Axonotmesis of the femoral and sciatic nerves mimicking lumbar radiculopathy
We report a case describing an extraspinal cause of lumbosacral radiculopathy. The goal of this case report is to highlight the contributing role of magnetic resonance imaging (MRI) of peripheral nerves in radicular pain. Axonotmesis of the sciatic nerve could be considered as a post-traumatic piriformis syndrome.
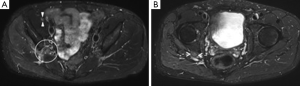
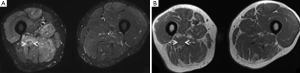
A 53-year-old man presented with a 5-month history of recalcitrant sciatic pain following an accidental fall in hip hyperabduction. The clinical examination revealed progressive difficulty walking, amyotrophy of the right thigh associated with severe weakness of the lower leg muscles and disappearance of ipsilateral Achilles reflex. Weakness of the quadriceps and absence of the patellar reflex indicated concomitant damage to the right femoral nerve. On electroneuromyography, the territory of the right femoral and sciatic nerves showed signs of severe subacute denervation. Pelvic MRI revealed involvement of the right femoral nerve with increased caliber, homogenous high T2-weighted signal intensity and a loss of its fascicular structure (Figure 1A, arrowheads). The right sciatic nerve from the infrapiriformis space (Figure 1A, white circle) showed the same pattern (Figure 1B, arrows), without loss of nerve continuity, until mid-thigh. Axial slices focused on the thigh revealed right muscle denervation with diffuse edema (Figure 2A) and fatty amyotrophy on T1-weighted images (Figure 2B). The diagnosis of post-traumatic nerve injury, called high-grade axonotmesis (1) of the right femoral and sciatic nerves, secondary to hip hyperabduction injury was retained and the lesion of the sciatic nerve could be considered as a post-traumatic piriformis syndrome (2).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Seddon H. Three types of nerve injury. Brain 1943;66:237-288.
- Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 1999;81:941-9. [PubMed]


