Cardiac CT imaging in coronary artery disease: Current status and future directions
Abstract: Computed tomography has undergone rapid developments over the last decades, in particular, the emergence and technological improvements of multislice CT scanners enable satisfactory performance of cardiac CT imaging. Cardiac CT has been widely used in the diagnosis of coronary artery disease, which is the leading cause of death in industrialized countries. Cardiac CT also provides valuable information to predict the extent and prognosis of coronary artery disease. The main disadvantage of cardiac CT imaging is radiation dose, which raises concern in recent years, as there is potential risk of radiation-induced malignancy. This article will provide an overview of the current research status of cardiac CT imaging in the diagnosis of coronary artery disease, highlight the key applications of cardiac CT imaging and briefly discuss future directions of this fast advancing technique.
Key words: Cardiac computed tomography; coronary artery disease; diagnosis; radiation
Introduction
Computed tomography (CT) has been gaining widespread acceptance in clinical practice since its invention in the 1970s. However, cardiac imaging with the use of conventional CT has been limited due to the fact that cardiac motion interferes with conventional CT reconstruction algorithms and leads to loss of morphological details due to motion-related artefacts. Traditionally, cardiac imaging has been dominated by invasive coronary angiography. However, this has changed with the development of multislice CT scanners. The main applications of multislice CT in cardiac imaging are demonstrated in the detection and assessment of degree of coronary stenosis and prediction of disease outcomes (1-5).
In addition to the above applications, cardiac CT demonstrates the potential to characterize atherosclerotic plaques, visualize coronary artery wall morphology and identify non-stenotic plaques that may not be detected by invasive coronary angiography (6-8). The purpose of this paper is to provide an overview of cardiac CT imaging with a focus on the diagnostic and prognostic value in coronary artery disease. Radiation dose issues associated with cardiac CT imaging are discussed; limitations and future directions of cardiac CT are highlighted.
Characterization of coronary plaques
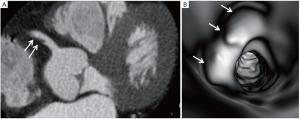
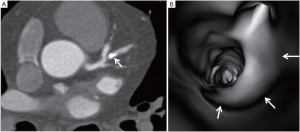
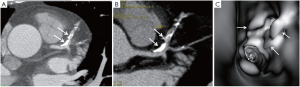
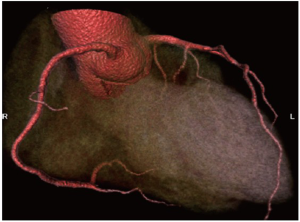
Coronary artery plaque was characterized into the following three types based on the CT attenuation: non-calcified plaques refer to plaques having lower density compared with the contrast-enhanced vessel lumen (Figure 1); calcified plaques indicate plaques with high density (Figure 2); mixed plaques refer to plaques with non-calcified and calcified elements within a single plaque or within a segment of the coronary artery (Figure 3). In addition, the calcified plaques can be further characterized into focal and extensive types according to the distribution of the plaques along the coronary artery (Figure 4).
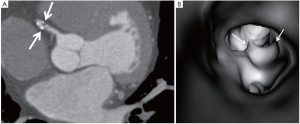
Classification of plaques by cardiac CT based on composition has important clinical implications, with increasing numbers of mixed plaques associated with adverse major cardiac events (9-11). Emerging data suggests that mixed plaque burden is more likely associated with an increased risk of adverse cardiac events. Feuchtner et al. in their prospective study analysed 1,060 patients with an intermediate risk of coronary artery disease referred for 64-slice CT coronary angiography and assessed whether there were differences in plaque composition and plaque burden in patients with coronary stenosis (12). Their results showed significant differences in plaque burden according to the severity of coronary stenosis, with mixed type of plaque being a significant indicator of adverse cardiac events due to its association with the high prevalence of obstructive coronary stenosis. This observation is supported by a recent multicentre study, ACCURACY trial, which was designed to determine the plaque composition in relation to the lumen stenosis (13). Min et al. in their multicentre trial showed patients with mixed plaque composition more often demonstrated obstructive coronary stenosis at both per-segment and per-patient assessments when compared to those with non-calcified and calcified plaques, while calcified plaques rarely resulted in obstructive stenosis. Therefore, plaque composition rather than the degree of luminal stenosis may be predictive of the patient’s risk for developing cardiac events.
