
Cystic lesions of the humeral head on magnetic resonance imaging: a pictorial review
Introduction
Cystic lesions of the proximal humerus are commonly encountered on routine shoulder magnetic resonance imaging (MRI). True cysts are defined as fluid-filled structures or lesions with an epithelial lining, whereas pseudocysts are fluid-filled lesions without epithelial lining. In this paper, the terms “cyst” and “cystic lesion” are used to encompass both true cysts, pseudocysts and other lesions which could mimic the appearance of a cyst on MRI, with increased signal on fluid sensitive sequences.
Cystic lesions observed in humeral heads are most commonly degenerative cysts in subcortical or subchondral locations, with other differentials being calcific tendinitis with osseous involvement, perianchor cysts, abscesses or tumours. Table 1 highlights how common these different causes of cystic lesions are.
Table 1
| Lesion | Frequency data |
|---|---|
| Common lesions | |
| Subchondral cystic change | Prevalence of 72% (1) |
| Subcortical cystic changes of humeral tuberosity | Prevalence of 15–45% (2) |
| Perianchor cystic change | Prevalence of 60% following rotator cuff surgery at 6 months (3) |
| Rare lesions | |
| Calcific tendinitis | Prevalence of 3% in the general population (4); osseous involvement occurs in 5% of these cases (5) |
| Osteomyelitis | Annual incidence of 0.0076%, with humeral involvement in 5.5% of cases—Brodie’s abscess occurs in a minority of these cases (6) |
| Bone tumours | Depends on the specific tumour |
On MRI, the location, distribution and morphology of cystic lesions can help point towards a specific diagnosis which carries its own clinical relevance. Knowledge of this may help target the search for underlying pathology that may be causing the cysts. One example would be the lesser tuberosity cyst, which can occur in the context of subscapularis tendinosis. Noting the patient’s demographic, presentation and past surgical history is also valuable. Other imaging modalities such as X-rays, are often complementary.
With a wide spectrum of causes, it is important for the radiologist to have an approach to differentiate the cystic lesions associated with underlying pathology and the ones requiring further investigation and management, from those that do not warrant intervention. This pictorial review aims to provide the radiologist with an approach to various cysts and cyst-like lesions that can be identified on imaging, with specific focus on MRI.
Differential diagnosis
Using the surgical sieve, the cystic lesions in the humeral head can be further categorised into: degenerative changes (which includes both subcortical cysts in various characteristic locations in humeral heads and subchondral cysts), depositional lesions, iatrogenic lesions, infections and tumours.
Degenerative lesions
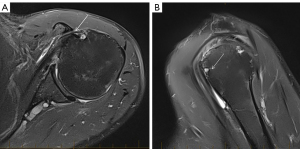
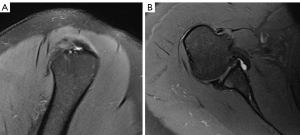
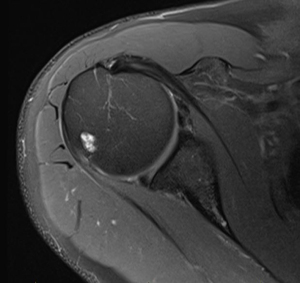
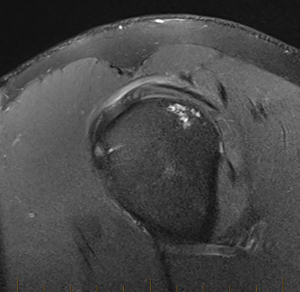
Subcortical cystic changes of the humeral tuberosities (shown in Figures 1-4) have an incidence of 15% to 45% in asymptomatic shoulders, with an association with ageing and rotator cuff pathology (2). They may be further divided based on location, into bare-area, lesser tuberosity, anterior greater tuberosity and posterior greater tuberosity cysts (2,7).
On MRI, subcortical cysts are seen at the tuberosities and bare area of the humerus as round lesions with low T1 and high T2 signal. These should be differentiated from vascular channels which are connected to tubular structures (2).
Bare-area cysts, located in the posterosuperior humeral head, are most common and are associated with ageing (2,7). They are typically pseudocysts communicating with the joint space and likely represent a normal anatomical variant, with no correlation with rotator cuff tears (2,7,8).
