parallel magnetic resonance imaging reconstruction with a mixed loss function. Quant Imaging Med Surg 2022;12:4390-401. [Crossref] [PubMed]
- Zhang H, Xue H, Alto S, Hui L, Kannengiesser S, Berthold K, Jin Z. Integrated Shimming Improves Lesion Detection in Whole-Body Diffusion-Weighted Examinations of Patients With Plasma Disorder at 3 T. Invest Radiol 2016;51:297-305. [Crossref] [PubMed]
- Fujima N, Shimizu Y, Yoneyama M, Nakagawa J, Kameda H, Harada T, Hamada S, Suzuki T, Tsushima N, Kano S, Homma A, Kudo K. The utility of diffusion-weighted T2 mapping for the prediction of histological tumor grade in patients with head and neck squamous cell carcinoma. Quant Imaging Med Surg 2022;12:4024-32. [Crossref] [PubMed]


