
Periureteric venous ring with renal pelvic stones: a case description
Case description
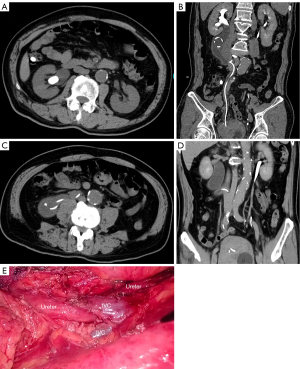
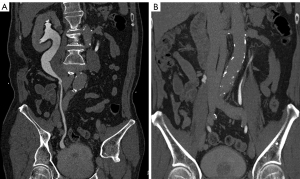
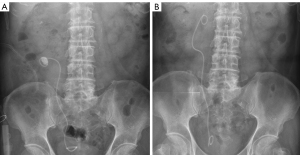
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. A 71-year-old man presented with right back pain and hematuria for 1 week. The patient had pronounced anemia, and his hemoglobin level had dropped from 142 to 76 g/L because of the hematuria. The patient had no obvious urinary frequency, dysuria, or urgency, nor did he have a fever. Physical examination showed no positive findings except for pain in the right renal region on palpation. Urinalysis revealed that his white and red blood cells [WBC 60/high power field (HPF), RBC 90/HPF] were significantly increased. Ultrasound examination showed that the right renal pelvis was separated by 18 mm, that the upper segment of the right ureter was dilated by 16 mm, and that there was a 22 mm × 13 mm strong echo with acoustic shadow 72 mm away from the renal hilum. The enhanced spiral computed tomography (CT) showed multiple stones in the right kidney, the largest being 20 mm × 13 mm, and the right renal pelvis and ureter were obviously dilated. CT confirmed the presence of a periureteral venous ring (Figures 1,2). Unfortunately, no measurement of glomerular filtration rate was performed to assess renal split function due to lack of equipment. A retroperitoneal laparoscopic reconstruction of the ureter was performed with excision of the retrocaval segment of the ureter and uretero-ureteral anastomosis (Figure 1). Three months after reconstruction, the patient’s hemoglobin returned to 135 g/L. Flexible ureteroscopy and holmium laser lithotripsy were performed for the pelvic renal calculi, and the indwelling catheter was removed 1 month after lithotripsy (Figure 3). After 18 months, the patient’s hemoglobin and urinalysis were normal, with no low back pain (Figure 2).
Discussion
Congenital inferior vena cava (IVC) dysplasia with circumcaval ureter, known as retrocaval ureter (RU), is a rare disease with an incidence of 1:1,500 (1,2). Patients with congenital IVC anomalies and a circumcaval ureter usually have no obvious clinical symptoms. They may experience mild backache and microscopic hematuria, and congenital IVC anomalies and a circumcaval ureter is often diagnosed incidentally on imaging studies. Periureteral venous rings are even rarer, with only 15 cases reported since the first case was reported in 1972 (3,4) (Table 1).
Table 1
| Year | Study | Patients (n)/sex | Age (years) | Diagnosis confirmation | Approach |
|---|---|---|---|---|---|
| 1972 | LePage | 1/M | 17 | IVU, inferior VC | Excision of anomalous vein |
| 1979 | Carrion | 1/M | 17 | IVU, inferior VC | Excision of anomalous vein |
| 1980 | Dharman | 1/M | 48 | IVU, RP, inferior VC | Nephroureterectomy |
| 1981 | Radcliffe | 1/M | 22 | IVU | UU |
| 1986 | Hattori | 1/M | 31 | IVU, CTU | NA |
| 1986 | Sasai | 1/F | 36 | IVU, CTU | NA |
| 1989 | Rosen | 1/F | 42 | IVU, CTU, RP | UU |
| 1991 | Dillon | 1/F | 50 | IVU, CTU | NA |
| 2006 | Dillon | 1/F | 17 | CTU, MRU | NA |
| 2010 | Gupta | 1/M | 73 | RP, CTU | Nephroureterectomy with bladder cuff excision |
| 2013 | Paik | 1/F | 50 | MRI | NA |
| 2015 | Sofia | 1/M | 46 | CT | NA |
| 2015 | Giddy | 1/F | 21 | CTU | LP UU |
| 2018 | Naik | 1/F | 25 | CTU | NA |
| 2020 | Rabley | 1/F | 47 | CTU, RP | FUSL |
M, male; F, female; IVU, intravenous urogram; VC, venocavogram; RP, retrograde pyelography; UU, uretero-ureteral anastomosis; CT, computed tomography; CTU, computed tomography urogram; NA, not available; LP, laparoscopic; FUSL, flexible ureteroscopic lithotripsy; MRI, magnetic resonance imaging.