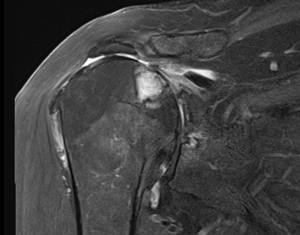
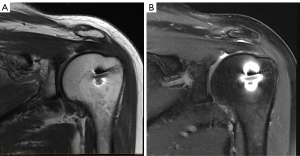
Lesser tuberosity cysts are also more frequent with older age and may be associated with subscapularis tears (2). In the younger demographic, they may also be associated with subcoracoid impingement (shown in Figure 1), which occurs when the subscapularis tendon is impinged between the coracoid process and the lesser tuberosity (9). This syndrome presents with anterior shoulder pain aggravated by adduction and internal rotation, and physical examination reveals point tenderness at the subcoracoid area (9).
On MRI, there may be increased soft tissue noted in the subcoracoid space due to compression and oedema of the subscapularis tendon. The distance between the coracoid tip and the closest point on the proximal humerus should be noted, with a distance of less than 6.8 mm supporting impingement (9). However, as the sensitivity of MRI in detecting subcoracoid impingement is low, direct arthroscopic observation may be needed to establish this diagnosis in patients with supportive clinical features and equivocal imaging (9). The first-line management is physiotherapy and activity modification, with surgery being considered if conservative measures are unsuccessful (9).
Anterior greater tuberosity cysts located near the insertion of the supraspinatus, and posterior greater tuberosity cysts located near the insertion of the infraspinatus, are associated with the presence of supraspinatus and infraspinatus tendon tears (2). Their pathogenesis is unclear, but theories include the cysts being an inflammatory reaction to microavulsive cuff tears, or a result of synovial fluid contacting the bone while intact tendons would have normally served as a barrier against this (2,10). However, given they are also common in asymptomatic shoulders, some suggest these cysts may be a normal variant unrelated to shoulder pathology or ageing (2). The majority of humeral tuberosity cysts are asymptomatic and require no treatment, although bone grafting may be needed in large cases interfering with rotator cuff repair (10).
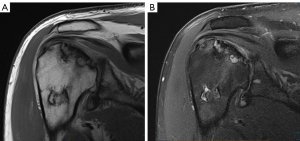
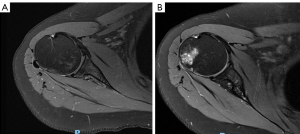
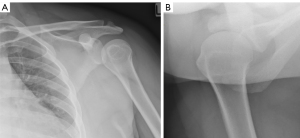
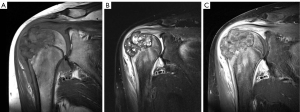
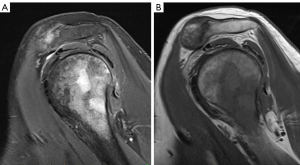
Posterior greater tuberosity cysts may be associated with posterosuperior (internal) impingement (shown in Figures 2,3), which describes the compression of the supraspinatus and infraspinatus tendons between the greater tuberosity and the posterosuperior glenoid rim (11,12). It classically occurs in overhead athletes and presents with posterior shoulder pain worsened by external rotation and abduction (11,12). MRI findings include cystic change at the site of infraspinatus attachment, undersurface tears of the anterior infraspinatus and posterior supraspinatus fibres and fraying or tearing of the posterosuperior glenoid labrum (12). Physiotherapy is the mainstay of management, with surgery in selected cases (11).
Subchondral cysts of the proximal humerus occur in the context of degenerative glenohumeral joint diseases, such as osteoarthritis (shown in Figure 5), rheumatoid arthritis, avascular necrosis (shown in Figure 6), crystal deposition disease, haemophilic arthritis, intraosseous ganglia and trauma (1). They are not true cysts as they lack an epithelial lining (13). The bony contusion theory posits that subchondral cysts develop from focal bone necrosis induced by abnormal stress on bony surfaces in a degenerated joint, whereas the synovial fluid intrusion theory suggests that they develop as a result of synovial fluid infiltrating the bone through damaged cartilage (1,13). Subchondral cysts are generally considered asymptomatic, although there may be a weak correlation between bone marrow oedema, which these cysts are associated with, and pain severity in osteoarthritis (14,15). The patient’s clinical features and management will vary depending on the underlying cause.
The subchondral cyst differs from the aforementioned subcortical cyst as it is situated deep to or at the articular surface of the humeral head lined by cartilage. On MRI, subchondral cysts show fluid-like signal and, in early stages, a bone marrow oedema pattern of T2 fat-suppressed hyperintensity of bone marrow (16). The diagnosis should be considered when associated features of degenerative joint diseases, such as cartilage erosion/thinning and osteophytes, are present (13). These subchondral cysts can affect the bone stock of the humerus that can in turn, have implications for type of joint replacement performed. Hence, if extensive, it may be worthwhile conveying the size and extent of these cysts for the orthopaedic referrer. Bone stock can be better assessed on computed tomography (CT) (17).
