Bedside ultrasonography for diagnosis of pneumothorax
Introduction
Pneumothorax (PTX) is an emergency that requires urgent management to avoid catastrophic consequences. PTX is also an important cause of respiratory failure in the emergency department and an annual rate of PTX is estimated at 22.7 cases for 100,000 population (1). Timely and accurate confirmation or exclusion of PTX is of paramount importance in emergency and critical care settings. The plain chest X-ray (CXR) is a traditional method for the evaluation of PTX. However, CXR is shown to have low sensitivity in detecting intrapleural air in trauma patients especially in supine position (2,3). Although computed tomography (CT) is the gold standard diagnostic test for the PTX, it is well limited by its high exposure to radiation and sometimes it is unsafe to transport these unstable patients. Chest ultrasonography (US) has found its way into the emergency and critical care setting for more than three decades and it is now gaining momentum in the evaluation of acute respiratory emergencies including but not limited to PTX. Diagnosis of PTX with US was first reported in 1986 by Rantanen (4). Recently numerous clinical studies have shown that PTX can be diagnosed by US with high sensitivity and specificity (5-8).
Normal findings in chest US
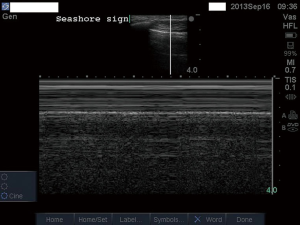
The pleural line is the basic structure that should be identified in the image of chest US. The so-called lung sliding identified at pleural line of the normal lung shows a cyclic movement between the visceral and parietal pleura with spontaneous respiration (Figure 1). It is the basic sign we need to identify when performing chest US. When lung sliding is observed, PTX can be ruled out. Since the structure above the pleural line is static during respiration, it produces parallel lines that look like waves in M-mode (e.g., the horizontal line represents time and static structure produces parallel lines). Beneath the pleural line, the cyclic movement of lung with respiration produces sand-like appearance. Pioneers in chest US termed this a “seashore sign” that represents the normal findings in chest US (Figure 2).

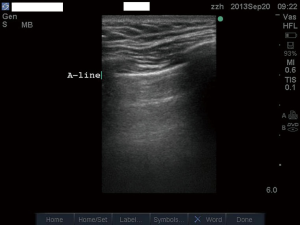
Besides the lung sliding, the most common artefacts in lung ultrasound are A-line (Figure 3) and B-line (Figure 4). The A-line artefact is horizontal artifactual repetitions of the pleura line. A-lines are often presented in normal lung, indicating that the lung is well aerated. Otherwise, A-line can also be found in PTX when lung sliding is absent.
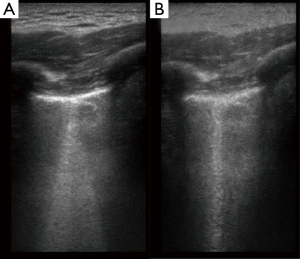
B-line is the vertical line that is perpendicular to the pleural line and its appearance represents fluid accumulation in the alveoli. The B-line is also known as comet-tail artefact which is formed by repetitive reflections of the ultrasound wave arising from the pleural line. B-line is characteristic of long and laser-like appearance that never fades at the distal image. B-line can be typically found in interstitial syndrome and occasionally in dependent regions of normal lung. Because PTX can be ruled out by the presence of B-line, it is discussed in this section. There is a trick in identification of B-line in modern bedside ultrasound machines. Most modern machines have the “multi-beam” (MB) function, which presents the ability of a probe to get rid of all sorts of angled ‘beams’ of sound across the field to try to get around echoic interfaces and other obstacles that might interfere with the distal image. This MB function helps the probe getting rid of artefacts from echoic objects in the near field. However, it is not desirable to get rid of artefacts in near field because in chest US the B-line is just the artefact that we want in the near field. Therefore the MB function should be switched off when the purpose is to identify B-line (Figure 4B). If MB is on, the B-line appears to be multiple lines emitting from a single point (Figure 4A).
