
A large leiomyoma of the round ligament: a case description and literature analysis
Background
Leiomyoma of the round ligament is part of a family of fibroids and is composed of smooth muscle, fibrous tissue, and fat (1). Leiomyoma of the round ligament is rare. The majority of cases are commonly located in the extraperitoneal region of the round ligament. Patients presenting with round ligament leiomyosarcoma sometimes experience abdominal pain, but many patients are asymptomatic (2). Most round ligament leiomyomas are diagnosed incidentally during physical health examinations or the imaging of other diseases of the abdomen. Our knowledge of this disease is limited due to the paucity of research and literature reports. In this paper, we present an unusual case of a patient with an intra-abdominal left leiomyoma of the round ligament and provide a review of the related literature. We also discuss imaging, which is essential for early diagnosis.
Case presentation
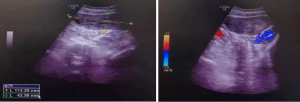
A 45-year-old woman consulted the Department of Obstetrics and Gynecology of Gansu Provincial Hospital. She reported that she had a history of abdominal distention for 2 months. The patient’s menarche was at age 12 years, she was gravida 2, she had no history of oral contraceptive use, and menopause had not occurred. When the patient’s systems were rechecked, there was no weight loss, night sweats, nausea, chills, vomiting, or bladder symptoms, and her previous medical and operational history was also uncharacteristic. A follow-up Doppler ultrasound showed an 11.2 cm × 9.5 cm × 4.3 cm mass, which was oval with a clear boundary and attached to the uterus (Figure 1).
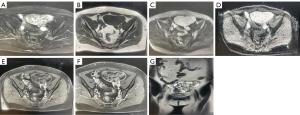
The results of a staging chest computed tomography (CT) scan were unremarkable. A magnetic resonance imaging (MRI) scan showed a large mass in the left pelvic cavity with slight enhancement (Figure 2). There was an absence of clear evidence of local infiltration or lymphadenopathy; therefore, it was highly doubtful that the mass was a benign pelvic tumor. The patient was treated with laparoscopic exploration.
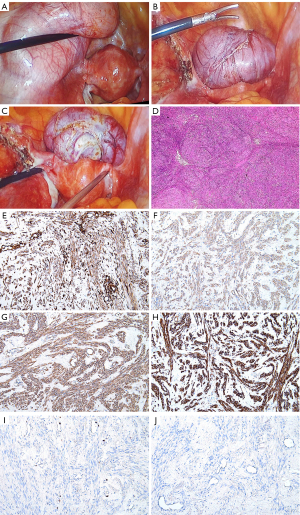
Laparoscopic surgery revealed a normal uterus with normal bilateral adnexa. A well-defined solid mass about 12 cm × 10 cm in size originated from the left round ligament of the uterus (Figure 3A,3B). No macrological irregularities were detected on the surface of the peritoneum. Subsequently, the left round ligament mass of the uterus was removed. Figure 3C shows a section of the mass. The tissue near the capsule was gray, solid, and tough, and the central tissue was yellow, solid, and soft. The specimen was examined by histopathology, which showed a staggered fascicle of smooth muscle cells (Figure 3D). Staining by immunohistochemistry (IHC) indicated that the cells were positive for vimentin (Figure 3E), H-caldesmon (Figure 3F), smooth muscle actin (SMA; Figure 3G), and desmin (Figure 3H). The Ki-67 index was less than 10%, and CKP was negative (Figure 3I,3J). The diagnosis was leiomyoma of the round ligament.
The patient was discharged from the hospital on postoperative day 4. A well-healed scar was visible after the surgery, with no overlying skin changes. No evidence of disease recurrence was discovered at the 6-month follow-up.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Literature review
Primary large leiomyoma of the round ligament is very rare. We searched the PubMed, Medline, Web of Science, and Ovid databases for English language case reports and cases of round ligament leiomyoma. We selected the literature published in the period from January 1, 2000, to March 1, 2022. After careful filtration of duplicates and unrelated results, data from 19 patients in 19 reports were collected and analyzed (Table 1).
