Comparison of three different embolic materials for varicocele embolization: retrospective study of tolerance, radiation and recurrence rate
Introduction
Varicocele is an abnormal dilatation of the veins in the pampiniform plexus that is caused by a reflux of blood in the internal spermatic vein. The incidence of varicocele in adolescent and young males is approximately 15-20%, and can be observed in up to 40-45% of infertile males (1,2). The etiology of varicocele is still debated and probably multifactorial. However, the most common cause is a congenital and/or acquired valve dysfunction responsible for reflux in the internal spermatic vein (3). The left side is affected in 80-90% of cases and the right side in only 5-10% of cases. It is bilateral in 1-15% of cases (3). Indications for treatment are as follows: pain or discomfort, recurrence or persistence after previous endovascular or surgical treatment and male infertility with reduced sperm quality (4). Treatment consists of preventing reflux through the internal spermatic vein and its branches superior to the pampiniform plexus. This can be achieved by surgical ligature or percutaneous endovascular embolization of the spermatic vein (5,6). Endovascular treatment has gained acceptance over the past two decades as an efficient alternative to surgery. Indeed, percutaneous embolization has the advantage of being an outpatient procedure with a faster return to normal activities, a considerably lower cost and a lower recurrence rate than is the case for surgery (6). The use of many different embolic agents, such as gelatin sponge, stainless steel coils, Amplatzer vascular plugs, detachable balloons, cyanoacrylate glues or sclerosing agents has been reported (7-15). However, to our knowledge, there are no data in the literature regarding the comparison of the different embolic materials currently available on the market for the treatment of varicocele in terms of efficacy, tolerance, radiation and recurrence rates. The goal of our study was to compare pain, radiation doses and recurrence rates in young male patients undergoing varicocele embolization with three different embolic materials: glue, mechanical devices and sclerosing agents.
Materials and methods
Study population
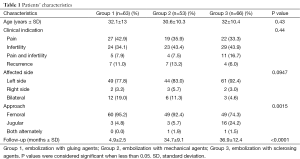
From July 2011 to May 2015, 204 young adult patients (mean age, 31.6±11.3 years) were referred to our radiology department for varicocele embolization. Patients younger than 18 years (n=5), patients with a normal phlebogram (n=9) and patients who could not be treated because of a technical failure were excluded (n=8). Finally, 182 patients, in whom 203 spermatic veins were found to be insufficient and hence treated by embolization, were included for the analysis. The diagnosis of varicocele and gonadal vein insufficiency were confirmed in all the patients by Doppler ultrasound and physical examination. The study population was retrospectively divided into three groups according to the embolic materials used for the endovascular treatment, whatever the phlebographic classification. The embolization procedure was performed using gluing agents (group 1, n=63), mechanical agents (group 2, n=53) or sclerosing agents (group 3, n=66).
The three study groups were comparable in terms of age, clinical indication and side of embolization. The clinical indications were impotence, pain and/or discomfort with or without infertility, and primary or secondary infertility. The varicoceles were classified according to an adapted version of the Dubin and Amelar classification as subclinical grade 1 (small), grade 2 (moderate), and grade 3 (large) (16). Symptomatic varicoceles were treated whatever the grade. Only grade 3 varicoceles were treated in patients with isolated infertility without symptoms. The jugular approach was more often used (P=0.0015) in group 3 than in groups 1 and 2. Characteristics of the three study populations are summarized in Table 1. Given that varicocele embolization was a common practice, the local ethics committee did not request additional consent.
Full table
Embolization techniques
All procedures were performed in an outpatient setting by two experienced interventional radiologists (R.L. and L.E., with 14 and 8 years of experience, respectively) using a Philips Allura Xper FD 20 angio room (Philips, Best, The Netherlands). After local anesthesia right transfemoral or transjugular selective venography of the renal veins and the internal spermatic veins were performed through a 6-Fr sheath using 5-Fr diagnostic catheters (Cobra-shaped and Vertebral catheter respectively for the femoral and jugular approach; Cook Europe, Bjaeverskov, Denmark). The studies were performed under the Valsalva maneuver with a maximum of 50 cc contrast agent (Visipaque 270 mgI/mL, GE Healthcare). Venous insufficiency was substantiated by retrograde opacification of the spermatic vein and of the pampiniform plexus, either spontaneously or after passing a competent valve. A 2.7-Fr microcatheter (Progreat®, Terumo Interventional Systems, Japan) was then positioned suprainguinal to perform superselective distal venography in the supine position. The paraspermatic veins, connecting collaterals or renospermatic bypasses to the internal spermatic vein, were mapped.