Diagnosis of PTX
PTX is typically confirmed by the presence of the following ultrasonographic findings: a stratosphere sign, abolished lung sliding or lung pulsing, the absence of B lines, and the presence of lung point. Lung point can be found at the boundary where normal lung sliding and PTX coexist, and it is a specific sign of PTX (see more descriptions and videos below). Pathophysiologically, PTX is the detachment of visceral and parietal pleura by entrapped air in the pleural space. All ultrasonographic signs should be comprehended with the understanding of this pathological process of PTX.
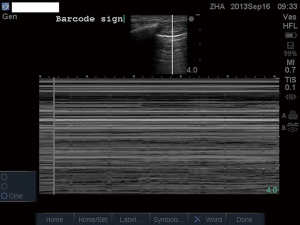
A hallmark sign that can be found in PTX is the stratosphere sign (Figure 5). In the pleural line the lung sliding is abolished and the sand-like appearance beneath the pleural line is replaced by parallel lines which is termed stratosphere or barcode sign. However, this finding can also be identified in conditions in which there is no relative movement between visceral and parietal pleura, such as apnea and pleuritis. PTX abolishes B-line, which is very sensitive that the presence of B-line can help to rule out PTX in scanned regions. Lung sliding has the same value in determining PTX that PTX can be 100% ruled out by the presence of lung sliding (10). In conditions with less movement between visceral and parietal pleura, lung pulse can be employed to rule out PTX. Lung pulse is produced by transmission of cardiac pulse to pleural line, given that the visceral and parietal pleura contact with each other (Figure 6). Volpicelli et al. gives important value to the lung pulse sign by stating that “even in the absence of lung sliding and B lines, visualization of a lung pulse rules out pneumothorax” (12). This is important because in clinical emergency, the ruling out of PTX can immediately direct clinicians to other culprits of a drop in oxygenation or respiratory distress. One useful method to determine PTX is to examine the contralateral side of suspected lung region. Figure 7 shows healthy lung with evident lung sliding, while Figure 8 shows the absence of lung sliding and pulsing, replaced by multiple A-lines. These two video clips were obtained from both lungs of the same patient in the third intercostal space at mid-clavicular line.

Lung point is thought to be a 100% specific sign for PTX, though the sensitivity is less satisfactory by the fact that lung-point cannot be found in every patient with PTX (15). Typically, lung-point is identified at the junction where visceral and parietal pleura contact with each other (Figure 9). In B-mode ultrasound, the stratosphere and seashore patterns alternate with each other. However, there is a tricky sign that may confuse beginners in determining the presence of lung point. In our previous work we identified this sign for the first time but it is thought to be universe in normal lung. We termed it the physiological lung point (17). This sign distinguished from the true lung point in that there is no barcode sign in the abnormal region. Instead, the cardiac pulse can be identified in this region. We proposed that physiological lung point could be identified at the junction of lung pleura and mediastinal soft tissue. “Pseudo-lung point” is another sign that should be distinguished from true lung point. The sign can be found in lung contusions, and again there is no stratosphere pattern (18).
After confirmation of the presence of PTX, the next important issue is to quantification of the volume of PTX. The latter is important in that it may determine whether conservative or surgical procedure needs to be instituted. Volpicelli et al. found that the location of lung point can reliably classify PTX size as compared to CXR (19). In animal models of PTX, Oveland et al. demonstrated that chest US can accurately assess the progression of PTX during mechanical ventilation (20). In a case study reported by our group, we identified a double lung point sign in an infant and the PTX was further confirmed by chest CT scan (21). The PTX can be managed with conservative method. To the best of our knowledge, there are three cases of double lung point having been reported and one common feature of them is that all of the patients were managed by conservative method due to small size of PTX (22-24). As a result, we propose that the identification of PTX with double lung point indicate limited volume of PTX. If the patient presents severe respiratory compromise, other potential causes should be thoroughly sought for.
