Bilateral reversible basal ganglia changes associated with dystonia and hemifacial spasms in central nervous system lupus
Case description
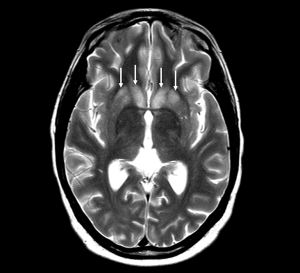
A 40-year-old woman with systemic lupus erythematosus (SLE) and associated inflammatory polyarthritis presented to the rheumatology outpatient clinic with acute episodes of facial spasms. The spasms were bilateral, involving her face and eyelids and had the appearance of dystonic spasms. Her speech was also affected, and she reported word-finding difficulties. An MRI brain, performed urgently, showed bilateral symmetrical basal ganglia signal changes on T2 (Figure 1). The neurological symptoms and imaging changes were thought to be due to an acute flare of her lupus with central nervous system (CNS) involvement. She was treated with a course of high dose steroids (a weekly reducing regime of oral prednisolone, over a period of 2 months, starting at 60 mg per day). Her symptoms resolved within 2 days of the onset of the steroid treatment. An interval MRI brain at 1 month follow-up showed complete resolution of the basal ganglia signal change.
Discussion
To our knowledge, this is the first report in the literature of facial spasm (orofacial dystonia) and corresponding MRI changes, in a patient with SLE presenting with CNS involvement (CNS lupus). Our patient’s movement disorder presented acutely, with corresponding bilateral basal ganglia changes on MRI. Treatment with immunosuppression led to complete resolution both of the clinical symptoms and of the changes seen on imaging.
The etiology of the movement disorder in CNS lupus and of the related neuroimaging changes is not well understood, but an autoantibody-mediated neurotoxic effect has been hypothesized, leading to impaired basal ganglia cell function and development of neuroinflammation (1).
Basal ganglia involvement in SLE is rare but has been described with seizures (2), and in patients with chorea or Parkinsonian symptoms (3,4). More recently, reversible basal ganglia lesions have also been reported in neuropsychiatric lupus in children (5), although none of these cases described facial spasms or dystonia.
Cranial MRI scans should be obtained during acute exacerbations of lupus or following events that may disrupt the blood-brain barrier. This may reveal unexpected CNS lesions, which may contribute towards effective planning of dosage and duration of immunosuppressive therapy.
Acknowledgements
The authors wish to thank the patient for giving us permission for publication.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kuroe K, Kurahashi K, Nakano I, Morimatsu Y, Takemori H. A neuropathological study of a case of lupus erythematosus with chorea. J Neurol Sci 1994;123:59-63. [PubMed]
- Shibata M, Kibe T, Fujimoto S, Ishikawa T, Murakami M, Ichiki T, Wada Y. Diffuse central nervous system lupus involving white matter, basal ganglia, thalami and brainstem. Brain Dev 1999;21:337-40. [PubMed]
- Kashihara K, Nakashima S, Kohira I, Shohmori T, Fujiwara Y, Kuroda S. Hyperintense basal ganglia on T1-weighted MR images in a patient with central nervous system lupus and chorea. AJNR Am J Neuroradiol 1998;19:284-6. [PubMed]
- Kwong KL, Chu R, Wong SN. Parkinsonism as unusual neurological complication in childhood systemic lupus erythematosus. Lupus 2000;9:474-7. [PubMed]
- Sato S, Nakajima J, Shimura M, Kawashima H, Yoshio T, Hara Y. Reversible basal ganglia lesions in neuropsychiatric lupus: a report of three pediatric cases. Int J Rheum Dis 2014;17:274-9. [PubMed]