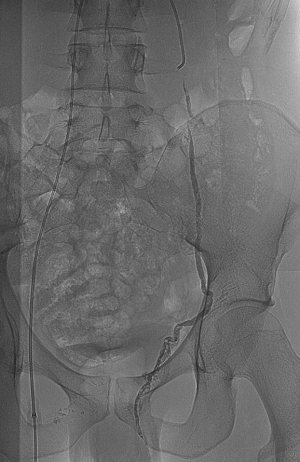
In group 1, the embolization procedure was performed using a gluing agent such as N-butyl 2-cyanoacrylate-methacryloxysulfolane (NBCA-MS) glue (Glubran®2, Viareggio, Italy) (range, 1-3 mL) mixted with Lipiodol (Lipiodol® Ultrafluid, Guerbet, Aulnay-sous-Bois, France) at a ratio of 1:1. The microcatheter dead space was filled with an anionic solution, dextrose 5%, to avoid intracatheter glue polymerization. The Lipiodol-glue mixture was injected under strict fluoroscopic control, with continuous manual injection and a display of real-time distribution. We began the glue injection in the distal intrapelvic segment of the gonadal vein, and withdrew the catheter while injecting the glue under fluoroscopy guidance. Injection was stopped before the pampiniform plexus was reached. The microcatheter was removed when the liquid embolic agent filled the venous space selected beforehand (Figure 1).
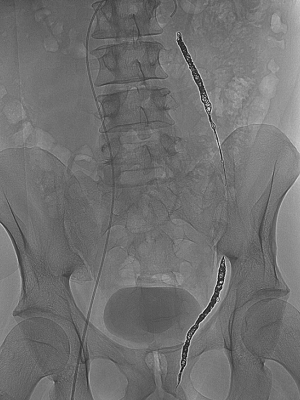
In group 2, the embolization procedure was performed using mechanical agents, such as detachable coils (Concerto®, Covidien, Irvine, CA, USA) or vascular plugs (Amplatzer®, St Jude Medical, Plymouth, MN, UK) of appropriate size, alone or in combination. The coils were first deployed through the microcatheter as distal as possible and up to the inguinal canal. Then, a sandwich occlusion of the spermatic vein was performed with additional coils in the proximal part of the spermatic vein (Figure 2). Plugs were usually deployed through a standard 5-Fr catheter or 6- or 7-Fr long sheath using the same sandwich technique (Figure 3). In some cases of large veins, both plugs and coils were used to ensure complete occlusion of the spermatic vein.
In group 3, the embolization procedure used a sclerosing agent, such as polidocanol 2% (Aetoxysclerol®, Kreussler Pharma, Paris, France) in combination with coils (Concerto®, Covidien, Irvine, CA, USA). In this sclerotherapy procedure, a syringe containing polidocanol at 2% (range, 2-8 mL) was mixed through a three-way stopcock with another syringe containing unfiltered room air (1:1 ratio) and 2 mL of contrast medium to create the sclerosing foam. The foam was then injected under fluoroscopic guidance through the catheter that was placed, in most cases, at the level of the sacroiliac joint. If there were origins of other collateral veins below the sacroiliac joint, the catheter was positioned at the level of these origins to allow the extensive sclerotherapy of all collaterals. During the polidocanol injection, the patient performed the Valsalva maneuver once again to prevent reflux of the sclerosing agent into the renal vein. To prevent the sclerosing foam from passing into the pampiniform plexus, which would lead to thrombophlebitis of the pampiniform plexus, coils were first placed at the level of the inguinal canal prior to sclerotherapy. Additional coils were then deployed according to the sandwich technique at the proximal part of the spermatic vein at the discretion of the interventional radiologist.
All of the patients were discharged after 2 hours of observation, and they returned to their normal daily activities after 24 hours. Piroxicam 20 mg twice daily was prescribed for 1 week. Patients were asked to avoid heavy physical activity for 7 days.
Sandwich embolization of the left internal spermatic vein with Amplatzer vascular plugs.
