
Around the time of a hip fracture, older East Asian female patients tend to measure lower densitometric femoral neck and total hip T-scores than older Caucasian female patients: a literature analysis
The clinical significance of osteoporosis lies in the fractures that occur, and the most important fracture is hip fracture. According to the 1994 World Health Organization (WHO) criteria, the T-score is defined as: (BMDpatient–BMDyoung normal mean)/SDyoung normal population, where BMD is bone mineral density and SD is the standard deviation. When the femoral neck is measured in adult women, a cutpoint value of patient BMD of 2.5 SD below the BMDyoung normal mean satisfies that the prevalence of osteoporosis for those aged ≥50 years is about 16.2%, the same as the lifetime risk of hip fragility fracture (FF) (1,2). If other sites are also considered, this cutpoint value identifies approximately 30% of postmenopausal women as having osteoporosis, which is approximately equivalent to the lifetime risk of FF at the spine, hip, or forearm. The FF prevalence of older Chinese women is slightly less than half that of Caucasians (3,4). This is the case for hip FF (5-7), radiographic vertebral FF (8), clinical vertebral FF (9-11), and many other FF sites (3,4,12,13). As compared with Caucasians, Chinese demonstrate an overall stronger skeleton property (14). For example, Walker et al. (15) reported that postmenopausal Chinese women have a higher trabecular plate-to-rod ratio and greater whole bone stiffness, translating into a greater trabecular mechanical competence.
Following the 1994 WHO definition, densitometric osteoporosis prevalence among a non-Caucasian population should be in proportion to its relative osteoporotic fracture risk with Caucasian data as reference (16). To achieve this goal, various region/ethnic-specific reference BMD databases have been published (3). Furthermore, the cutpoint T-score for defining densitometric osteoporosis should be adjusted according to the osteoporotic fracture risk profile. Based on statistical modeling (3), we proposed that the femoral neck cutpoint T-score is revised from ≤−2.5 to ≤−2.75 for Hong Kong older women when a local BMD reference published by Lynn et al. (17) is applied. The same principle can also be applied to Japanese older women if a local BMD reference published by Iki et al. is used (3,18). In an empirical study on women with radiographic vertebral FF as a surrogate clinical endpoint, we recently demonstrated that, at the mean age of around 74, a femoral neck T-score of −2.60 for Italian Caucasians is equivalent to −2.77 for Hong Kong Chinese, while a lumbar spine T-score of −2.44 for Italian Caucasians is equivalent to −3.75 for Hong Kong Chinese (19). Moreover, our literature analysis suggested that, while a cutpoint T-score ≤−2.5 for defining spine densitometric osteoporosis is justified for Caucasian women, for East Asian women the same cutpoint T-score much inflates the estimated prevalence of spine densitometric osteoporosis (11).
To further support our argument that the cutpoint T-score for defining femoral neck densitometric osteoporosis among East Asian populations should be lower than the conventional value of ≤−2.5, we conducted an additional literature analysis. The hypothesis is that, around the time when a proximal femur FF occurs (which is a clinical endpoint for osteoporosis), East Asians measure a lower T-score than that of Caucasians. We grouped together Chinese, Korean, and Japanese as East Asians. It has been suggested that Korean and Japanese older women have similar FF risk profiles similar to those of older Chinese women (5,13,20-23). On Dec 13th 2022, two structured literature searches on https://pubmed.ncbi.nlm.nih.gov/ were conducted using the keywords combination of ‘((hip OR femur OR femoral) AND fracture) AND T-score’, and ‘(BMD OR T-score) AND hip fracture AND (Chinese OR Korean OR Japanese)’. These searches generated 1,558 results and 492 results respectively. The results were initially screened by their titles, and then by their abstracts (when available). For potentially relevant items, the full articles were retrieved for analysis. Though Singapore is a Southeast Asia nation, data from Singapore were included as 75% of Singaporean populations are ethnically Chinese.
