Contrast enhanced ultrasound demonstration of a proliferative mass in rectum wall in a patient after rectal cancer surgery
A 53-year-old man was admitted to hospital manifested with bloody stool for a month without other symptoms. Colonoscopy found a cauliflower-like mass in anterior rectal wall. The distance of the tumor lower margin from the anal verge was 5 cm. Biopsy pathology results showed adenocarcinoma. Pre-operative chest radiographs and abdominal ultrasound did not show evidence of metastasis. The patient underwent laparotomy Dixon operation. Postoperative pathologic diagnosis was moderately differentiated adenocarcinoma invading the muscle layer with no lymph node metastasis. 12 days after the operation, the patient had rectal bleeding and hemorrhagic shock. He underwent emergency trans-anal exploration immediately and it was found that there was a hemorrhagic foci covered with dried blood on the posterior rectal wall 1-2 cm below the anastomosis, which was intact, and no active bleeding was observed at the time. Gauze was then inserted into the rectum for compression hemostasis. The patient recovered well and no reoccurrence of hemorrhage occurred.
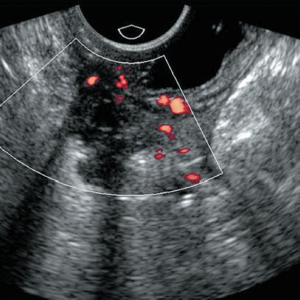
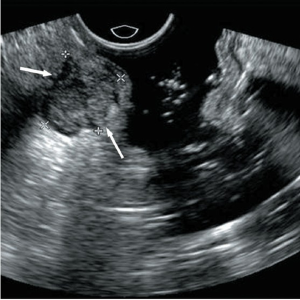
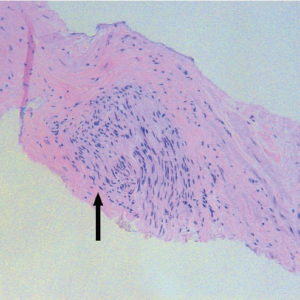
Twenty-three months later, a contrast enhanced pelvic CT scan in a scheduled follow-up visit detected a 1.5 cm × 2.1 cm intraluminal low density non-enhancing mass in the right lateral wall of the rectum in peri-anastomotic area, suspicious for local recurrence(Figure 1). The patient then underwent endorectal ultrasonography (ERUS) examination. The ultrasound machine used was Philips iU22 unit (Philips, Bothell, WA, USA). An end-fire type endorectal probe (C5-9 sec) was utilized. ERUS found an intramural mass located in the right lateral wall of the rectum in the peri-anastomotic area (Figure 2). The mass was hypoechoic, inhomogeneous, and lobulated with clear margin. Both the color and power doppler sonography showed no blood flow (Figure 3). The mass was mainly confined to the muscular layer with intact mucosal and submucosal layers. Contrast enhanced ERUS was then performed with 2.4 mL contrast agent administrated through a forearm vein (MI 0.08-0.11, Sonovue, Bracco). Approximately 11 seconds after injection, the bowel wall enhanced, achieving the maximum enhancement at approximately 20 seconds. The mass was not enhanced throughout 40 seconds of recording while the bowel wall continued enhancement (Video 1). The mass was considered to be a benign post-operative alteration, based on characteristics of the margin and interface, and lack of blood flow and enhancement of the mass, as well as the history of gauze compression for rectal mucosal hemorrhage. Trans-rectal EUS-guided biopsy of the mass was performed subsequently and the pathologic result demonstrated proliferation of fibrous tissue and neural tissue, which confirmed our previous diagnosis (Figure 4).

CT and MRI is effective in the detection of local recurrence of rectal cancer, but is limited in distinguishing lesions from artifacts caused by metal clips, post-operative scarring or stool, granulation tissue and inflammation. Contrast enhanced ERUS is not interfered by the artifacts, and capable of distinguishing the five layers of the bowel wall and providing an accurate depiction of the tumor vascularization. The usefulness of ERUS in postoperative evaluations of rectal cancer has been confirmed in a number of retrospective and prospective studies but contrast enhanced ERUS has not been reported in literatures. This case indicates the advantage of ERUS in differentiation of a postoperative tissue proliferation from local recurrence.
Acknowledgements
Disclosure: The authors declare no conflict of interest.