
Successful management of traumatic cervical esophageal injury by intraoperative microscopy and esophagoscopic assistance: a case description
Introduction
Anterior cervical discectomy with bone graft fusion has become an effective method for treating various diseases, including cervical degenerative diseases, ossification of the posterior longitudinal ligament (OPLL), trauma, and tumors. Esophageal perforation is a rare complication that occurs after anterior cervical spine surgery. According to reports, the incidence of esophageal perforation is 0.04–0.25% (1-3). Although the incidence of esophageal perforation is very low, its mortality is as high as 20%, representing a fatal risk to patients (4).
The repair of esophageal perforation is a challenging operation. Despite significant advances in surgical technology, leakage and stenosis after repair are still common, which contributes to the increase of postoperative mortality and the decline of quality of life (5). Most perforation repair can be completed successfully when the perforation site has sufficient nutrition, good blood supply, and is tension-free. However, due to the different characteristics of the esophagus itself, the repair of esophageal perforation is more prone to leakage than are most other repairs of gastrointestinal perforation (6). Wang et al. (7) reported leakage rates as high as 25% to 50% for the initial repair of esophageal perforations. Esophageal stenosis often leads to dysphagia, which has an adverse impact on the quality of life of patients. The literature concerning the use of intraoperative technology for esophageal repair to reduce the incidence of postoperative esophageal leakage and stenosis is disputable. In this case of esophageal perforation, the microscope makes the surgical field clear, which supports the fine and tight suturing required at the perforation site, maintaining uniform suture spacing and flat anastomosis and thus preventing poor blood flow and leakage after repair. Esophagoscopy can directly show the perforation site and properly expand the damaged esophageal segment, which facilitates suturing and prevents postoperative stenosis. Overall, the combined application of esophagoscopy and microscopy reduces the difficulty of the operation.
This paper describes a case of a patient undergoing esophageal perforation after anterior cervical surgery. The perforation was successfully repaired with the help of a microscope and esophagoscope. This case provides more information about the diagnosis and treatment of complications of anterior cervical surgery.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the ethics committee of the People’s Hospital of Baoan and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
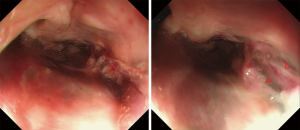
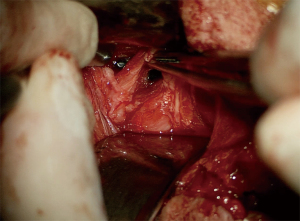
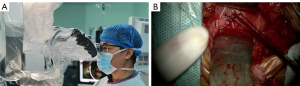
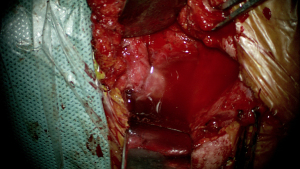
A 63-year-old male underwent an anterior cervical discectomy with bone graft fusion. Three h after the operation, the patient complained of neck wound pain and throat discomfort. Physical examination showed that there was no obvious redness or swelling at the neck incision but that there was a large amount of gas and about 2 mL of bloody drainage fluid in the drainage bag (Figure 1). This led us to suspect perforation of the esophagus, which was ultimately confirmed by emergency upper gastrointestinal endoscopy (Figure 2). Esophageal perforation can be caused by intraoperative traction on the esophagus or tracheal intubation. During the surgical repair, 2 tears about 1 cm long were found on the right wall of the patient’s esophageal opening (Figure 3). The esophagus was fixed with an esophagoscopy, and the esophageal perforation was sutured under a microscope (Figure 4). The diameter of the esophagoscope was 1 cm. The suture type was an absorbable suture manufactured by Johnson & Johnson. The scapuloglossal muscle flap was then filled between the esophagus and the anterior edge of the vertebral body and firmly fixed to the surrounding tissue so that the damaged esophageal wall was completely covered by the muscle flap. After this, esophagoscopy was performed once more, which showed that the esophageal perforation was tightly sutured and that there was no esophageal stenosis. The esophagus was inflated through the esophagoscope, which revealed that there were no bubbles in the water left in the operating area. This reconfirmed that the esophagus was no longer perforated (Figure 5). Vacuum sealing and drainage were subsequently performed in the area of the neck operation, and the neck incision was closed in layers. At the same time, gastrostomy was also performed with the aid of a gastroscope. Intravenous nutritional support and anti-inflammatory treatment were administered after the operation. Enteral nutrition was started on the 12th day after the operation, and oral feeding was started on the 21st day. One month after the operation, esophagoscopy showed that the perforation had completely healed without stenosis (Figure 6).