Depositional lesions
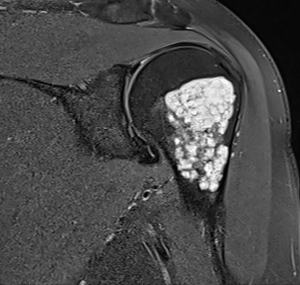
Osseous involvement in calcific tendinitis can produce cyst-like change in the humerus (shown in Figure 7) (4). Calcific tendinitis is a common disease, affecting 3% of adults, characterised by the deposition of calcium hydroxyapatite crystals in and around tendons as a result of trauma, hypoxia and metabolic derangement (4). The shoulder is the most commonly affected site and symptoms include pain, swelling and erythema. Osseous involvement is uncommon and may result from periosteal reactivity in response to crystal-induced tendon inflammation (4). The mechanism of cystic change in calcific tendinosis is unclear; it may be due to calcium accumulation on pre-existing tuberosity cysts, or it may develop as a reactive response to intramedullary crystal deposition (4). It is important to differentiate the osseous changes of calcific tendinitis from neoplastic lesions to avoid more invasive investigation or unnecessary biopsies. The former is easily managed with cortisone injection and anti-inflammatories (4).
On MRI, deposits of calcific tendinitis are observed as T1 and T2 hypointensities within the cystic lesions, with inflammatory oedema manifesting as T2 hyperintensity around tendons (4). Cortical bone erosion and marrow extension, evidenced by heterogenous marrow signal intensity adjacent to tendon calcification, are supporting features (4). Prior or ancillary imaging demonstrating calcium deposit in adjacent tendons, such as on X-ray, may help support the diagnosis.
Iatrogenic lesions
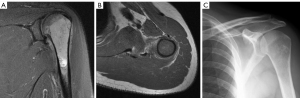
The perianchor cyst (shown in Figure 8) is an osteolytic lesion which may be found incidentally in patients following rotator cuff repairs using suture anchors (18). Perianchor cysts are more common with the use of bioabsorbable anchors. In a study of 100 patients treated with bioabsorbable suture anchors and 100 patients treated with non-absorbable anchors, Micic et al. reported a 12-month incidence of 39% and 6%, respectively (18). They may arise due to synovial fluid entering the bone through cracks produced by the surgeon drilling a hole for anchor insertion (18). Their association with bioabsorbable anchors may be related to the design of these anchors allowing fluid infiltration more easily along the sutures and through the central hole of the anchor (18). These are not associated with impaired postoperative outcomes, do not increase the incidence of rotator cuff retear or shoulder instability and the majority self-resolve by 18 months post-surgery (3,18). These can be mistaken as post-operative infection and the lack of clinical features such as fever may be a useful distinguishing feature.
On MRI, perianchor cysts are seen as collections near the anchor which are hyperintense on fluid-sensitive sequences. They may be graded by size in relation to the anchor (3).
Technical artefacts
Susceptibility artefacts may mimic humeral cysts, as shown in Figure 9. They occur due to the hardware used and associated paramagnetic effects. Magnetic field distortion can be observed to differentiate this artefact from true pathology.
Infectious lesions
Infectious cystic lesions must be considered in the context of pain, swelling and fever (19). When considering Brodie’s abscess as a differential for the cystic lesion, it is important to look for the penumbra sign, which describes four layers of the abscess: a core of T1 hypointensity and T2 hyperintensity, an inner ring of T1 intermediate signal and T2 hypointensity, an outer ring of T1 and T2 hypointensity and surrounding bone marrow oedema (19,20). The abscess enhances peripherally with contrast (19,20). These lesions are managed with antibiotics and may need surgical drainage (20).
Pseudolesions on X-ray that may masquerade as cystic lesions
Pseudolesions of the humerus can appear as cysts, but do not represent a true pathological process. They are commonly seen on internal rotation shoulder radiographs as a radiolucent lesion with a sclerotic border in the humeral head (21). These pseudolesions can be differentiated from true osteolytic lesions as they are absent on externally rotated and other shoulder views (21). An example is shown in Figure 10.