Table 1
| Author [year] | Age (years) | Size (cm) | Side | Presentation | Imaging | Surgery |
|---|---|---|---|---|---|---|
| Vignali M, [2006] (3) | 40 | 10×12×9 | R | Acute pain in the right iliac fossa | US | Laparoscopy |
| Grossman SL, [2007] (4) | 49 | 3.9 (diameter) | R | Right adnexal mass | US | Laparoscopy |
| Kirkham JC, [2008] (5) | 43 | 9.0 | R | An asymptomatic, enlarging right groin mass | MRI | N/A |
| Ali SM, [2012] (6) | 38 | 5.0×5.0 | R | Painless swelling | N/A | Laparotomy |
| Colak E, [2013] (7) | 40 | 6.0×6.0 | R | Painless groin mass | US | Laparotomy |
| Chang TM, [2013] (8) | 52 | 4.0×3.5×5.0 | L | Chronic pelvic pain | US | Laparoscopy |
| E H, [2014] (9) | 40 | 3.0×4.0 (CT) | L | Painful abdomen and left inguinal swelling | CT | Laparotomy |
| Canto MJ, [2015] (10) | 63 | 5.0×5.0×5.0 | R | Asymptomatic | CT | Laparoscopic |
| Birge O, [2015] (11) | 28 | 3.0×2.0 (US) | L | Dyspareunia | US | Laparotomy |
| Bedir R, [2016] (12) | 32 | 4.8×3.5×3.0 (US) | R | Painful swelling | US | Laparotomy |
| Najjar M, [2016] (13) | 47 | 4.0×3.0×2.0 | R | Intermittently painful | N/A | Laparotomy |
| Efthimiadis C, [2017] (14) | 34 | 6.0×6.0 | R | Swelling in the right inguinal region | N/A | Laparotomy |
| Deol M, [2017] (15) | 68 | 2.1×1.7×2.0 (US) | L | Intermittent pelvic pain | US, MRI | N/A |
| Kan Ö, [2017] (16) | 39 | 8×7 | L | Swelling | US | Laparotomy |
| Klingbeil KD, [2017] (2) | 68 | 25.0×9.0×8.5 | L | Inguinal mass | CT | Laparotomy |
| Kaya C, [2018] (17) | 28 | 4.5×4 (US) | R | Pelvic pain | US, MRI | Laparoscopy |
| Christodoulou IM, [2018] (18) | 47 | 19×6×2.5 (MRI) | R | Painless mass in the left inguinal region | MRI | Laparotomy |
| Kypriotis K, [2021] (19) | 26 | 7.5×6.6×5.9 | L | Left-sided discomfort | US | Laparoscopy |
| Tympa A, [2021] (20) | 51 | 9.0 | R | Asymptomatic | US, MRI | Laparotomy |
| Bhatti D, [2022] (1) | 45 | 16.4×15.0 (US) | R | Asymptomatic | US, MRI | Laparotomy |
L, left; R, right; US, ultrasound; CT, computed tomography; MRI, magnetic resonance imaging; N/A, not available or not applicable.
Of all patients included in the 19 analyzed reports, only 6 had masses on their left side, and most masses were on the right side. The age range of the patients spanned from 28 to 68 years old, and their clinical manifestations were diverse. The size of the tumors in all cases of round ligament leiomyoma ranged from 2 to 19 cm; 79% of the masses exceeded 4.0 cm. With regard to preoperative diagnostic evaluation for leiomyomas, ultrasound (n=12) was used most often. Four cases were evaluated using ultrasound combined with MRI. In all patients, surgical management was the primary treatment option. Laparoscopy was most commonly used for intra-abdominal leiomyomas, whereas laparotomy was used for extra-abdominal leiomyomas.
Discussion
Large leiomyoma of the round ligament is very rare. Only 21 documented cases of round ligament leiomyomas were reported between January 1, 2000, and March 1, 2022. Most leiomyomas are in the extraperitoneal region of the round ligament (21). The reason for the predominance of this location is unknown.