We only included studies on proximal femoral fractures among older subjects while excluded the studies included a significant portion of high energy trauma cases, thus included cases are assumed to be mostly FF. Efforts were made that the reported cases were only counted once in this analysis (note some authors might have used the same case materials for different types of analysis and published more than one article). We aimed to include studies concerning dual-energy X-ray absorptiometry areal BMD measured around the time of fracture, and usually the fracture was shortly followed by surgical intervention. Other excluding criteria were: (I) articles concerned with patients group-wise systematically under a specific anti-osteoporotic treatment regime, however, it was allowed when a portion of cases was under an anti-osteoporosis medication as an usual care (as would be expected in a real-world clinic); (II) articles concerned with specific types of patients such as those with diabetes mellitus type 2, however, it was allowed for studies with a portion of their patients had a disease such as diabetes mellitus type 2 (as would be expected among general community older subjects); (III) articles only concerned with hip re-fracture patients; (IV) articles concerned with atypical femur fracture; (V) articles concerned with femoral head subchondral insufficiency fracture; (VI) articles concerned with ex vivo study; (VII) study cohorts with fewer than 10 cases. For articles from East Asia, we only included studies which used a local or an East Asian BMD reference. If this aspect was not specified in the published article, the authors were contacted to validate this information, and articles were excluded if this could not be validated (only one article was excluded due to this reason). Finally, we included 12 articles (n=5 for East Asians and n=7 for Caucasians) that reported women’s and men’s data separately, and 12 articles (n=7 for East Asians and n=5 for Caucasians) that reported women’s and men’s data together. The articles available for analysis were much fewer than initially anticipated. Many studies concerned with proximal femur FF only reported BMD values instead of T-score values. Some studies reported T-score classifications (such as 28% of the hip fracture patients had femoral neck T-score of ≤−2.5) instead of the actual T-score values.
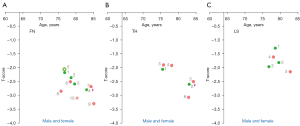
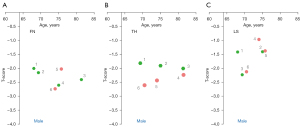
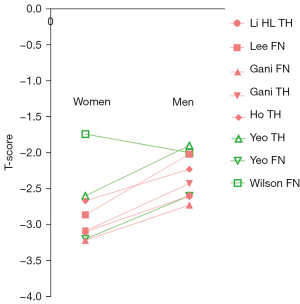
For the data in the articles included for analysis, the results are shown in Figure 1 for female patients (24-33), Figure 2 for male and female patients mixed (34-45), and Figure 3 for male patients (24,28-30,32,33,46,47). For the data in Figure 2, females commonly constituted 2/3 of the cases, reflecting that hip fracture prevalence among older women is about double of that among older men. A trend can be seen that East Asian female patients measure a lower femoral neck and a lower total hip T-score than those of Caucasians. The same trend is also tentatively noted for female patients’ lumbar spine T-score. For the data of male and female patients mixed, a trend is only noted that East Asian patients measure lower femoral neck T-score. For male patients, only a ‘possible’ trend is noted that East Asian patients measure lower total hip T-scores. Another point noted is that, around the timepoint of a hip fracture, at least for East Asians included in this study, male patients tend to measure higher femoral neck and total hip T-scores than those of female patients (Figure 4) (24,28-30,32,33). Based on Figure 4, it appears that, a femoral neck T-score of −3.3 in East Asian women will be approximately equivalent to a femoral neck T-score of −2.4 in East Asian men (a hip T-score of −3.0 in East Asian women will be approximately equivalent to a hip T-score of −2.4 in East Asian men, note that femoral neck T-score and hip T-score are usually highly correlated). This may suggest that different T-score cutpoints for classifying densitometric osteoporosis should be applied for Asian men and women, on the other hand, this observation may also be coincidental. Note, the 1994 WHO Study Group did not establish any guidelines for the diagnosis of osteoporosis in men (1).