Evaluation of parameters
Tolerance
Patients were retrospectively asked by telephone interviews to evaluate pain during embolization and at 1, 7 and 30 days using a quantitative pain scale ranging from 0 to 10.
Radiation
Radiation exposure during the embolization procedure was assessed by the means of three dosimetric parameters: duration of scopy (min), kinetic energy released per unit mass (kerma, mGy) and dose area product (DAP, mGy·cm2).
Recurrence
All of the patients were scheduled for a clinical and ultrasound Doppler examination in our facility 2 months after the embolization. The intervention was considered clinically successful when the following conditions were met: the absence of reflux in the ultrasound Doppler exam and/or the absence of scrotum pain and heaviness depending on the initial indication. For the long-term follow-up, we used patients’ medical records and conducted telephone interviews with the patients themselves to request information concerning post-interventional visits to the referring urologist, varicocele recurrence or persistence and post-procedural varicocele repair. Recurrence was defined as varicocele which required a new endovascular or surgical repair. Mean and median follow-up times were 24.4 and 30.5 months, respectively [range, 2-53 months; standard deviation (SD), 17 months].
Statistical analysis
Categorial variables are presented as percentages and compared using the Chi2 or Fisher’s exact test. Continuous variables are described as means (with SDs) and medians (with ranges). They were compared using parametric tests (Student or ANOVA) if distribution was normal, and non-parametric tests (Wilcoxon or Kruskall-Wallis) if not. Statistical analyses were performed using SAS 9.3 software. All tests were two sided and P values were considered significant when less than than 0.05.
Results
Of the 182 patients who underwent technically successful varicocele embolization, no major complications were recorded. We encountered 7 (3.8%) minor peri-procedural complications: two cases of a self-limiting vein lesion that did not require treatment (one case of contrast agent extravasation and one case of vein spasm) and four cases of temporary minimal groin hematoma that resolved spontaneously. No non-target migration of embolic material was reported during the procedure. No pampiniform plexus phlebitis was diagnosed. There were no long-term complications, such as testes loss. Fertility data were not investigated.
Tolerance
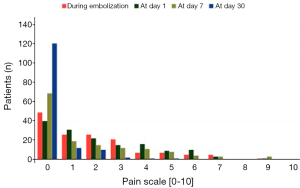
Data are based on the 147 (group 1 =53, group 2 =41, group 3 =53) of 182 patients who responded to the telephone interviews. Of the 147 patients interviewed, 66.7%, 72.8%, 53.1% and 17.7% reported pain or discomfort >0 during the procedure and at 1, 7 and 30 days, respectively. However, the mean pain or discomfort during the procedure, at 1, 7 and 30 days was always <2.5 on the quantitative pain scale with a range from 1 to 9, whatever the group. No difference in significant pain (pain score ≥3) during embolization and at 1, 7 and 30 days after treatment was noted between the three groups. Discomfort (pain score <3) was more frequent in group 1 (mean, 2.4±2.6) than in groups 2 (mean, 1.2±1.9) and 3 (mean, 1.6±2.2) at 7 days after the procedure (P=0.049). No difference in discomfort was noted during embolization and at 1 day and 30 days between the three groups. The distribution of pain scores during embolization and at 1, 7 and 30 days is shown in Figure 4.
Radiation
Data on duration of the scopy are based on the 156 (group 1 =60, group 2 =44, group 3 =52) of 182 patients in whom this parameter was available. Duration of scopy was significantly shorter (P<0.0001) in group 1 (mean time, 13±7.6 min) than in groups 2 (mean time, 21.4±9.1 min) and 3 (mean time, 19.1±10.1 min)
Data on kerma are based on the 142 (group 1 =48, group 2 =44, group 3 =50) of 182 patients in whom this parameter was available. Kerma was significantly lower (P=0.0087) in group 1 (mean, 304.3±310.9) than in groups 2 (mean, 504.6±481.3) and 3 (520.5±664.5).
Data on DAP are based on the 172 (group 1 =63, group 2 =47, group 3 =62) of 182 patients in whom this parameter was available. DAP was slightly but not significantly lower (P=0.1361) in group 1 (mean, 103,136±101,118) than in groups 2 (mean, 139,192±129,152) and 3 (mean, 143,423±191,267). Two-sided comparisons showed that DAP was lower in group 1 than in group 2 (P=0.04) but no difference was noted between groups 1 and 3, and groups 2 and 3. All of the data regarding dosimetric parameters are summarized in Table 2.
