
Stent-in-stent technique under fluoroscopy for removal of embedded esophageal stent: a retrospective case series
Introduction
Esophageal metallic stent placement is an effective and widely used method for treatment of benign and malignant esophageal stenosis and fistulas (1-3). However, problems such as esophageal restenosis, stent fracture, complaints of retrosternal pain and foreign body sensation, hiccups, gastroesophageal reflux, airway compression, or bleeding may necessitate stent removal in some patients (4,5). Removal can usually be safely performed via gastroscopic or interventional radiology approaches. However, because the stent acts as a foreign body, tissue overgrowth often occurs at both ends of the stent after long-term placement and makes stent removal difficult in some patients.
Several authors have reported successful gastroscopic removal of embedded esophageal stents using stent-in-stent (SIS) technique (6-8). In our previous study, we applied the SIS technique to remove an incarcerated airway stent (9). Inspired by these descriptions, we applied the SIS technique under fluoroscopy. The purpose of this paper was to describe the SIS technique for removal of esophageal metallic stent under fluoroscopy and to retrospectively evaluate the safety and efficacy of the method. We present the following article in accordance with the AME Case Series reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-21-1039/rc).
Methods
The data of 25 consecutive patients who underwent metallic esophageal stent removal by the SIS technique under fluoroscopy from May 2017 to June 2021 were analyzed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of the First Affiliated Hospital of Zhengzhou University (No. 2017-C01) and informed consent was taken from all the patients.
Patients were eligible for inclusion in this study if (I) they had severe restenosis after esophageal stent placement and presented with difficulty in swallowing fluids; (II) computed tomography (CT), esophagography, or endoscopy showed deeply embedded stent or stent displacement without effective blockage of fistula; and (III) esophageal stent removal was by the SIS technique under fluoroscopy. Patients with slightly embedded esophageal stent and those not treated by the SIS technique were excluded from this study.
Procedure
Placement of the second self-expanding metal stent
For the procedure, patients were admitted to hospital and fasted overnight for 6–8 h. Diazepam and anisodamine were administered intramuscularly 30 min before the procedure, and lidocaine gel was given orally for local anesthesia.
The procedure was performed under fluoroscopy. The patient was placed supine on the digital subtraction angiography (DSA) bed, and 37% ioversol (Jiangsu Hengrui Medicine Company, Lianyungang, China) was administered orally. The location and degree of esophageal stenosis were determined by fluoroscopy in the supine and the 45° left anterior oblique position. Then, under fluoroscopic monitoring, a 5-F catheter and 0.035-inch guide wire were cooperatively inserted through the mouth into the esophagus and advanced past the first stent until the tip of the guide wire was in the gastric cavity. Then, the second stent (Nanjing Micro-Tech Medical Company, Nanjing, China), along with the double-fold retrievable wire and transporter, was passed over the guide wire. The diameter of the second stent was the same as, or 2 mm larger than, the diameter of the first stent, and the length was 2–4 cm longer than that of the first esophageal stent. The second stent was released at the center of the original esophageal stent. After confirming correct placement of the stent, the double-fold retrievable thread was brought into the nasal cavity from the mouth with the help of a suction catheter and fixed at the side of the ear.
Postoperative management
After implantation of the second stent, the patients were closely monitored for 3 days. If there was choking, obvious pain, or severe foreign body sensation, esophagography was performed and, if necessary, the second stent was removed immediately. At 4 weeks after the second stent implantation, all patients underwent CT and esophagography for evaluation of the general situation of the esophagus. If esophagography showed smooth passage of contrast medium and CT showed no obvious granulation tissue at both ends of the stent, the stent was removed. If CT and esophagography showed persisting granulation tissue proliferation, stent removal was delayed until the granulation tissue had subsided sufficiently.
Removal of the stents
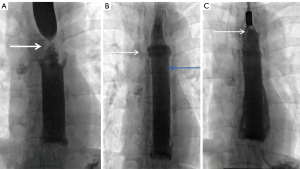
The second stent was removed 4 weeks after implantation. The stent removal device was shown in Figure 1. Preoperative preparation and esophagography were performed as before. The double-fold retrievable thread of the second stent was brought into the oral cavity. Under fluoroscopy, steady traction on the thread was used to pull the stent out. If undue resistance was encountered, an esophageal stent-removal sheath was passed along the double-fold retrievable thread up to the upper end of the stent. With the sheath fixed, the thread was pulled to stretch the upper end of the stent and make it cone shaped, then the double fold retrievable thread and sheath were together pulled to slowly extract the second stent (Figure 2).