Diagnostic value of cardiac CT in coronary artery disease
Diagnostic value of cardiac CT in coronary artery disease has been significantly increased with the developments of multislice CT scanners and electrocardiographygated (ECG) scanning and retrospectively reconstructed techniques. Early studies with use of 4- and 16-slice CT showed moderate diagnostic accuracy in the diagnosis of coronary artery disease due to technical limitations (1,14). Diagnostic accuracy was further increased with 64-slice CT due to improved spatial and temporal resolution, thus leading to shorter examination times and better visualization of coronary arteries. Several systematic reviews and meta-analyses reported high sensitivities and specificities of 64-slice CT coronary angiography in the diagnosis of coronary artery disease (15-19). The main limitation of 64-slice CT angiography is that patient’s heart rate must be controlled to lower than 64 beats per minute (bpm) with use of beta-blockers to ensure optimal image quality for diagnostic purposes. This has been overcome to a greater extent with the development of dual-source CT as the temporal resolution has been significantly improved compared to single-source 64-slice CT (20,21).
Studies performed with dual-source CT coronary angiography have demonstrated high diagnostic accuracy for diagnosis of coronary artery disease, and most importantly the image quality is independent of heart rate (22-24). It has been reported that dual-source CT demonstrated the superior advantage in patients with high heart rates, and most importantly, high diagnostic image quality was achieved with lower doses in dual-source CT than that of single-source CT (25-27) (Figure 5).
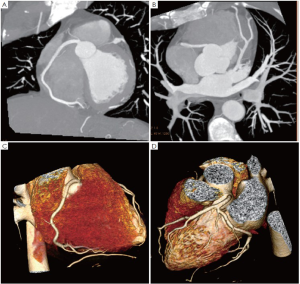
Further technical developments and expansion of multislice CT systems from a 64-slice to 256- and 320-slice system have allowed for the accurate assessment of coronary stenosis and atherosclerotic plaque composition, or even the acquisition of whole-heart coverage in one gantry rotation (28-30) (Figure 6). Despite these advantages, the temporal resolution (135 ms and 175 ms) of 256- and 320-slice CT is inferior to that of dual-source CT (83 ms), thus, high radiation dose associated with 256- and 320-slice CT needs to be addressed in future technical developments.
Prognostic value of cardiac CT in coronary artery disease
In recent years, cardiac CT is increasingly used to provide the prognostic information about coronary artery disease. Studies based on a single centre experience reported that findings of cardiac CT have been closely associated with future cardiac events, with 0% or 1% cardiac events being reported in patients with normal cardiac CT or mild coronary artery disease, and up to 30% in patients with one or more vessel obstructive CAD (11,31,32). The extent of coronary atherosclerotic plaque as well as the presence of proximal atherosclerotic plaque was found to be associated with a significantly increased risk of a major adverse cardiac event (31). Prognostic value of cardiac CT can be further enhanced by determination of plaque composition (noncalcified and mixed plaque burden), as reported in a recent study (33).
The CT-STAT trial, a prospective multi-center trial evaluating 700 patients presenting to the emergency department with acute chest pain symptoms further confirmed the prognostic value of cardiac CT (34). These findings demonstrated that the presence and severity of atherosclerotic plaque on cardiac CT were independent predictors of acute coronary syndrome. Despite these promising results, the prognostic value of cardiac CT in patients with suspected coronary artery disease needs to be further verified in cohorts with a large range of coronary artery calcium and inclusion of multi-centers (35,36).
Radiation dose related to cardiac CT
Radiation dose is becoming a major issue for cardiac CT, since CT is a high dose modality, and CT-related radiation risk is not negligible. The radiation risks associated with cardiac CT have become a hot topic of debate in the literature (37-40). The general view about radiation dose is that CT is associated with a risk of cancer development. Therefore, cardiac CT should be performed with dosesaving strategies whenever possible to reduce the radiation exposure to patients.
A number of techniques have been introduced to reduce the radiation dose in cardiac CT imaging without compromising image quality. These dosereduction techniques include ECG-controlled tube current modulation, lower x-ray tube voltage, high pitch, prospective ECG-triggered scanning and reconstruction algorithms (41,42). Of these dose-saving strategies, prospective ECG-triggering is the most effective approach in terms of dose reduction and high diagnostic accuracy when compared to conventional retrospective ECG-gated protocol (41-43). High pitch protocol is another strategy which is only achievable with the second generation of dualsource CT scanners, Siemens Definition Flash. This dualsource CT mode has high temporal resolution (75 ms) and it enables cardiac CT to be performed at high pitch value of up to 3.4, with dose lower than 1 mSv reported in some studies (44,45), thus, significantly reducing the radiation dose. There is no doubt that tremendous progress has been made to reduce the radiation dose associated with cardiac CT imaging, with a radiation dose of less than 10 mSv to as low as 1 mSv in some studies. It is important to note that the effective doses from current cardiac CT imaging are at the same level or even lower than those acquired from invasive coronary angiography.