Discussion
The diagnosis of esophageal perforation should be confirmed by a combination of symptoms, signs, and relevant auxiliary examinations. When there is perforation in the esophagus, the X-ray of the neck can show subcutaneous emphysema, widening of the prevertebral space, and loosening and displacement of hardware. Even so, the missed diagnosis rate is still 10–46% (8). Computed tomography and magnetic resonance imaging of the cervical spine can determine whether hardware is loose or displaced and whether the tissue around the perforation has edema or inflammation. Angiography during swallowing can confirm the presence of esophageal perforation and further determine its location and the degree of exudation. Esophagoscopy can directly observe the location and size of the perforation and the soft tissue around the perforation. Esophagography can also show the location and size of the perforation. At present, the diagnosis of esophageal perforation mainly depends on esophageal endoscopy or esophageal barium meal angiography. Previous studies report that 25% of esophageal angiography examinations produce a false-negative result, which can lead to missed diagnoses and misdiagnoses (9). In this case, the patient suffered from pain in the neck wound and had a large amount of gas in the drainage bag, which led us to suspect perforation of the esophagus. Subsequently, the patient underwent esophagoscopy, and the results confirmed the diagnosis of esophageal perforation.
Four common treatment methods for esophageal perforation exist and are described below: (I) surgical treatment: For a large perforation, it is recommended that patients in good overall condition undergo early surgery, with perforation repair or excision and anastomosis being selected according to the results of intraoperative exploration (10). However, routine surgical repair of esophageal perforation has a high postoperative mortality and complication rate. (II) Esophageal stent implantation: A stent is used to physically cover the perforation. Some centers have reported that esophageal stent implantation seems to be as effective as surgical repair in the treatment of various types of acute perforation, but it involves more postoperative complications, such as chest pain, foreign body sensation, upper gastrointestinal bleeding, esophageal perforation, food impaction, and stent displacement (11,12). The incidence of stent displacement is between 10.2% and 25.9% (13,14). (III) Biological protein gel or gastroscope titanium clip therapy: These apply to smaller perforations. (IV) Nonoperative treatment: This includes intravenous broad-spectrum antibiotics, parenteral nutrition, and cessation of oral feeding.
Some researchers and practitioners suggest that conservative treatment mainly be used for a perforation less than 1 cm in size, with surgery being the first choice for a perforation larger than 1 cm (9,15). However, about 25% of patients who do not receive surgical treatment will develop a cervical abscess (16,17). Perrone et al. (9) reported a mortality rate of surgical treatment for esophageal perforation of 12% and a mortality rate of conservative treatment of 18%. In general, most authors recommend early and active intervention in patients with esophageal perforation because the mortality rate for a treatment time <24 h is 20% while the mortality rate for treatment >24 h is close to 50% (18). Therefore, as long as it is feasible, 1-stage repair should be attempted.
The blood supply to the esophagus is relatively low, the esophageal wall is thin compared with the intestine, and the overall healing speed of the esophagus is slow when stimulated by gastrointestinal secretions (19). Therefore, esophageal perforation is considered to be a complex and challenging condition. The general principles of esophageal perforation treatments are the following: (I) excellent exposure, (II) debridement of inactivated tissue, (III) closure of the defect; (IV) use of muscle flap support, and (V) adequate drainage. Adequate drainage and muscle flap support are the preferred treatments when there is severe inflammation or delayed identification of the injury, or when the location of perforation cannot be determined (20). In this case, because the combined assistance of esophagoscopy and microscope could identify the perforation and facilitate suturing, we chose a 1-stage closure of the perforation.