Another type of pseudolesion occurs in the superolateral humeral head as a result of normal anatomical variation with trabecular bone loss and increased fat (21). This radiolucency is seen best on externally rotated radiographs and appears as a region of increased fat-signal on MRI (21).
Tumours
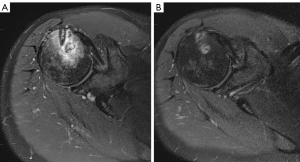
Tumours (shown in Figures 11-14) should always be considered in the differential diagnoses of cysts. These include benign and malignant primary tumours and those secondary to a metastatic aetiology. An example of a tumour which can sometimes be mistaken for a cystic lesion is the chondroid tumour, given its intrinsically hyperintense signal on fluid-sensitive sequences. A useful distinguishing feature is its lobulated contour. Other imaging characteristics that can help separate a neoplastic process from a cystic lesion of the humeral head is the internal architecture of the lesion; if a lesion has an internal solid component or septation, it is more likely to be neoplastic. Surrounding marrow oedema signal or extraosseous breach would also be more supportive of a malignant process. Occasionally, it can be challenging to differentiate soft tissue tumours or juxtacortical lesions with bone invasion from primary bone tumours with extraosseous extension (22). Using the epicentre of a lesion can help localise its origin.
The details of specific neoplasms are beyond the scope of this manuscript.
The simple (unicameral) humeral bone cyst is a non-neoplastic bone tumour which may be considered in the differential diagnosis of cystic change in the humeral head, although this lesion usually occurs in the metaphysis and diaphysis rather than the humeral head (23).
Summary and approach to cystic lesions of the humeral head
Once a cystic lesion is identified in the humeral head, characterised by T1 hypointensity and T2, PD, PDFS or STIR hyperintensity, the most useful step in determining its aetiology and associations is noting its location. A summary of this approach is provided in Figure 15. The patient’s clinical presentation should be considered, for example posterior shoulder pain and instability in a throwing-athlete will support the diagnosis of posterosuperior impingement. Prior imaging is also useful, particularly in cases of calcific tendinosis with osseous involvement.

Contrast-enhanced MRI (CE-MRI) is useful in differentiating the non-enhancing necrotic and enhancing vascularised areas of bone tumours. This can help avoid sampling necrotic areas during biopsy (19). CE-MRI also highlights the changes of osteomyelitis, such as peripheral enhancement of abscesses (part of the penumbra sign) and sinus tracts (20).
Advanced MRI techniques are not routinely needed to help characterise cystic lesions in the humeral head, although they can be useful in the workup of neoplastic lesions.
For instance, diffusion weighted imaging (DWI) is valuable in differentiating benign and malignant bone lesions. As a lower apparent diffusion coefficient (ADC) can reflect increased cell number and size, malignant tumours tend to have lower ADC values than benign tumours. An ADC of 0.67 and above suggests a benign process. This has a sensitivity of 94%, specificity of 79% and accuracy of 87% (24).
Dynamic CE-MRI can help differentiate tumours from surrounding inflammatory change or post-therapeutic change such as haematoma or seroma, as tumours will show earlier enhancement (19). The details of these techniques are beyond the scope of the manuscript.
Conclusions
This manuscript provides a basic framework to approaching cystic lesions in shoulder imaging, with specific focus on MRI. With the increased utilisation of shoulder MRI, it is useful to be able to differentiate cystic changes which are benign in nature from those that carry clinical implications or point to underlying pathology.