Limitations and future directions of cardiac CT
The main challenge in cardiac CT is that there is a strong demand on high temporal resolution which translates into the time required to acquire cardiac images in a very short period. A temporal resolution of 75 ms is achieved with the recent models of dual-source CT scanners, and this demonstrates a significant improvement in cardiac imaging. However, the temporal resolution of these models is still significantly inferior to that of invasive coronary angiography, which is 10 ms, therefore, aggressive approaches such as heart rate control with the use of beta-blockers still constitute an essential step in the current cardiac CT imaging. Further technical developments of multislice CT scanners in temporal resolution will benefit more patients, especially for those with higher or irregular heart rates.
The spatial resolution of current multislice CT scanners is excellent, which ranges from 0.4 to 0.5 mm, and this is close to the spatial resolution of invasive coronary angiography, which is between 0.1 and 0.2 mm. Thus, cardiac CT allows accurate assessment of main coronary arteries and side branches with high diagnostic accuracy. Despite this achievement, cardiac CT is unable to determine which plaques are ‘vulnerable’ or unstable versus those which are stable (46). Therefore, differentiation of lipid-rich content from fibrous content with cardiac CT remains challenging due to considerable overlap in the attenuation values of lipid and fibrous tissue (47).
Summary and conclusion
Cardiac CT represents the most rapidly developed imaging modality in cardiac imaging, with satisfactory results achieved in the diagnosis of coronary artery disease. Cardiac CT demonstrates high accuracy for detection and diagnosis of coronary artery disease, characterization of atherosclerotic plaques and prediction of disease outcome.
Radiation dose associated with cardiac CT has increased significantly over the last decade due to widespread use of CT and this should draw attention to the clinicians responsible for referring patients for CT examinations. Accurate risk stratification for appropriate selection of cardiac CT is crucial, and both radiologists and referring cardiologists need to work together to develop better selection criteria for patients referred for cardiac CT.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Nieman K, Oudkerk M, Rensing BJ, et al. Coronary angiography with multi-slice computed tomography. Lancet 2001;357:599-603.
- Achenbach S, Giesler T, Ropers D, et al. Detection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated multislice computed tomography. Circulation 2001;103:2535-8.
- Sun Z, Jiang W. Diagnostic value of multislice CT angiography in coronary artery disease: A meta-analysis. Eur J Radiol 2006;60:279-86.
- Cademartiri F, Maffei E, Palumbo A, et al. Diagnostic accuracy of computed tomography coronary angiography in patients with a zero calcium score. Eur Radiol 2010;20:81-7.
- Carrigan TP, Nair D, Schoenhagen P, et al. Prognostic utility of 64-slice computed tomography in patients with suspected but no documented coronary artery disease. Eur Heart J 2009;30:362-71.
- Sun Z, Dimpudus FJ, Nugroho J, et al. CT virtual intravascular endoscopy assessment of coronary artery plaques: A preliminary study. Eur J Radiol 2010;75:e112-9.
- Motoyama S, Sarai M, Harigay H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol 2009;54:49-57.
- Miszalski-Jamka T, Klimeczek P, Banys R, et al. The composition and extent of coronary artery plaque detected by multislice computed tomographic angiography provides incremental prognostic value in patients with suspected coronary artery disease. Int J Cardiovasc Imaging 2012;28:621-31.
- Pundziute G, Schuijf JD, Jukema JW, et al. Head-tohead comparison of coronary plaque evaluation between multislice computed tomography and intravascular ultrasound radiofrequency data analysis. JACC Cardiovasc Interv 2008;1:176-82.
- Lin F, Shaw LJ, Berman DS, et al. Multidetector computed tomography coronary artery plaque predictors of stressinduced myocardial ischemia by SPECT. Atherosclerosis 2008;197:700-9.
- Pundziute G, Schuijf JD, Jukema JW, et al. Prognostic value of multislice com- puted tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol 2007;49:62-70.
- Feuchtner GM, Cury RC, Jodocy D, et al. Differences in coronary plaque composition by noninvasive computed tomography angiography in individuals with and without obstructive coronary artery disease. Atherosclerosis 2011;215:90-5.
- Min JK, Edwards M, Lin FY, et al. Relationship of coronary artery plaque composition to coronary artery stenosis severity: results from the prospective multicentre ACCURACY trial. Atherosclerosis 2011;219:573-8.
- Kuettner A, Trabold T, Schroeder S, et al. Noninvasive detection of coronary artery lesions using 16-detector row multislice spiral computed tomography technology: initial clinical results. J Am Coll Cardiol 2004;44:1230-7.