Leakage and stenosis after esophageal perforation repair contribute to the increase of postoperative mortality and the reduction of quality of life. However, the combined assistance of the microscope and esophagoscope may help to reduce the incidence of leakage and stenosis after perforation repair. This is mainly because the microscope can enlarge the surgical field of vision and provide good lighting conditions which result in an improved tissue recognition rate, more accurate hemostasis, less tissue damage, uniform needle spacing, and flat anastomosis. This ensures the blood supply and reduces the susceptibility to stenosis or embolism (21). In this case, microscope-assisted surgery provided good exposure and repair of the perforation. Ahn et al. (22) showed that it is possible to determine the location of the esophageal perforation through intraoperative palpation and observation of the nasogastric tube, but it may be difficult to detect a tiny perforation with this approach. In our case, there were many advantages of using esophagoscopy in the esophagus during repair. First, flexible esophagoscopy can directly display the perforation site. Second, it is possible to inject normal saline into the operation area and observe the change by inflating the digestive tract to reconfirm the position of a difficult-to-observe perforation and to confirm the tightness of the suture. Third, intraoperative esophagoscopy can maintain the appropriate expansion of the damaged esophagus, which not only provides operation space for the perforation suture but also prevents postoperative stenosis of the perforation repair site. Fourth, because the esophagus itself is soft, it may move when the perforation is being sutured, and the esophagoscope in the esophagus can fix the esophagus to prevent the esophagus from moving, thus facilitating suturing.
While treating esophageal perforation, nutritional support is also essential to ensure adequate nutrition and to avoid stimulation of the perforation site, which enables early and complete healing of the perforation site. Nasal feeding is generally not recommended for patients with an esophageal perforation because it cannot provide the nutritional needs for wound healing and will stimulate the perforation site. Konstantakos et al. (23) reported the use of jejunostomy to avoid long-term damage of a nasogastric tube to mucosa. In this study, gastrostomy, gastrointestinal decompression, and placement of an indwelling jejunal nutrition tube were performed at the same time as the diagnosis of esophageal perforation, which provided the best conditions for early and complete healing of the perforation.
Conclusions
This study shows that using a microscope and an esophagoscope can be a highly effective surgical method for repairing an esophageal perforation.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-3/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the ethics committee of the People’s Hospital of Baoan and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gaudinez RF, English GM, Gebhard JS, Brugman JL, Donaldson DH, Brown CW. Esophageal perforations after anterior cervical surgery. J Spinal Disord 2000;13:77-84. [Crossref] [PubMed]
- Henderson E, Echavé V, Lalancette M, Langlois G. Esophageal perforation in closed neck trauma. Can J Surg 2007;50:E5-6. [PubMed]
- Vogel SB, Rout WR, Martin TD, Abbitt PL. Esophageal perforation in adults: aggressive, conservative treatment lowers morbidity and mortality. Ann Surg 2005;241:1016-21; discussion 1021-3. [Crossref] [PubMed]
- Amhaz HH, Kuo R, Vaidya R, Orlewicz MS. Esophageal perforation following cervical spine surgery: A review with considerations in airway management. Int J Crit Illn Inj Sci 2013;3:276-8. [Crossref] [PubMed]