Acknowledgments
Part of this manuscript was presented as an educational poster at the European Congress of Radiology 2022.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-108/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethics was waived for this pictorial essay.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jin W, Ryu KN, Park YK, Lee WK, Ko SH, Yang DM. Cystic lesions in the posterosuperior portion of the humeral head on MR arthrography: correlations with gross and histologic findings in cadavers. AJR Am J Roentgenol 2005;184:1211-5. [Crossref] [PubMed]
- Gwark JY, Park TS, Park HB. Association between the location of tuberosity cysts and rotator cuff tears: A comparative study using radiograph and MRI. J Orthop Surg (Hong Kong) 2019;27:2309499019825762. [Crossref] [PubMed]
- Chung SW, Lee YS, Kim JY, Lee JH, Ki SY, Oh KS, Yoon JP, Kim JY. Changes in Perianchor Cyst Formation Over Time After Rotator Cuff Repair: Influential Factors and Outcomes. Am J Sports Med 2019;47:165-72. [Crossref] [PubMed]
- Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, Kransdorf MJ. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol 2003;181:965-72. [Crossref] [PubMed]
- Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM. Retrospective study of sonographic findings in bone involvement associated with rotator cuff calcific tendinopathy: preliminary results of a case series. Radiol Bras 2015;48:353-7. [Crossref] [PubMed]
- Ma X, Han S, Ma J, Chen X, Bai W, Yan W, Wang K. Epidemiology, microbiology and therapeutic consequences of chronic osteomyelitis in northern China: A retrospective analysis of 255 Patients. Sci Rep 2018;8:14895. [Crossref] [PubMed]
- Sano A, Itoi E, Konno N, Kido T, Urayama M, Sato K. Cystic changes of the humeral head on MR imaging. Relation to age and cuff-tears. Acta Orthop Scand 1998;69:397-400. [Crossref] [PubMed]
- Kadi R, Milants A, Shahabpour M. Shoulder Anatomy and Normal Variants. J Belg Soc Radiol 2017;101:3. [Crossref] [PubMed]
- Okoro T, Reddy VR, Pimpelnarkar A. Coracoid impingement syndrome: a literature review. Curr Rev Musculoskelet Med 2009;2:51-5. [Crossref] [PubMed]
- Chillemi C, Paglialunga C, Guerrisi M, Mantovani M, Osimani M. Arthroscopic Transosseous Repair of Rotator Cuff Tear and Greater Tuberosity Cysts. Arthrosc Sports Med Rehabil 2020;2:e241-50. [Crossref] [PubMed]
- Manske RC, Grant-Nierman M, Lucas B. Shoulder posterior internal impingement in the overhead athlete. Int J Sports Phys Ther 2013;8:194-204. [PubMed]
- Giaroli EL, Major NM, Higgins LD. MRI of internal impingement of the shoulder. AJR Am J Roentgenol 2005;185:925-9. [Crossref] [PubMed]
- Li G, Yin J, Gao J, Cheng TS, Pavlos NJ, Zhang C, Zheng MH. Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes. Arthritis Res Ther 2013;15:223. [Crossref] [PubMed]
- Audrey HX, Abd Razak HR, Andrew TH. The truth behind subchondral cysts in osteoarthritis of the knee. Open Orthop J 2014;8:7-10. [Crossref] [PubMed]
- Vincent TL. Peripheral pain mechanisms in osteoarthritis. Pain 2020;161:S138-46. [Crossref] [PubMed]
- Carrino JA, Blum J, Parellada JA, Schweitzer ME, Morrison WB. MRI of bone marrow edema-like signal in the pathogenesis of subchondral cysts. Osteoarthritis Cartilage 2006;14:1081-5. [Crossref] [PubMed]
- Sharifi A, Siebert MJ, Chhabra A. How to Measure Glenoid Bone Stock and Version and Why It Is Important: A Practical Guide. Radiographics 2020;40:1671-83. [Crossref] [PubMed]
- Micic I, Kholinne E, Kwak JM, Koh KH, Jeon IH. Osteolysis is observed around both bioabsorbable and nonabsorbable anchors on serial magnetic resonance images of patients undergoing arthroscopic rotator cuff repair. Acta Orthop Traumatol Turc 2019;53:414-9. [Crossref] [PubMed]
- Nascimento D, Suchard G, Hatem M, de Abreu A. The role of magnetic resonance imaging in the evaluation of bone tumours and tumour-like lesions. Insights Imaging 2014;5:419-40. [Crossref] [PubMed]
- Wright WF. "Penumbra sign" of Brodie's abscess. Braz J Infect Dis 2020;24:264-5. [Crossref] [PubMed]
- Mhuircheartaigh JN, Lin YC, Wu JS. Bone tumor mimickers: A pictorial essay. Indian J Radiol Imaging 2014;24:225-36. [Crossref] [PubMed]
- Ferguson PC, Griffin AM, O'Sullivan B, Catton CN, Davis AM, Murji A, Bell RS, Wunder JS. Bone invasion in extremity soft-tissue sarcoma: impact on disease outcomes. Cancer 2006;106:2692-700. [Crossref] [PubMed]
- Noordin S, Allana S, Umer M, Jamil M, Hilal K, Uddin N. Unicameral bone cysts: Current concepts. Ann Med Surg (Lond) 2018;34:43-9. [Crossref] [PubMed]
- Geneidi EASH, Ali HI, Dola EF. Role of DWI in characterization of bone tumors. The Egyptian Journal of Radiology and Nuclear Medicine 2016;47:919-27. [Crossref]