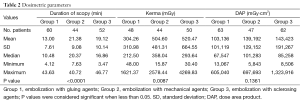
Full table
Recurrence
Data are based on the 147 (group 1 =53, group 2 =41, group 3 =53) of 182 patients who were followed by the referring urologist. At a mean overall follow-up of 24.4±17 months (range, 2-53 months), the recurrence rate was lower (P=0.032) in group 1 (n=0) than in groups 2 (n=7) and 3 (n=6). However, mean follow-up was shorter (P<0.0001) in group 1 (mean, 4.9±2.5 months) than in groups 2 (mean, 34.7±9.1 months) and 3 (mean, 36.9±12.4 months) (Table 1). The overall recurrence rate was 8.8% in interviewed patients.
Discussion
In this retrospective study, we evaluated differences in pain, radiation doses and recurrence rates in patients undergoing varicocele embolization with three different embolic materials: gluing agents (cyanoacrylate), mechanical agents (coils and/or plugs) or sclerosing agents (polidocanol). The use of cyanoacrylate glue for varicocele embolization was shown to be as safe as other embolic agents and led to less radiation (shorter duration of scopy, less kinetic energy released per unit mass, lower DAP) and a lower recurrence rate than was the case with other embolic materials. Moreover, the proportion of patients with significant pain, defined as a pain score ≥3, was similar in all three groups. As far as we are aware, this is the first report to compare different embolic materials for the percutaneous treatment of varicocele.
In the interventional radiology literature, technical and clinical success rates of 80-100% (9,12,13,15) in both sclerotherapy and embolization have been reported, which are consistent with our technical and clinical success rates of 100% and 91.2%, respectively. Among the endovascular methods, coils are the most commonly used because they are safe, easy to handle and readily available (8,17). Amplatzer vascular plugs may be used as an alternative to coils (18). The mechanism of action of coils and plugs is entirely occlusive and their effect is equivalent to surgical ligation of the main gonadal vein. One disadvantage of these mechanical embolic agents is that they are not as effective in the presence of collateral vessels, which may lead to recanalization of the varicocele. Furthermore, coil embolization has been shown to lead to complications such as coil migration, which may cause pulmonary embolism. Nowadays, this kind of complication is almost nil thanks to the development of detachable coils, which were used in our study. On the other hand, deployment of plugs may sometimes be challenging and requires large sheaths when the internal spermatic vein is large. Another frequently used endovascular option for varicocele treatment is pure sclerotherapy (12,14,15). Polidocanol injected as foam induces phlebitis with thrombosis and fibrosis of the vessel. This option is an effective but somewhat painful technique. The advantage of liquid substances over coils and plugs is that they produce a more extensive effect along the entire gonadal vein whereas coils or surgery cause a more focal obstruction of the vein. Liquids spread beyond the main gonadal vein through the collaterals, thus preventing possible recurrence. In the main study conducted in 141 patients with 146 varicoceles who underwent sclerotherapy with polidocanol 2%, the technical success rate was 91.8% (15). Follow-up revealed a clinical success rate of 83.9% and a persistence or relapse rate of 16.1%. The lowest relapse rate reported in the literature comes from the study by Jargiello et al., who used 3% aethoxysclerol with fibered coils (19). The highest relapse rates were reported in studies by Puche-Sanz et al. (8) and Wunsch et al. (20), who used fibered coils alone and aethoxysclerol alone in various concentrations, respectively. As suggested by some authors, a combination of sclerotherapy and embolization could provide better results (21). Kwak et al. described the so-called sandwich technique, which involves placing a nest of coils at the level of the inguinal canal prior to sclerotherapy (21). This would prevent reflux of the sclerosing agent into the plexus pampiniformis and, simultaneously, occlude the small collaterals that otherwise would not be embolized with coils alone. Additional coils are then placed in the upper part of the spermatic vein, as we usually did in our study.