There are many limitations to the current analysis. The patient populations included in the current analysis were highly heterogeneous, while the number of studies available for analysis is small. In theory, for the studies which reported the BMD values and the specific type of bone densitometer used, we could use a suitable ethnic specific BMD reference database and perform an adjustment to count for the bone densitometers employed to derive T-scores. However, we did not choose to do this as we consider our analysis as a ‘test-of-the-concept’ study. Since the expected trend was already shown, we did not want to further complicate our analysis, thus we chose only to use the T-score results as they were reported by the authors. The trend that older East Asian patients tend to measure lower femoral neck and total hip T-scores than older Caucasians as shown in the current analysis was not strong nor a ‘clear-cut’. This is probably not surprising. Our proposed cutpoint T-score for female femoral neck only differs by −0.2 to −0.25 from the conventional value of −2.5 (3). However, its impact on epidemiological studies will not be trivial. As an example, using the Japanese data of Iki et al., an adjustment of femoral neck T-score from ≤−2.5 to ≤−2.75 can lower osteoporosis prevalence for older Japanese women aged 50–79 years from 12% to 7.5% (3). Another point is that the precision of BMD measures is affected by many factors. Many reports specified that femoral neck and total hip BMD were measured using the contra-lateral non-fractured hip, while a few articles did not report such details. We can only assume the necessary steps to ensure a satisfactory level of measurement precision were taken by the authors. Note the right and left hips commonly have very similar BMD values. For the current analysis, we initially anticipated a bigger difference for lumbar spine T-score between East Asians and Caucasians. The data in Figures 1-3 for lumbar spine T-score may reflect that lumbar spine T-score is not as predictive for hip fracture risk as femoral neck or total hip T-scores. The measurement of lumbar spine BMD is complicated by spine degeneration which can lead to artificially higher BMD measures, thus only a lower lumbar spine T-score is relevant rather than the mean lumbar spine T-score. In this study, except for the data of Carlson et al. (41), all other Caucasian data are from Europe and Near East. The ethnicities of the patients in their studies were mostly not specified, we take it that it is a reasonable assumption that most of their older patients were Caucasians.
In conclusion, our literature analysis suggests that, around the time of a hip fracture, older East Asian female patients tend to measure lower femoral neck and total hip T-scores than older Caucasian female patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-65/coif). YXJW serves as the Editor-in-Chief of Quantitative Imaging in Medicine and Surgery. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Assessment of fracture risk and its application to screen-ing for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992]. 1994. Available online: https://apps.who.int/iris/handle/10665/39142
- Jain RK, Vokes T. Dual-energy X-ray Absorptiometry. J Clin Densitom 2017;20:291-303. [Crossref] [PubMed]
- Wáng YXJ, Xiao BH. Estimations of bone mineral density defined osteoporosis prevalence and cutpoint T-score for defining osteoporosis among older Chinese population: a framework based on relative fragility fracture risks. Quant Imaging Med Surg 2022;12:4346-60. [Crossref] [PubMed]