Diagnostic accuracy of chest US
Due to its wide availability in emergency and critical care setting, US has been investigated in numerous studies for its diagnostic accuracy in the determination of PTX (25-31). Recently, two independent study groups conducted systematic reviews of these articles (32,33). Ebrahimi et al.’s study included 28 studies and showed that the pooled sensitivity and specificity of chest US were 0.87 (95% CI: 0.81-0.92) and 0.99 (95% CI: 0.98-0.99), respectively (33). Additionally, they performed meta-regression and the result showed that the diagnostic accuracy of US in diagnosing PTX performed by the emergency physician was higher than by non-emergency physician. Higher pooled sensitivity (0.90; 95% CI: 0.83-0.98) was found in non-trauma setting, but lower specificity (0.97; 95% CI: 0.95-0.99) was reported in non-trauma setting. Alrajab et al.’s study included only 13 original research articles, probably due to more strict selection criteria (32). Their study showed that US had a pooled sensitivity of 78.6% (95% CI: 68.1-98.1) and a specificity of 98.4% (95% CI: 97.3-99.5). They also performed meta-regression and subgroup analyses to investigate heterogeneity, which indicated that consecutive sampling of patients provided higher sensitivity results than convenience sampling.
Conclusions
US represents a novel approach for the evaluation of PTX, with advantages of timeliness, high accuracy and high reliability. The US skills should be incorporated into the standard training programs of physicians working at emergency and critical care settings. Because lung ultrasound is relatively new, there are many areas of active research. For example, new signs continue to be reported and defined. The technique to quantification of PTX size is still under investigation. Furthermore, the diagnosis of PTX under special conditions such as mechanical ventilation and patients with large pulmonary bullae are being reported (34). Atypical signs such as “physiological lung point” and “pseudo-lung point” should be noted and carefully distinguished from true lung point.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bobbio A, Dechartres A, Bouam S, Damotte D, Rabbat A, Régnard JF, Roche N, Alifano M. Epidemiology of spontaneous pneumothorax: gender-related differences. Thorax 2015;70:653-8. [PubMed]
- Abdulrahman Y, Musthafa S, Hakim SY, Nabir S, Qanbar A, Mahmood I, Siddiqui T, Hussein WA, Ali HH, Afifi I, El-Menyar A, Al-Thani H. Utility of extended FAST in blunt chest trauma: is it the time to be used in the ATLS algorithm? World J Surg 2015;39:172-8. [PubMed]
- Soult MC, Weireter LJ, Britt RC, Collins JN, Novosel TJ, Reed SF, Britt LD. Can routine trauma bay chest x-ray be bypassed with an extended focused assessment with sonography for trauma examination? Am Surg 2015;81:336-40. [PubMed]
- Rantanen NW. Diseases of the thorax. Vet Clin North Am Equine Pract 1986;2:49-66. [PubMed]
- Ianniello S, Di Giacomo V, Sessa B, Miele V. First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med 2014;119:674-80. [PubMed]
- Jalli R, Sefidbakht S, Jafari SH. Value of ultrasound in diagnosis of pneumothorax: a prospective study. Emerg Radiol 2013;20:131-4. [PubMed]
- Ojaghi Haghighi SH, Adimi I, Shams Vahdati S, Sarkhoshi Khiavi R. Ultrasonographic diagnosis of suspected hemopneumothorax in trauma patients. Trauma Mon 2014;19:e17498. [PubMed]
- Shostak E, Brylka D, Krepp J, Pua B, Sanders A. Bedside sonography for detection of postprocedure pneumothorax. J Ultrasound Med 2013;32:1003-9. [PubMed]
- Chen L, Zhang Z. Basic structures of lung ultrasound. Asvide 2015;2:079. Available online: http://www.asvide.com/articles/672
- Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest 1995;108:1345-8. [PubMed]
- Chen L, Zhang Z. The presence of lung pulse to exclude pneumothorax. Asvide 2015;2:080. Available online: http://www.asvide.com/articles/673