In Europe, the main cyanoacrylate glues used for medical purposes today are NBCA (Histoacryl®) and NBCA-MS (Glubran®2), a copolymer of NBCA with a lower temperature of polymerization (10,22). The endothelium of the vessel is damaged as a result of the heat generated by the polymerization reaction of the glue. Cyanoacrylate has a dual mechanism of action. It is an embolic agent that causes mechanical obstruction and thrombosis, and it acts as a sclerosing agent, triggering chemical phlebitis, which subsequently induces fibrosis and complete destruction of the gonadal vein in a manner analogous to polidocanol (23). Few series have reported the use of glue as the only embolic agent in such a setting (9,10). Urbano et al. reported technical and clinical success rates of 100% in a series of 41 patients treated with Glubran®2 for varicocele (9). Vanlangenhove et al. demonstrated in a prospective, randomized, blinded comparative study that Histoacryl® and Glubran®2 were equally efficient and safe for the embolization of varicoceles (10).
However, Glubran®2 has many advantages over classical cyanoacrylate glues such as Histoacryl®. First, with Glubran®2 the polymerization reaction is slower, thus making handling and release easier. Second, NBCA is combined with another monomer, metacryloxysulfolane, to produce a more pliable and stable polymer whose milder exothermic reaction (45 °C) results in less inflammation and histotoxicity than is the case with Histoacryl® (22). It is therefore less painful at the time of injection, even though the assumed lower inflammatory reaction with NBCA-MS did not translate into improved tolerance in the only prospective study to compare varicocele embolization with either Histoacryl® (n=54) or Glubran®2 (n=58) (10). Discomfort after glue embolization of varicocele is a common side effect, which might evolve to pain. Some authors suggested that the occurrence of post-embolization pain seemed to be more frequent when cyanoacrylate and sclerosing agents rather than coils were used (14,15,24). However, we demonstrated in our study that the mean pain or discomfort during the procedure and at 1, 7 and 30 days was always <2.5 on the quantitative pain scale, whatever the embolic materials used. No difference in significant pain (pain score ≥3) during embolization and at 1, 7 and 30 days after treatment was noted between the three different embolic agents. Discomfort (pain score <3) at 7 days after the procedure was, however, more frequent with glue, though this was well managed with symptomatic treatment. No difference in discomfort was noted during embolization and at 1 and 30 days between the three different materials. Another advantage of Glubran®2 is the CE marking (25). Indeed, Histoacryl® is theoretically not allowed for endovascular purposes because of the absence of CE marking. Its use is considered off-label in this setting.
One technical aspect is that cyanoacrylate should be mixed with Lipiodol and released under fluoroscopic control. The mixture with Lipiodol also modulates the polymerization rate. In all of our patients, we used a glue-Lipiodol ratio of 1:1, thus achieving rapid polymerization, which avoids migration into the renal vein. We always started injecting the glue very low down to avoid potential revascularization from branches of the saphenous vein, while avoiding reflux into the pampiniform plexus at the same time. Cyanoacrylate is more viscous than polidocanol foam and polymerizes quickly. The possibility of significant reflux and massive diffusion through the collaterals is therefore unlikely.
Glue embolic agents present some drawbacks. Possible complications of cyanoacrylate varicocele embolization are glue migration into the pulmonary circulation, a glued catheter and severe phlebitis of the gonadal vein or pampiniform plexus (26-28). We had no complications in our series because the glue embolization was performed by radiologists with considerable experience in the use of tissue adhesives.
Lastly, embolization with Glubran®2 is very fast. On average, the glue injection takes less than 15 seconds, thus leading to low radiation in comparison with other embolic techniques, as demonstrated in our study (29). Furthermore, embolization with Glubran®2 is cost-effective. One cc is 3 times cheaper than any detachable coil or plug (30).