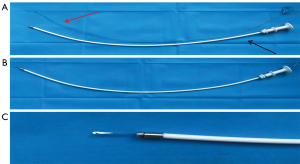
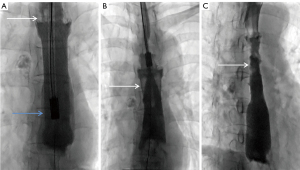
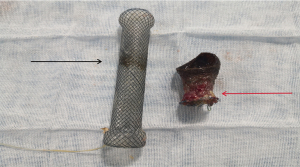
The first stent was then removed. Under fluoroscopy, a catheter and guide wire were cooperatively inserted through the mouth into the esophagus and past the stent into the gastric cavity. An esophageal stent-removal sheath (Nanjing Micro-Tech Medical Company, Nanjing, China) was passed along the guide wire up to the lower end of the stent. Then, an esophageal stent removal hook (diameter, 1 mm; Nanjing Micro-Tech Medical Company, Nanjing, China) was inserted into the esophageal stent-removal sheath, and the nitinol wire of the lower part of the first esophageal stent was hooked and pulled out by the inversion technique (Figure 3). Photograph of both esophageal stents after removal was shown in Figure 4. The technology is completed by the same radiologist (with more than 10 years of working experience).
Vital signs and bleeding were monitored during 24 h after the procedure. If there were no complications, the patient was discharged from hospital 72 h after the procedure.
Results
The 25 patients were in the age range of 48–90 years. Table 1 summarized the characteristics of the patients. Four patients had benign esophageal stricture (one esophageal granulomatous inflammation, one esophageal compression by lung cancer, and two corrosive strictures); two patients had malignant esophageal stricture (esophageal squamous cell carcinoma); four patients had esophagotracheal fistula (not caused by cancer); and fifteen patients had esophagogastric anastomotic stenosis (two confirmed by pathology as anastomotic tumor recurrence). In 15 patients, the second esophageal stent was successfully removed by pulling on the double-fold retrievable thread. In the other 10 patients, the help of the esophageal stent-removal sheath was required because strong resistance was experienced when pulling on the double-fold retrievable thread.
Table 1
| Characteristics | Data |
|---|---|
| Sex | |
| Male | 14 (56%) |
| Female | 11 (44%) |
| Age (years), median | 66 |
| Comorbidities | |
| None | 13 (52%) |
| Hypertension | 7 (28%) |
| Diabetes | 3 (12%) |
| Cerebral infarction | 2 (8%) |
| Smoking history | 8 (32%) |
| Tumor stage | |
| T3N3M1 | 2 (9.52%) |
| T3N3M0 | 3 (14.29%) |
| T3N2M0 | 7 (33.33%) |
| T3N1M0 | 3 (14.29%) |
| T3N0M0 | 4 (19.05%) |
| T2N3M0 | 1 (4.76%) |
| T2N2M0 | 1 (4.76%) |
| Reason for stent placement | |
| Esophageal stricture | 6 (24%) |
| Anastomotic stenosis (after esophageal cancer surgery) | 15 (60%) |
| Esophagotracheal fistula (after esophageal cancer surgery) | 4 (16%) |
| Indwelling time of the first stent (days), median | 505.5 |
| Indwelling time of the second stent (days), median | 26 |
| Time taken for stent removal (min), median | 12.5 |
In 23 patients, the first esophageal stent was successfully removed at the first attempt by the inversion technique. In the other two patients, stent fracture occurred during removal as the wires were corroded because of the prolonged indwelling time of the stent. Most of the nitinol wires were removed during the procedure itself, but gastroscopy was required for removal of some residual wires.
The average procedure time for removal of both esophageal stents was 16.2 min. No serious complications such as esophageal mucosal necrosis, esophageal rupture, esophageal hemorrhage, or mediastinal abscess occurred in any patient.
Discussion
Removal of the embedded esophageal stent by the traditional extraction techniques may result in serious esophageal tear. However, the SIS technique suppresses granulation tissue proliferation at both ends of the stent and reduces the risk. Currently, the three commonly used methods for removal of esophageal stent are surgical resection (10), removal under fluoroscopy (11), and removal under endoscopy (8,12). Surgical resection is traumatic and can cause complications such as anastomotic stricture and anastomotic leakage; therefore, it is rarely used nowadays. Removal under fluoroscopy is easily performed for esophageal stents with short indwelling time, but it is difficult for stents with prolonged indwelling time, when there may be severe granulation hyperplasia. Endoscopic removal of esophageal stent can be performed through several approaches, including combined cryoablation and SIS technique (13), double-step invagination technique (14), inversion technique (15), and rat-tooth forceps or rat-tooth forceps with a snare technique (16). With extended periods of stent placement, the stent tends to get embedded in tissue, and the upper and lower ends of the stent may be severely narrowed. Direct removal of such embedded esophageal stents can cause serious complications such as esophageal mucosal tear, esophageal rupture, and massive hemorrhage. Thus, the endoscopic procedure can be complex and time taking, and so requires the services of an experienced endoscopic surgeon (17,18). In addition, endoscopic stent removal is usually carried out under general anesthesia, and so the patient also has to bear the anesthetic risks. In this study, the SIS technique was successfully used to remove embedded esophageal stents in 25 patients, with no serious complications (e.g., massive bleeding and esophageal rupture) occurring during or after the operation. In two patients who had had stent placement for long durations, the corroded metal wires of the original stent fractured, and some fragments had to be removed endoscopically.