- Volpicelli G, Boero E, Stefanone V, Storti E. Unusual new signs of pneumothorax at lung ultrasound. Crit Ultrasound J 2013;5:10. [PubMed]
- Chen L, Zhang Z. Lung sliding is present in healthy lung (obtained from left chest in the third intercostal space at mid-clavicular line). Asvide 2015;2:081. Available online: http://www.asvide.com/articles/674
- Chen L, Zhang Z. The clip shows the absence of lung sliding and pulsing, replaced by multiple A-lines (obtained from right chest in the third intercostal space at mid-clavicular line). Asvide 2015;2:082. Available online: http://www.asvide.com/articles/675
- Lichtenstein D, Mezière G, Biderman P, Gepner A. The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med 2000;26:1434-40. [PubMed]
- Chen L, Zhang Z. Lung point identified at the junction where visceral and parietal pleura contact with each other. Asvide 2015;2:083. Available online: http://www.asvide.com/articles/676
- Zhang Z, Chen L. A physiological sign that mimics lung point in critical care ultrasonography. Crit Care 2015;19:155. [PubMed]
- Gillman LM, Alkadi A, Kirkpatrick AW. The "pseudo-lung point" sign: all focal respiratory coupled alternating pleural patterns are not diagnostic of a pneumothorax. J Trauma 2009;67:672-3. [PubMed]
- Volpicelli G, Boero E, Sverzellati N, Cardinale L, Busso M, Boccuzzi F, Tullio M, Lamorte A, Stefanone V, Ferrari G, Veltri A, Frascisco MF. Semi-quantification of pneumothorax volume by lung ultrasound. Intensive Care Med 2014;40:1460-7. [PubMed]
- Oveland NP, Lossius HM, Wemmelund K, Stokkeland PJ, Knudsen L, Sloth E. Using thoracic ultrasonography to accurately assess pneumothorax progression during positive pressure ventilation: a comparison with CT scanning. Chest 2013;143:415-22. [PubMed]
- Zhang Z. Double lung point in an 18-month-old child: a case report and literature review. J Thorac Dis 2015;7:E50-3. [PubMed]
- Aspler A, Pivetta E, Stone MB. Double-lung point sign in traumatic pneumothorax. Am J Emerg Med 2014;32:819.e1-2.
- Soldati G, Sher S, Copetti R. If you see the contusion, there is no pneumothorax. Am J Emerg Med 2010;28:106-7. [PubMed]
- Volpicelli G, Audino B. The double lung point: an unusual sonographic sign of juvenile spontaneous pneumothorax. Am J Emerg Med 2011;29:355.e1-2.
- Brook OR, Beck-Razi N, Abadi S, Filatov J, Ilivitzki A, Litmanovich D, Gaitini D. Sonographic detection of pneumothorax by radiology residents as part of extended focused assessment with sonography for trauma. J Ultrasound Med 2009;28:749-55. [PubMed]
- Chung MJ, Goo JM, Im JG, Cho JM, Cho SB, Kim SJ. Value of high-resolution ultrasound in detecting a pneumothorax. Eur Radiol 2005;15:930-5. [PubMed]
- Donmez H, Tokmak TT, Yildirim A, Buyukoglan H, Ozturk M, Yaşar Ayaz U, Mavili E. Should bedside sonography be used first to diagnose pneumothorax secondary to blunt trauma? J Clin Ultrasound 2012;40:142-6. [PubMed]
- Goodman TR, Traill ZC, Phillips AJ, Berger J, Gleeson FV. Ultrasound detection of pneumothorax. Clin Radiol 1999;54:736-9. [PubMed]
- Lichtenstein DA, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M. Ultrasound diagnosis of occult pneumothorax. Crit Care Med 2005;33:1231-8. [PubMed]
- Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest 2008;133:204-11. [PubMed]
- Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD, Jiang GY. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care 2006;10:R112. [PubMed]
- Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care 2013;17:R208. [PubMed]
- Ebrahimi A, Yousefifard M, Mohammad Kazemi H, Rasouli HR, Asady H, Moghadas Jafari A, Hosseini M. Diagnostic Accuracy of Chest Ultrasonography versus Chest Radiography for Identification of Pneumothorax: A Systematic Review and Meta-Analysis. Tanaffos 2014;13:29-40. [PubMed]
- Simon BC, Paolinetti L. Two cases where bedside ultrasound was able to distinguish pulmonary bleb from pneumothorax. J Emerg Med 2005;29:201-5. [PubMed]


