Prenatal ultrasound diagnosis of 1 case of vesicoureteral reflux
Introduction
Vesicoureteral reflux (VUR) is a backward flow of urine from the urinary bladder to the kidneys. It is important to detect VUR as early as possible in order to decrease renal damage and associated complication, e.g., by urinary tract infection (1,2). However, usually renal damage has already occurred after the patients are diagnosed (3). We hoped to obtain characteristics of ultrasound sonography of prenatal VUR in order to give clue to diagnosis of potential renal damage. Here we reported a case that prenatal diagnosis showed VUR and was further confirmed by postnatal follow-up ultrasound and micturating cystourethrogram (MCUG).
Case presentation
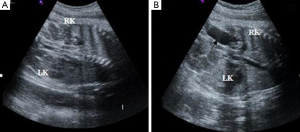
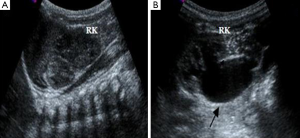
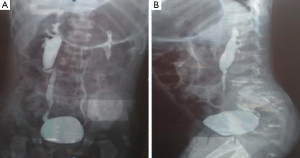
This case was from a 22-year-old pregnant woman in our department and keep in observation as long as 3 years. According to our ultrasound examination one day before the birth, the right kidney of the fetus showed mild hydronephrosis and the size of the renal pelvis was 0.6 cm, while the left kidney did not show obvious abnormality. The right kidney was smaller than the left one and corticomedullary differentiation was absent. It had been observed several times that the right ureter dilated and the maximum size was about 2.0 cm in inner diameter (Figure 1). One day after the birth, both longitudinal and transverse images of the kidney were obtained by urinary ultrasound examination. When the baby was crying or micturating, the ureter dilated to about 2.0 cm in inner diameter (Figure 2). At the same time, we observed that the bladder capacity was shrinking. MCUG was performed on the baby at one year old. A grade IV VUR on the right side was demonstrated (Figure 3). The VUR was still observed when he was 3 years old. The size of the right kidney was 5.4 cm × 2.3 cm but the size of the left kidney was 8.2 cm × 3.4 cm. Although we have done frequent ultrasound monitoring and the boy did not get urinary tract infection, his right kidney has been growing slowly.
Discussion
VUR is mainly caused by a failure of the ureterovesical valve mechanism. According to the international VCUG grading criteria, VUR is divided into five grades (4). Mild VUR does not cause kidney damage. The study by Kamil has suggested that 80% of patients with primary VUR do not require surgical treatment (5). Severe VUR is a risk factor for progressive kidney damage in the event of urinary tract infection, so only severe VUR is clinically significant (6).
In general, VUR may not show any clinical symptoms and lead to any specific signs, unless combined with urinary tract infection. Thus, asymptomatic VUR may lead to long-term effects on the kidneys. In our case, after we observed the grade IV VUR prenatally, follow-up examinations on VUR and urinary tract infection were performed frequently after the birth. It indicates that prenatal ultrasound diagnosis of severe VUR can provide clues for the prevention or treatment of damage to the kidneys after birth as early as possible.
Antenatal hydronephrosis is a sign of VUR, but about 50% of fetus has antenatal hydronephrosis in prenatal examination (7). Although in most cases hydronephrosis is physiological, it is still possibly linked to urinary tract abnormalities. In case of mild reflux, the ureter may have momentary dilatation that disappears quickly, which is often overlooked and considered as an intestinal canal in scanning. In this case, we did not observe obvious VUR in the left kidney prenatally, but MCUG demonstrated a mild VUR. It was due to the prenatal ultrasound examination is less capable to tell the difference between mildly dilated ureter and intestinal canal. When hydronephrosis is detected in prenatal examination, it may not be diagnosed as normal especially in the presence of a smaller kidney. A further ultrasound examination should be repeatedly applied to observe the transverse and longitudinal sections of the kidney to exclude the possibility of VUR.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- de Jong TP, van Gool JD, Van Wijk AA, Stoutenbeek P, Van Isselt HW. Antenatally diagnosed obstructive uropathy--kidney imaging vs kidney function. Acta Urol Belg 1989;57:413-6. [PubMed]
- Thomas DF. Prenatal diagnosis: does it alter outcome? Prenat Diagn 2001;21:1004-11. [Crossref] [PubMed]
- Nakai H, Kakizaki H, Konda R, Hayashi Y, Hosokawa S, Kawaguchi S, Matsuoka H, Nonomura K, Shimada K, Kawamura T; Prospective Study Committee of Reflux Nephropathy Forum, Japan. Clinical characteristics of primary vesicoureteral reflux in infants: multicenter retrospective study in Japan. J Urol 2003;169:309-12. [Crossref] [PubMed]
- Kaefer M, Curran M, Treves ST, Bauer S, Hendren WH, Peters CA, Atala A, Diamond D, Retik A. Sibling vesicoureteral reflux in multiple gestation births. Pediatrics 2000;105:800-4. [Crossref] [PubMed]
- Kamil ES. Recent advances in the understanding and management of primary vesicoureteral reflux and reflux nephropathy. Curr Opin Nephrol Hypertens 2000;9:139-42. [Crossref] [PubMed]
- Parvex P, Willi JP, Kossovsky MP, Girardin E. Longitudinal analyses of renal lesions due to acute pyelonephritis in children and their impact on renal growth. J Urol 2008;180:2602-6; discussion 2606. [Crossref] [PubMed]
- Roth JA, Diamond DA. Prenatal hydronephrosis. Curr Opin Pediatr 2001;13:138-41. [Crossref] [PubMed]