IVC dysplasia can involve the ureter and is characterized by developmental abnormalities, such as duplication and aplasia. McClure and Butler hypothesized that the infrarenal portion of the IVC is formed primarily from the supracardinal vein (5). If the posterior cardinal vein does not regress, the infrarenal portion of the IVC originates mainly from the posterior cardinal vein, resulting in a RU as the ureter spirals from the dorsolateral to the ventromedial position around the posterior cardinal vein. Duplication mainly refers to a double IVC, often located on both sides of the abdominal aorta. If both are located on the right side, it is a right double IVC, categorized as either a complete or partial right double IVC. A complete right double IVC refers to the complete separation of the infrarenal portion of the IVC. A partial right-sided double IVC refers to the partial division of the infrarenal portion of the IVC and re-fusion above the bifurcation of the IVC to form a venous ring, with the ureter passing through the venous ring. To avoid confusion, LePage et al. and McClure and Butler have named this type of RU a periureteral venous ring (3,5). The normal development of the supracardinal vein without regression of the posterior cardinal vein results in a periureteral venous ring (5). Gupta and Nayyar used a schematic diagram to describe the mechanism of the generation of a periureteric vena cava (6).
In 1972, LePage reported the first case of a periureteral venous ring and relieved the ureteral obstruction by excision of the abnormally unregressed veins (3). To date, only 15 cases of periureteral venous rings have been reported in the literature (Table 1): in 2 patients, the ureteral obstruction was relieved by excision of the restricting portion of the anomalous vein (3); 1 patient with a nonfunctioning kidney underwent nephroureterectomy; 1 patient with suspected renal pelvis tumor underwent nephroureterectomy with bladder cuff excision; 3 patients underwent uretero-ureteral anastomosis; 1 patient with ureteral calculi underwent ureteroscopic holmium laser lithotripsy; and 7 patients with hydronephrosis did not worsen during follow-up, and they did not undergo any surgical treatment.
In 1994, Baba (7) was the first to report using laparoscopic techniques to treat RU. In 1999, Salomon performed the first retroperitoneal laparoscopic surgery for retrocaval ureteroplasty (8). Laparoscopy repair for the treatment of RU has obvious advantages: less blood loss during the surgery, shorter hospital stays, less postoperative pain, and a superior esthetic effect (9-11). In our case, the patient had marked hematuria and anemia prior to reconstruction. After surgery, the patient’s hemoglobin returned to normal levels, so the patient’s symptoms were mainly related to the periureteral venous rings.
Management of this condition depends on the patient’s clinical symptoms and the severity of the effect on renal function. Asymptomatic patients may not require any treatment. Patients with significant obstructive nephropathy usually require surgical intervention. Surgical treatment involves excision and uretero-ureteral anastomosis of the ureter. Retroperitoneal laparoscopic ureteroplasty has obvious advantages in treating periureteral venous rings, as it allows for simultaneous treatment of renal pelvic stones. Renal pelvic stones may be treated by flexible ureteroscopy in 2 stages. Thus far, only 15 cases of periureteral venous rings have been reported in the literature, including 1case of periureteral venous rings with kidney stones (Table 1). Our report provides insights into the management of this extremely rare disease.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-259/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhang XD, Hou SK, Zhu JH, et al. Diagnosis and treatment of retrocaval ureter. Eur Urol 1990;18:207-10. [Crossref] [PubMed]
- Ichikawa T, Ono S, Nagafuji Y, et al. Congenital venous anomalies associated with retrocaval ureter: evaluation using computed tomography. Folia Morphol (Warsz) 2022; Epub ahead of print. [Crossref] [PubMed]
- LePage JR, Baldwin GN. Obstructive periureteric venous ring. Radiology 1972;104:313-5. [Crossref] [PubMed]
- Rabley A, Singh D, Rawlings T, et al. Asymptomatic Obstructive Ureterolithiasis Due to a Periureteral Venous Ring. J Endourol Case Rep 2020;6:505-8. [Crossref] [PubMed]
- McClure CFW, Butler EG. The development of the vena cava inferior in man. American Journal of Anatomy 1925;35:331-83. [Crossref]
- Gupta NP, Nayyar R, Sahay SC. Periureteric venous ring with renal calculi and transitional cell carcinoma: report of a rare case. Surg Radiol Anat 2010;32:405-7. [Crossref] [PubMed]
- Baba S, Oya M, Miyahara M, et al. Laparoscopic surgical correction of circumcaval ureter. Urology 1994;44:122-6. [Crossref] [PubMed]
- Salomon L, Hoznek A, Balian C, et al. Retroperitoneal laparoscopy of a retrocaval ureter. BJU Int 1999;84:181-2. [Crossref] [PubMed]
- Abdessater M, El Khoury R, Elias S, et al. Diagnosis and laparoscopic management of retrocaval ureter: A review of the literature and our case series. Int J Surg Case Rep 2019;59:165-75. [Crossref] [PubMed]
- Escolino M, Masieri L, Valla JS, et al. Laparoscopic and robotic-assisted repair of retrocaval ureter in children: a multi-institutional comparative study with open repair. World J Urol 2019;37:1941-7. [Crossref] [PubMed]
- Gokcen K, Dundar G, Gokce G, et al. Laparoscopic transperitoneal repair of retrocaval (circumcaval) ureter. Int Braz J Urol 2018;44:649-50. [Crossref] [PubMed]