Our study had several limitations. First, this was a retrospective review of a cohort from a single center, with some patients lost of follow-up. Second, one goal of our study was to evaluate tolerance to embolization of the spermatic vein with different embolic materials during the procedure and at 1, 7 and 30 days. Almost half of the patients in each group had symptomatic varicocele. After embolization, it usually takes a few weeks for the pain to disappear completely. Consequently, it is difficult to know whether pain reported at 30 days in some patients was related to the procedure or just due to normal recovery in symptomatic patients treated with embolization. Third, the results of our study must be interpreted with caution. Indeed, although we attempted to compare gluing, mechanical and sclerosing agents with each other for varicocele embolization, polidocanol was not used alone in the sclerotherapy group but in combination with coils. This could have led to longer procedure times and higher radiation during the procedure in comparison with sclerotherapy alone. Fourth, the fact that recurrence rate of varicocele, which required a new treatment, was significantly lower in group 1 than in the two other groups may have been due to two factors. The mean follow-up in this group was significantly shorter than in groups 2 and 3. Indeed, in our daily practice, glue has come into use more recently in this setting and is now the only embolic agent used for varicocele treatment. Furthermore, no systematic ultrasound imaging follow-up was performed beyond 2 months following the procedure, which could have led to potential lower detection rate of long-term varicocele recurrence. Lastly, infertility was the clinical indication for treatment in a large proportion of our patients. In this setting, varicocele was often asymptomatic and recurrence after embolization could not be determined without ultrasound imaging. The results of our study must be validated in future prospective randomized controlled studies with longer follow-up times to determine whether the embolic material can affect outcome.
Conclusions
In conclusion, the use of Glubran®2 acrylic glue as an embolic agent for percutaneous embolization of varicocele is a therapeutic alternative that is effective, safe, inexpensive, and easily feasible in an outpatient setting, and has a high technical success rate. Glubran®2 triggers a local inflammatory reaction that promotes sclerosis and thrombosis, but without causing more significant pain than is the case with other embolic agents. The liquid nature of the embolization product allows diffusion through the gonadal vein and its collaterals, which appears to reduce recurrence rates and improve results. Lastly, the use of glue allows fast procedures, leading to less radiation than treatment with mechanical or sclerosing agents.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Belloli G, D'Agostino S, Pesce C, Fantuz E. Varicocele in childhood and adolescence and other testicular anomalies: an epidemiological study. Pediatr Med Chir 1993;15:159-62. [PubMed]
- Jarow JP, Coburn M, Sigman M. Incidence of varicoceles in men with primary and secondary infertility. Urology 1996;47:73-6. [PubMed]
- Mali WP, Oei HY, Arndt JW, Kremer J, Coolsaet BL, Schuur K. Hemodynamics of the varicocele. Part II. Correlation among the results of renocaval pressure measurements, varicocele scintigraphy and phlebography. J Urol 1986;135:489-93. [PubMed]
- Barbalias GA, Liatsikos EN, Nikiforidis G, Siablis D. Treatment of varicocele for male infertility: a comparative study evaluating currently used approaches. Eur Urol 1998;34:393-8. [PubMed]
- Cockett AT, Takihara H, Cosentino MJ. The varicocele. Fertil Steril 1984;41:5-11. [PubMed]
- Dewire DM, Thomas AJ Jr, Falk RM, Geisinger MA, Lammert GK. Clinical outcome and cost comparison of percutaneous embolization and surgical ligation of varicocele. J Androl 1994;15 Suppl:38S-42S. [PubMed]
- Hawkins CM, Racadio JM, McKinney DN, Racadio JM, Vu DN. Varicocele retrograde embolization with boiling contrast medium and gelatin sponges in adolescent subjects: a clinically effective therapeutic alternative. J Vasc Interv Radiol 2012;23:206-10. [PubMed]