- Wáng YXJ. Fragility fracture prevalence among elderly Chinese is no more than half of that of elderly Caucasians. Quant Imaging Med Surg 2022;12:874-81. [Crossref] [PubMed]
- Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, Tan KC, Luckey MM, Cauley JA, Fujiwara S, Kung AW. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int 2012;23:879-85. [Crossref] [PubMed]
- Xu L, Lu A, Zhao X, Chen X, Cummings SR. Very low rates of hip fracture in Beijing, People's Republic of China the Beijing Osteoporosis Project. Am J Epidemiol 1996;144:901-7. [Crossref] [PubMed]
- Ho SC, Bacon WE, Harris T, Looker A, Maggi S. Hip fracture rates in Hong Kong and the United States, 1988 through 1989. Am J Public Health 1993;83:694-7. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Leung JCS, Iannacone A, Kripa E, Kwok TCY, Diacinti D. Much lower prevalence and severity of radiographic osteoporotic vertebral fracture in elderly Hong Kong Chinese women than in age-matched Rome Caucasian women: a cross-sectional study. Arch Osteoporos 2021;16:174. [Crossref] [PubMed]
- Hayhoe RPG, Chan R, Skinner J, Leung J, Jennings A, Khaw KT, Woo J, Welch AA. Fracture Incidence and the Relevance of Dietary and Lifestyle Factors Differ in the United Kingdom and Hong Kong: An International Comparison of Longitudinal Cohort Study Data. Calcif Tissue Int 2021;109:563-76. [Crossref] [PubMed]
- Wáng YXJ, Deng M, Griffith JF, Kwok AWL, Leung JCS, Lam PMS, Yu BWM, Leung PC, Kwok TCY. 'Healthier Chinese spine': an update of osteoporotic fractures in men (MrOS) and in women (MsOS) Hong Kong spine radiograph studies. Quant Imaging Med Surg 2022;12:2090-105. [Crossref] [PubMed]
- Wáng YXJ. The definition of spine bone mineral density (BMD)-classified osteoporosis and the much inflated prevalence of spine osteoporosis in older Chinese women when using the conventional cutpoint T-score of -2.5. Ann Transl Med 2022;10:1421. [Crossref] [PubMed]
- Morin SN, Berger C, Liu W, Prior JC, Cheung AM, Hanley DA, Boyd SK, Wong AKO, Papaioannou A, Rahme E, Goltzman D. Differences in fracture prevalence and in bone mineral density between Chinese and White Canadians: the Canadian Multicentre Osteoporosis Study (CaMos). Arch Osteoporos 2020;15:147. [Crossref] [PubMed]
- Shin MH, Zmuda JM, Barrett-Connor E, Sheu Y, Patrick AL, Leung PC, Kwok A, Kweon SS, Nam HS, Cauley JA. Race/ethnic differences in associations between bone mineral density and fracture history in older men. Osteoporos Int 2014;25:837-45. [Crossref] [PubMed]
- Cong E, Walker MD. The Chinese skeleton: insights into microstructure that help to explain the epidemiology of fracture. Bone Res 2014;2:14009. [Crossref] [PubMed]
- Walker MD, Liu XS, Zhou B, Agarwal S, Liu G, McMahon DJ, Bilezikian JP, Guo XE. Premenopausal and postmenopausal differences in bone microstructure and mechanical competence in Chinese-American and white women. J Bone Miner Res 2013;28:1308-18. [Crossref] [PubMed]
- Wáng YXJ. Estimation of osteoporosis prevalence among a population is reasonable only after the concerned reference bone mineral density database and cutpoint T-score have been validated. Osteoporos Int 2023;34:417-8. [Crossref] [PubMed]
- Lynn HS, Lau EM, Au B, Leung PC. Bone mineral density reference norms for Hong Kong Chinese. Osteoporos Int 2005;16:1663-8. [Crossref] [PubMed]