For patients with embedded esophageal stent and hyperplasia-induced stenosis, the SIS technique under endoscopy has been demonstrated to be effective and safe (7,17,19). We therefore adapted the SIS technique for the interventional radiology approach. Under fluoroscopy, a second esophageal stent with a diameter slightly larger or equivalent to that of the original stent is placed. The radial force exerted by the second stent causes necrosis of the proliferating granulation tissue (20), thus facilitating the removal of the original embedded stent.
In contrast to endoscopic esophageal stent removal, interventional radiology procedures are generally carried out under local anesthesia on conscious patients. Our patients were all elderly and in poor physical condition, and therefore unfit for general anesthesia; stent removal under local anesthesia and sedation was therefore preferred. The process is simple, with the stent being extracted by the guide wire or by a stent retrieval hook applied at the upper or lower end of stent. This minimally invasive method rarely causes serious complications such as esophageal rupture and massive hemorrhage. In our study cohort, no serious complications occurred, and the median time taken for stent removal was only 12.5 min.
In the present study, the second stent was placed for a median duration of 26 days before removal; this is consistent with the 2–3 weeks reported in previous studies. None of our patients developed severe granulation hyperplasia, though one patient did have mild granulation hyperplasia at the upper end of the second stent. In our series, one patient developed airway compression after placement of the second stent, necessitating its early removal. Because the indwelling time of the second stent was too short, the original stent remained embedded and was fractured during extraction. Some of the stent wires had to be removed under endoscopy.
The SIS technique under fluoroscopy has the following advantages over the gastroscopic removal technique: (I) it can be carried out under local anesthesia in conscious patients and so is suitable even for those in poor physical condition; (II) stent implantation and removal is quickly and accurately performed; and (III) the guide wire catheter has a smaller diameter than the gastroscope, and so it can easily be passed through narrow strictures that would not allow passage of a gastroscope. Meanwhile, a major advantage of the gastroscopic technique is that it allows direct visualization of the esophageal lumen and, when necessary, permits hemostasis under direct vision. However, gastroscopic stent removal needs general anesthesia, which may be risky in some patients. Further, passage of the gastroscope through severely narrowed segments can be difficult. The main limitation of this study is its small sample size and a retrospective single-center study. Methods to more rapidly reduce the granulation tissue and shorten the treatment cycle need to be identified. We are planning to conduct a clinical trial or animal experiment to further study the effectiveness of the technique and its mechanism.
Conclusions
The SIS technique under fluoroscopy appears to be a safe and effective method for the removal of esophageal metallic stent. The advantages and disadvantages of the SIS technique performed under fluoroscopy needs to be studied in greater detail in future research.
Acknowledgments
We are very grateful for the manuscript editing services provided by ELIXIGEN corporation.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-21-1039/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-21-1039/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of the First Affiliated Hospital of Zhengzhou University (No. 2017-C01) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yano T, Yoda Y, Nonaka S, Abe S, Kawata N, Yoshio T, Sasaki T, Tanaka S, Sasaki F, Maekita T, Kitano M, Matsumoto K, Isayama H, Ono H. Pivotal trial of a biodegradable stent for patients with refractory benign esophageal stricture. Esophagus 2022; Epub ahead of print. [Crossref] [PubMed]
- Conio M, Filiberti RA, Siersema PD, Manta R, Blanchi S, De Ceglie A. A new designed self-expandable metal stent for the management of benign radiotherapy-induced hypopharyngeal or cervical esophageal strictures. Surg Endosc 2022;36:2290-9. [Crossref] [PubMed]