Although somatic mutations of normal smooth muscle, sex steroids, and local growth factors have been hypothesized, the mechanism of primary round ligament leiomyoma development remains unclear. Lösch et al. (22) reported a postmenopausal patient with a history of using estrogen and suggested that the estrogen might have promoted leiomyoma . In contrast, our patient never received hormonal treatment.
There are no specific symptoms of round ligament leiomyoma. A small percentage of patients have abdominal pain; however, most patients are not symptomatic. Round ligament leiomyoma is usually found during a medical examination, ultrasound, or MRI. The symptoms are determined by the size, location, and growth rate of the tumor. Two-thirds of leiomyomas occur in the extraperitoneal portion, which includes the vulva and inguinal area, and are commonly noted as labial or inguinal masses (10). Those that are intra-abdominal, as in our patient, are less commonly reported.
The clinical manifestation is a solid adnexal mass. Therefore, differential diagnosis between ovarian tumors and benign uterine fibroids is challenging. Traditional detection modalities for round ligament leiomyoma include ultrasound, CT, and MRI. The same methods of detection applied to round ligament leiomyoma are used for other types of leiomyoma. The key to the diagnosis of leiomyoma is Doppler ultrasound, which shows the vascular connections of the leiomyoma with the uterus. In our case, an MRI scan showed an oval with a clear boundary without any pathological lymph nodes, which suggested a benign mass. MRI is necessary to diagnose cases and distinguish between malignant and benign pelvic masses.
Currently, the most common way to manage round ligament leiomyoma is open surgical excision or laparoscopy. Furthermore, robot-assisted laparoscopic myomectomy is suitable for patients with round ligament leiomyoma. With regard to their size and location, open surgical excision, laparoscopy, or robot-assisted laparoscopic myomectomy can lead to a satisfactory result with hardly any recurrence. In our case, the round ligament leiomyoma was in the intra-abdominal area. Therefore, laparoscopy was suitable and achieved a great outcome.
The continued advancement of diagnostic skills should lead to more approaches to identifying round ligament leiomyoma and more sophisticated options for treating round ligament leiomyoma. These advancements will gradually achieve a safe, feasible diagnosis with an excellent prognosis in round ligament leiomyoma treatment.
Conclusions
The incidence of large leiomyoma is common, and the majority occur in the uterine body. However, the 45-year-old woman in our case report demonstrated a very rare presentation—a large leiomyoma situated in the round ligament. Usually, Doppler ultrasound and MRI can be used as tools for diagnosis before the patient undergoes an operation. Therefore, round ligament leiomyoma is typically diagnosed with Doppler ultrasound and MRI assessment. If the mass can be successfully resected, the outcome for the patient is favorable.
Acknowledgments
Funding: This work was supported by the Youth Science Foundation of Gansu Province (Grant No. 21JR1RA006), the Natural Science Foundation of Gansu Province of China (Grant No. 21JR1RA012), and the Innovation and Entrepreneurship Talent Project of Lanzhou (2020-RC-52).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-311/coif). All authors reported that this work was supported by the Youth Science Foundation of Gansu Province (21JR1RA006), the Natural Science Foundation of Gansu Province of China (21JR1RA012), the Internal Hospital Scientific Research Project of Gansu Province (21GSSYC-10), and the Innovation and Entrepreneurship Talent Project of Lanzhou (2020-RC-52). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient and her husband for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bhatti D, Mandrelle K, Chander A. Leiomyoma of the round ligament in a postmenopausal woman: A rare case report. Int J Gynaecol Obstet 2022;156:585-6. [Crossref] [PubMed]