- Akiyama H. Esophageal anastomosis. Arch Surg 1973;107:512-4. [Crossref] [PubMed]
- Yuan Y, Wang KN, Chen LQ. Esophageal anastomosis. Dis Esophagus 2015;28:127-37. [Crossref] [PubMed]
- Wang N, Razzouk AJ, Safavi A, Gan K, Van Arsdell GS, Burton PM, Fandrich BL, Wood MJ, Hill AC, Vyhmeister EE, Miranda R, Ahn C, Gundry SR. Delayed primary repair of intrathoracic esophageal perforation: is it safe? J Thorac Cardiovasc Surg 1996;111:114-21; discussion 121-2. [Crossref] [PubMed]
- Vrouenraets BC, Been HD, Brouwer-Mladin R, Bruno M, van Lanschot JJ. Esophageal perforation associated with cervical spine surgery: report of two cases and review of the literature. Dig Surg 2004;21:246-9. [Crossref] [PubMed]
- Perrone O, Tassi V, Mattioli B, Daddi N, Uneddu M, Borghesi I, Mattioli S. Pharyngo-oesophageal perforation following anterior cervical discectomy and fusion: management and results. Eur J Cardiothorac Surg 2017;51:160-8. [Crossref] [PubMed]
- Zisis C, Guillin A, Heyries L, Lienne P, D'Journo XB, Doddoli C, Giudicelli R, Thomas PA. Stent placement in the management of oesophageal leaks. Eur J Cardiothorac Surg 2008;33:451-6. [Crossref] [PubMed]
- Doosti-Irani A, Mansournia MA, Rahimi-Foroushani A, Haddad P, Holakouie-Naieni K. Complications of stent placement in patients with esophageal cancer: A systematic review and network meta-analysis. PLoS One 2017;12:e0184784. [Crossref] [PubMed]
- Baerlocher MO, Asch MR, Vellahottam A, Puri G, Andrews K, Myers A. Safety and efficacy of gastrointestinal stents in cancer patients at a community hospital. Can J Surg 2008;51:130-4. [PubMed]
- Selinger CP, Ellul P, Smith PA, Cole NC. Oesophageal stent insertion for palliation of dysphagia in a District General Hospital: experience from a case series of 137 patients. QJM 2008;101:545-8. [Crossref] [PubMed]
- Keller R, Flieger D, Fischbach W, Christl SU. Self-expanding metal stents for malignant esophagogastric obstruction: experience with a new design covered nitinol stent. J Gastrointestin Liver Dis 2007;16:239-43. [PubMed]
- Harman F, Kaptanoglu E, Hasturk AE. Esophageal perforation after anterior cervical surgery: a review of the literature for over half a century with a demonstrative case and a proposed novel algorithm. Eur Spine J 2016;25:2037-49. [Crossref] [PubMed]
- Smith MD, Bolesta MJ. Esophageal perforation after anterior cervical plate fixation: a report of two cases. J Spinal Disord 1992;5:357-62. [Crossref] [PubMed]
- Loop FD, Groves LK. Esophageal perforations. Ann Thorac Surg 1970;10:571-87. [Crossref] [PubMed]
- Hershman SH, Kunkle WA, Kelly MP, Buchowski JM, Ray WZ, Bumpass DB, et al. Esophageal Perforation Following Anterior Cervical Spine Surgery: Case Report and Review of the Literature. Global Spine J 2017;7:28S-36S. [Crossref] [PubMed]
- Reid RR, Dutra J, Conley DB, Ondra SL, Dumanian GA. Improved repair of cervical esophageal fistula complicating anterior spinal fusion: free omental flap compared with pectoralis major flap. Report of four cases. J Neurosurg 2004;100:66-70. [PubMed]
- Sudarshan M, Cassivi SD. Management of traumatic esophageal injuries. J Thorac Dis 2019;11:S172-6. [Crossref] [PubMed]
- Vergara P, Timofeev I. Minimally invasive anterior cervical discectomy and fusion: a valid alternative to open techniques. Acta Neurochir (Wien) 2018;160:2467-71. [Crossref] [PubMed]
- Ahn SH, Lee SH, Kim ES, Eoh W. Successful repair of esophageal perforation after anterior cervical fusion for cervical spine fracture. J Clin Neurosci 2011;18:1374-80. [Crossref] [PubMed]
- Konstantakos AK, Temes RT. Delayed esophageal perforation: a complication of anterior cervical spine fixation. Ann Thorac Surg 2005;80:349. [Crossref] [PubMed]