- Grass JK, Küsters N, von Döhren FL, Melling N, Ghadban T, Rösch T, Simon M, Izbicki JR, König A, Reeh M. Management of Esophageal Cancer-Associated Respiratory-Digestive Tract Fistulas. Cancers (Basel) 2022;14:1220. [Crossref] [PubMed]
- Khara HS, Diehl DL, Gross SA. Esophageal stent fracture: case report and review of the literature. World J Gastroenterol 2014;20:2715-20. [Crossref] [PubMed]
- Talreja JP, Eloubeidi MA, Sauer BG, Al-Awabdy BS, Lopes T, Kahaleh M, Shami VM. Fully covered removable nitinol self-expandable metal stents (SEMS) in malignant strictures of the esophagus: a multicenter analysis. Surg Endosc 2012;26:1664-9. [Crossref] [PubMed]
- DaVee T, Irani S, Leggett CL, Berzosa Corella M, Grooteman KV, Wong Kee Song LM, Wallace MB, Kozarek RA, Baron TH. Stent-in-stent technique for removal of embedded partially covered self-expanding metal stents. Surg Endosc 2016;30:2332-41. [Crossref] [PubMed]
- Aiolfi A, Bona D, Ceriani C, Porro M, Bonavina L. Stent-in-stent, a safe and effective technique to remove fully embedded esophageal metal stents: case series and literature review. Endosc Int Open 2015;3:E296-9. [Crossref] [PubMed]
- Gornals JB, Golda T, Soriano A. Stent-in-stent technique for removal of a metal stent embedded in the colon wall by using a fully covered, self-expandable metal esophageal stent (with video). Gastrointest Endosc 2012;76:695-6. [Crossref] [PubMed]
- Xie PF, Liu Y, Qi Y, Li XN, Yin MP, Zhao Y, Li CX, Li Z, Wu G. Stent-in-stent technique for removal of the tracheal stent in patients with severe granulation tissue hyperplasia. Quant Imaging Med Surg 2021;11:4676-82. [Crossref] [PubMed]
- Odell JA, DeVault KR. Extended stent usage for persistent esophageal leak: should there be limits? Ann Thorac Surg 2010;90:1707-8. [Crossref] [PubMed]
- Kim PH, Song HY, Park JH, Zhou WZ, Na HK, Cho YC, Jun EJ, Kim JK, Kim GB. Fluoroscopic removal of retrievable self-expandable metal stents in patients with malignant oesophageal strictures: Experience with a non-endoscopic removal system. Eur Radiol 2017;27:1257-66. [Crossref] [PubMed]
- Ou Y, Chen L, Li J, Ye Y, Chen Z, Cai L, Liao J. Endoscopic removal of a migrated esophageal covered self-expandable metal stent: the nylon loop pusher-assisted method. Endoscopy 2022; Epub ahead of print. [Crossref] [PubMed]
- Chandnani M, Cohen J, Berzin TM. Combined Approach of Cryoablation and Stent-In-Stent Technique for Removal of an Embedded Esophageal Stent. Case Rep Gastrointest Med 2018;2018:8619252. [Crossref] [PubMed]
- Chandrasekar TS, Kalamegam RY, Janakan GB, Suriyanarayanan S, Menta PS, Chandrasekar VT. Double-step invagination technique-A novel approach to retrieve embedded esophageal self-expanding metal stent. Indian J Gastroenterol 2017;36:424-8. [Crossref] [PubMed]
- Hill C, Khalil BK, Barola S, Agnihotri A, Moran RA, Chen YI, Ngamruengphong S, Singh VK, Frame LA, Schweitzer MA, Magnuson TH, Khashab MA, Okolo PI 3rd, Kumbhari V. Inversion Technique for the Removal of Partially Covered Self-Expandable Metallic Stents. Obes Surg 2018;28:161-8. [Crossref] [PubMed]
- Eloubeidi MA, Lopes TL. Novel removable internally fully covered self-expanding metal esophageal stent: feasibility, technique of removal, and tissue response in humans. Am J Gastroenterol 2009;104:1374-81. [Crossref] [PubMed]
- Hirdes MM, Vleggaar FP, Van der Linde K, Willems M, Totté ER, Siersema PD. Esophageal perforation due to removal of partially covered self-expanding metal stents placed for a benign perforation or leak. Endoscopy 2011;43:156-9. [Crossref] [PubMed]
- Setoyma T, Miyamoto S, Horimatsu T, Morita S, Ezoe Y, Muto M, Watanabe G, Tanaka E, Chiba T. Multimodal endoscopic treatment for delayed severe esophageal stricture caused by incomplete stent removal. Dis Esophagus 2014;27:112-5. [Crossref] [PubMed]
- Liu XQ, Zhou M, Shi WX, Qi YY, Liu H, Li B, Xu HW. Successful endoscopic removal of three embedded esophageal self-expanding metal stents. World J Gastrointest Endosc 2017;9:494-8. [Crossref] [PubMed]
- Dua KS, Vleggaar FP, Santharam R, Siersema PD. Removable self-expanding plastic esophageal stent as a continuous, non-permanent dilator in treating refractory benign esophageal strictures: a prospective two-center study. Am J Gastroenterol 2008;103:2988-94. [Crossref] [PubMed]