- Iki M, Kagamimori S, Kagawa Y, Matsuzaki T, Yoneshima H, Marumo F. Bone mineral density of the spine, hip and distal forearm in representative samples of the Japanese female population: Japanese Population-Based Osteoporosis (JPOS) Study. Osteoporos Int 2001;12:529-37. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Leung JCS, Iannacone A, Kripa E, Kwok TCY, Diacinti D. Conversion of osteoporotic vertebral fracture severity score to osteoporosis T-score equivalent status: a framework and a comparative study of Hong Kong Chinese and Rome Caucasian older women. Arch Osteoporos 2022;18:1. [Crossref] [PubMed]
- Cheung CL, Ang SB, Chadha M, Chow ES, Chung YS, Hew FL, Jaisamrarn U, Ng H, Takeuchi Y, Wu CH, Xia W, Yu J, Fujiwara S. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia 2018;4:16-21. [Crossref] [PubMed]
- Kwok AW, Gong JS, Wang YX, Leung JC, Kwok T, Griffith JF, Leung PC. Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int 2013;24:877-85. [Crossref] [PubMed]
- Patel MC, Chandra M, Lo JC. Mortality following hip fracture in Chinese, Japanese, and Filipina women. Am J Manag Care 2016;22:e358-9. [PubMed]
- Lo JC, Chandra M, Lee C, Darbinian JA, Ramaswamy M, Ettinger B. Bone Mineral Density in Older U.S. Filipino, Chinese, Japanese, and White Women. J Am Geriatr Soc 2020;68:2656-61. [Crossref] [PubMed]
- Wilson J, Bonner TJ, Head M, Fordham J, Brealey S, Rangan A. Variation in bone mineral density by anatomical site in patients with proximal humeral fractures. J Bone Joint Surg Br 2009;91:772-5. [Crossref] [PubMed]
- Olszewski K, Olszewska-Słonina D, Matewski D, Kruczyński J. Bone mineral density in patients with femoral neck fractures. Ortop Traumatol Rehabil 2006;8:395-401. [PubMed]
- Schnabel M, Eser G, Ziller V, Mann D, Mann E, Hadji P. Bone mineral density in postmenopausal women with proximal femoral fractures--comparative study between quantitative ultrasonometry and gold standard DXA. Zentralbl Chir 2005;130:469-75. [Crossref] [PubMed]
- Di Monaco M, Castiglioni C, Bardesono F, Milano E, Massazza G. Sarcopenia, osteoporosis and the burden of prevalent vertebral fractures: a cross-sectional study of 350 women with hip fracture. Eur J Phys Rehabil Med 2020;56:184-90. [Crossref] [PubMed]
- Yeo AK, Ahrberg AB, Theopold JD, Ewens S, Borte G, Josten C, Fakler JK. Are radiographic indices reliable indicators for quantitative bone mineral density and vitamin D status after femoral neck fractures? A retrospective study in 112 elderly patients. Patient Saf Surg 2015;9:39. [Crossref] [PubMed]
- Lee KH, Park JW, Kim S, Lee GY, Park SB, Yang DB, Ha YC. Prevalence, Clinical Implication, and Cause of Spine Hip Discordance in Elderly Patients with Fragility Hip Fracture. J Bone Metab 2022;29:51-7. [Crossref] [PubMed]
- Gani LU, Saripalli KR, Fernandes K, Leong SF, Tsai KT, Tan PT, Chong LR, King TFJ. Bone mineral density and trabecular bone score in elderly type 2 diabetes Southeast Asian patients with severe osteoporotic hip fractures. PLoS One 2020;15:e0241616. [Crossref] [PubMed]
- Zhu TY, Hung VW, Cheung WH, Cheng JC, Qin L, Leung KS. Value of Measuring Bone Microarchitecture in Fracture Discrimination in Older Women with Recent Hip Fracture: A Case-control Study with HR-pQCT. Sci Rep 2016;6:34185. [Crossref] [PubMed]
- Ho AW, Lee MM, Chan EW, Ng HM, Lee CW, Ng WS, Wong SH. Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric patients with hip fracture and its correlation with different factors. Hong Kong Med J 2016;22:23-9. [PubMed]