- Puche-Sanz I, Flores-Martín JF, Vázquez-Alonso F, Pardo-Moreno PL, Cózar-Olmo JM. Primary treatment of painful varicocoele through percutaneous retrograde embolization with fibred coils. Andrology 2014;2:716-20. [PubMed]
- Urbano J, Cabrera M, Alonso-Burgos A. Sclerosis and varicocele embolization with N-butyl cyanoacrylate: experience in 41 patients. Acta Radiol 2014;55:179-85. [PubMed]
- Vanlangenhove P, De Keukeleire K, Everaert K, Van Maele G, Defreyne L. Efficacy and safety of two different n-butyl-2-cyanoacrylates for the embolization of varicoceles: a prospective, randomized, blinded study. Cardiovasc Intervent Radiol 2012;35:598-606. [PubMed]
- Sze DY, Kao JS, Frisoli JK, McCallum SW, Kennedy WA 2nd, Razavi MK. Persistent and recurrent postsurgical varicoceles: venographic anatomy and treatment with N-butyl cyanoacrylate embolization. J Vasc Interv Radiol 2008;19:539-45. [PubMed]
- Carmignani L, Casellato S, Galasso G, Bozzini G, Spinelli M, Dell'Agnola CA, Rocco F. Sclerotherapy of the pampiniform plexus with modified Marmar technique in children and adolescents. Urol Int 2009;82:187-90. [PubMed]
- Seyferth W, Jecht E, Zeitler E. Percutaneous sclerotherapy of varicocele. Radiology 1981;139:335-40. [PubMed]
- Riedl P, Kumpan W, Maier U, Stackl W, Lunglmayr G. Long-term results after sclerotherapy of the spermatic vein in patients with varicocele. Cardiovasc Intervent Radiol 1985;8:46-9. [PubMed]
- Ali A, Wirth S, Treitl KM, Treitl M. Treatment of male varicoceles by transcatheter polidocanol foam sclerotherapy: evaluation of clinical success, complications, and patients' satisfaction with regard to alternative techniques. Eur Radiol 2015;25:2889-97. [PubMed]
- Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril 1970;21:606-9. [PubMed]
- Kuroiwa T, Hasuo K, Yasumori K, Mizushima A, Yoshida K, Hirakata R, Komatsu K, Yamaguchi A, Masuda K. Transcatheter embolization of testicular vein for varicocele testis. Acta Radiol 1991;32:311-4. [PubMed]
- Cil B, Peynircioğlu B, Canyiğit M, Geyik S, Ciftçi T. Peripheral vascular applications of the Amplatzer vascular plug. Diagn Interv Radiol 2008;14:35-9. [PubMed]
- Jargiello T, Drelich-Zbroja A, Falkowski A, Sojka M, Pyra K, Szczerbo-Trojanowska M. Endovascular transcatheter embolization of recurrent postsurgical varicocele: anatomic reasons for surgical failure. Acta Radiol 2015;56:63-9. [PubMed]
- Wunsch R, Efinger K. The interventional therapy of varicoceles amongst children, adolescents and young men. Eur J Radiol 2005;53:46-56. [PubMed]
- Kwak N, Siegel D. Imaging and interventional therapy for varicoceles. Curr Urol Rep 2014;15:399. [PubMed]
- Loffroy R, Guiu B, Cercueil JP, Krausé D. Endovascular therapeutic embolisation: an overview of occluding agents and their effects on embolised tissues. Curr Vasc Pharmacol 2009;7:250-63. [PubMed]
- Heye S, Maleux G, Wilms G. Pain experience during internal spermatic vein embolization for varicocele: comparison of two cyanoacrylate glues. Eur Radiol 2006;16:132-6. [PubMed]
- Vanlangenhove P, Everaert K, Van Maele G, Defreyne L. Tolerance of glue embolization under local anesthesia in varicoceles: a comparative study of two different cyanoacrylates. Eur J Radiol 2014;83:559-63. [PubMed]
- Levrier O, Mekkaoui C, Rolland PH, Murphy K, Cabrol P, Moulin G, Bartoli JM, Raybaud C. Efficacy and low vascular toxicity of embolization with radical versus anionic polymerization of n-butyl-2-cyanoacrylate (NBCA). An experimental study in the swine. J Neuroradiol 2003;30:95-102. [PubMed]
- Kolilekas L, Kalomenidis I, Manali E, Triantafillidou C, Brountzos E, Papiris S. Cyanoacrylate-related pulmonary embolism following percutaneous varicocele embolization. South Med J 2008;101:1073-4. [PubMed]
- Vinters HV, Galil KA, Lundie MJ, Kaufmann JC. The histotoxicity of cyanoacrylates. A selective review. Neuroradiology 1985;27:279-91. [PubMed]
- Montanaro L, Arciola CR, Cenni E, Ciapetti G, Savioli F, Filippini F, Barsanti LA. Cytotoxicity, blood compatibility and antimicrobial activity of two cyanoacrylate glues for surgical use. Biomaterials 2001;22:59-66. [PubMed]
- Verstandig AG, Shamieh B, Shraibman V, Raveh D. Radiation dose reduction in fluoroscopic procedures: left varicocele embolization as a model. Eur Radiol 2015;25:1639-45. [PubMed]
- Iaccarino V, Venetucci P. Interventional radiology of male varicocele: current status. Cardiovasc Intervent Radiol 2012;35:1263-80. [PubMed]