- Klingbeil KD, Polcari AM, Azab B, Franceschi D. Large, extra-abdominal leiomyoma of the round ligament with carneous degeneration. BMJ Case Rep 2017;2017:bcr-2017-222454. [Crossref] [PubMed]
- Vignali M, Bertulessi C, Spreafico C, Busacca M. A large symptomatic leiomyoma of the round ligament. J Minim Invasive Gynecol 2006;13:375-6. [Crossref] [PubMed]
- Grossman SL, Cheung VYT. Round ligament fibroid. J Obstet Gynaecol Can 2007;29:109. [Crossref] [PubMed]
- Kirkham JC, Nero CJ, Tambouret RH, Yoon SS. Leiomyoma and leiomyosarcoma arising from the round ligament of the uterus. J Am Coll Surg 2008;207:452. [Crossref] [PubMed]
- Ali SM, Malik KA, Al-Qadhi H, Shafiq M. Leiomyoma of the Round Ligament of the Uterus: Case report and review of literature. Sultan Qaboos Univ Med J 2012;12:357-9. [PubMed]
- Colak E, Ozlem N, Kesmer S, Yildirim K. A rare inguinal mass: Round ligament leiomyoma. Int J Surg Case Rep 2013;4:577-8. [Crossref] [PubMed]
- Chang TM, Tsui KH, Cheng JT, Liou WS, Yen MS, Wang PH. Chronic pelvic pain secondary to leiomyoma of the round ligament. Taiwan J Obstet Gynecol 2013;52:135-6. [Crossref] [PubMed]
- E H. N S S, P B I. A rare case of round ligament leiomyoma: an inguinal mass. J Clin Diagn Res 2014;8:NJ05-6. [PubMed]
- Canto MJ, Palmero S, Palau J, Ojeda F. Laparoscopic management of a leiomyoma of the round ligament. J Obstet Gynaecol 2015;35:856. [Crossref] [PubMed]
- Birge O, Arslan D, Kinali E, Bulut B. Round ligament of uterus leiomyoma: an unusual cause of dyspareunia. Case Rep Obstet Gynecol 2015;2015:197842. [Crossref] [PubMed]
- Bedir R, Yılmaz R, Şehitoğlu İ, Yurdakul C. Round Ligament Leiomyoma Developing During Pregnancy: A Case Report and Literature Review. Iran J Pathol 2016;11:261-4. [PubMed]
- Najjar M, Mandel M. Round Ligament Leiomyoma Presenting as an Incarcerated Inguinal Hernia: Case Report and Review of the Literature. Case Rep Surg 2016;2016:9380212. [Crossref] [PubMed]
- Efthimiadis C, Ioannidis A, Grigoriou M, Kofina K, Gerasimidou D. Leiomyoma of round ligament mimicking an incarcerated inguinal hernia-report of a rare case. J Surg Case Rep 2017;2017:rjx237. [Crossref] [PubMed]
- Deol M, Arleo EK. Round ligament leiomyoma: a rare manifestation of a common entity. Clin Imaging 2017;42:34-6. [Crossref] [PubMed]
- Kan Ö, Sükür YE, Aytac R. Extraperitoneal leiomyoma of the round ligament of the uterus mimicking adnexal mass. J Obstet Gynaecol 2017;37:257-8. [PubMed]
- Kaya C, Alay İ, Babayeva G, Güraslan H, Ekin M, Yaşar L. Laparoscopic Management of a Torsioned Round Ligament Fibroid. Oman Med J 2018;33:441-3. [Crossref] [PubMed]
- Christodoulou IM, Angelopoulos A, Siaperas P, Ioannidis A, Skarpas A, Tellos A, Velimezis G, Karanikas I. Leiomyoma of the Round Ligament of the Uterus Mimicking Inguinal Hernia. Case Rep Surg 2018;2018:6702494. [Crossref] [PubMed]
- Kypriotis K, Kathopoulis N, Tsiriva M, Zacharakis D, Chatzipapas I, Protopapas A. Leiomyoma originating from left round ligament presents as symptomatic inguinal hernia. Clin Case Rep 2021;9:e04445. [Crossref] [PubMed]
- Tympa A, Grigoriadis C, Terzakis E, Goudeli C, Melemeni A. Leiomyoma of the uterine round ligament: A case report. Exp Ther Med 2021;22:1285. [Crossref] [PubMed]
- Warshauer DM, Mandel SR. Leiomyoma of the extraperitoneal round ligament: CT demonstration. Clin Imaging 1999;23:375-6. [Crossref] [PubMed]
- Lösch A, Haider-Angeler MG, Kainz C, Breitenecker G, Lahodny J. Leiomyoma of the round ligament in a postmenopausal woman. Maturitas 1999;31:133-5. [Crossref] [PubMed]