- Li HL, Shen Y, Tan LH, Fu SB, Dai RC, Yuan LQ, Sheng ZF, Xie ZJ, Wu XP, Liao EY, Tang XL, Wu XY. Relationship between bone mineral density and fragility fracture risk: a case-control study in Changsha, China. BMC Musculoskelet Disord 2021;22:728. [Crossref] [PubMed]
- Xu Z, Tian G, Liu C, Xie Y, Zhang R. The predictive value of the Singh index for the risk of InterTAN intramedullary fixation failure in elderly patients with intertrochanteric fractures. BMC Musculoskelet Disord 2022;23:769. [Crossref] [PubMed]
- Lo JC, Kim S, Chandra M, Ettinger B. Applying ethnic-specific bone mineral density T-scores to Chinese women in the USA. Osteoporos Int 2016;27:3477-84. [Crossref] [PubMed]
- Kang JS, Kwon YT, Suh YJ, Lee TJ, Ryu DJ. Outcomes of U-Blade Lag Screw for Cephalomedullary Fixation of Unstable Trochanteric Femur Fractures: A Case Control Study. Geriatr Orthop Surg Rehabil 2020;11:2151459320979975. [Crossref] [PubMed]
- Heetveld MJ, Raaymakers EL, van Eck-Smit BL, van Walsum AD, Luitse JS. Internal fixation for displaced fractures of the femoral neck. Does bone density affect clinical outcome? J Bone Joint Surg Br 2005;87:367-73. [Crossref] [PubMed]
- Amar AOS, Hyldstrup L, Nielsen J, Palm H, Jensen JB. Intensive screening for osteoporosis in patients with hip fracture. Arch Osteoporos 2019;14:63. [Crossref] [PubMed]
- Valentini A, Cianfarani MA, Federici M, Tarantino U, Bertoli A. Osteoprotegerin in diabetic osteopathy. Nutr Metab Cardiovasc Dis 2020;30:49-55. [Crossref] [PubMed]
- Ganhão S, Guerra MG, Lucas R, Terroso G, Aguiar F, Costa L, Vaz C. Predictors of Mortality and Refracture in Patients Older Than 65 Years With a Proximal Femur Fracture. J Clin Rheumatol 2022;28:e49-55. [Crossref] [PubMed]
- Carlson BC, Robinson WA, Wanderman NR, Nassr AN, Huddleston PM 3rd, Yaszemski MJ, Currier BL, Jeray KJ, Kirk KL, Bunta AD, Murphy S, Patel B, Watkins CM, Sietsema DL, Edwards BJ, Tosi LL, Anderson PA, Freedman BA. The American Orthopaedic Association's Own the Bone® database: a national quality improvement project for the treatment of bone health in fragility fracture patients. Osteoporos Int 2018;29:2101-9. [Crossref] [PubMed]
- Li XP, Zhang P, Zhu SW, Yang MH, Wu XB, Jiang XY. All-cause mortality risk in older patients with femoral neck fracture. BMC Musculoskelet Disord 2022;23:941. [Crossref] [PubMed]
- Hey HW, Sng WJ, Lim JL, Tan CS, Gan AT, Ng JH, Kagda FH. Interpretation of hip fracture patterns using areal bone mineral density in the proximal femur. Arch Orthop Trauma Surg 2015;135:1647-53. [Crossref] [PubMed]
- Kanno A, Aizawa T, Mori Y, Aizawa T. Different types of hip fragility fractures have different values of 25-hydroxyvitamin D and parathyroid hormone. J Orthop Sci 2022;S0949-2658(22)00315-3. Epub ahead of print. [Crossref] [PubMed]
- Yamamoto N, Tomita Y, Noda T, Inoue T, Mochizuki Y, Ozaki T. Reduction quality and nail fixation ratio as bone-implant stability factors associated with reoperation for trochanteric fractures. Injury 2021;52:1813-8. [Crossref] [PubMed]
- Cesme F, Esmaeilzadeh S, Oral A. Discriminative ability of calcaneal quantitative ultrasound compared with dual-energy X-ray absorptiometry in men with hip or distal forearm fractures. Acta Orthop Traumatol Turc 2016;50:548-53. [Crossref] [PubMed]
- Di Monaco M, Castiglioni C, Milano E, Massazza G. Is there a definition of low lean mass that captures the associated low bone mineral density? A cross-sectional study of 80 men with hip fracture. Aging Clin Exp Res 2018;30:1429-35. [Crossref] [PubMed]