- Sun Z, Lin CH, Davidson R, et al. Diagnostic value of 64-slice CT angiography in coronary artery disease: A systematic review. Eur J Radiol 2008;67:78-84.
- Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R, et al. Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology 2007;244:419-28.
- Abdulla J, Abildstrom Z, Gotzsche O, et al. 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J 2007;28:3042-50.
- Mowatt G, Cook JA, Hillis GS, et al. 64-slicecomputed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and metaanalysis. Heart 2008;94:1386-93.
- Stein PD, Yaekoub AY, Matta F, et al. 64-slice CT for diagnosis of coronary artery disease: a systematic review. Am J Med 2008;121:715-25.
- Johnson TR, Nikolaou K, Busch S, et al. Diagnostic accuracy of dual-source computed tomography in the diagnosis of coronary artery disease. Invest Radiol 2007;42:684-91.
- Alkadhi H, Stolzmann P, Scheffel H, et al. Radiation dose of cardiac dual-source CT: the effect of tailoring the protocol to patient-specific parameters. Eur J Radiol 2008;68:385-91.
- Ropers U, Ropers D, Pflederer T, et al. Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J Am Coll Cardiol 2007;50:2393-8.
- Fang XM, Chen HW, Hu XY, et al. Dual-source CT coronary angiography without heart rate or rhythm control in comparison with conventional coronary angiography. Int J Cardiovasc Imaging 2010;26:323-31.
- Brodoefel H, Burgstahler C, Tsiflikas I, et al. Dualsource CT: Effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology 2008;247:346-55.
- Wang M, Qi HT, Wang XM, et al. Dose performance and image quality: dual source CT versus single source CT in cardiac CT angiography. Eur J Radiol 2009;72:396-400.
- Guo SL, Guo YM, Zhai YN, et al. Diagnostic accuracy of first generation dual-source computed tomography in the assessment of coronary artery disease: a meta-analysis from 24 studies. Int J Cardiovasc Imaging 2011;27:755-71.
- Baumüller S, Leschka S, Desbiolles L, et al. Dual-source versus 64-section CT coronary angiography at lower heart rates: comparison of accuracy and radiation dose. Radiology 2009;253:56-64.
- Chao SP, Law WY, Kuo CJ, et al. The diagnostic accuracy of 256-row computed tomographic angiography compared with invasive coronary angiography in patients with suspected coronary artery disease. Eur Heart J 2010;31:1916-23.
- Rybicki FJ, Otero HJ, Steigner ML, et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 2008;24:535-46.
- de Graaf FR, Schuijf JD, van Velzen JE, et al. Diagnostic accuracy of 320-row multidetector computed tomography coronary angiography in the non-invasive evaluation of significant coronary artery disease. Eur Heart J 2010;31:1908-15.
- Carrigan TP, Nair D, Schoenhagen P, et al. Prognostic utility of 64-slice computed tomography in patients with suspected but no documented coronary artery disease. Eur Heart J 2009;30:362-71.
- Chow BJ, Wells GA, Chen L, et al. Prognostic value of 64-slice cardiac computed tomography severity of coronary artery disease, coronary atherosclerosis, and left ventricular ejection fraction. J Am Coll Cardiol 2010;55:1017-28.
- Miszalski-Jamka T, Klimeczek P, Banys R, et al. The composition and extent of coronary artery plaque detected by multislice computed tomographic angiography provides incremental prognostic value in patients with suspected coronary artery disease. Int J Cardiovasc Imaging 2012;28:621-31.
- Goldstein JA, Chinnaiyan KM, Abidov A, et al. The CTSTAT (Coronary computed tomographic angiography for systematic triage of acute chest pain patients to treatment) trial. J Am Coll Cardiol 2011;58:1414-22.
- Alexanderson E, Canseco-León N, Iñarra F, et al. Prognostic value of cardiovascular CT: is coronary artery calcium screening enough? The added value of CCTA. J Nucl Cardiol 2012. [Epub ahead of print].
- Mark DB, Berman DS, Budoff MJ, et al. ACCF/ ACR/AHA/ NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: A report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol 2010;55:2663-99.
- Paul JF, Abada HT. Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol 2007;17:2028-37.
- Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007;357:2277-84.
- Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA 2009;301:500-7.
- Raff GL, Chinnaiyan KM, Share DA, et al. Radiation dose from cardiac computed tomography before and after implementation of radiation dose-reduction techniques. JAMA 2009;301:2340-8.
- Sabarudin A, Sun Z, Ng KH. A systematic review of radiation dose associated with different generations of multidetector CT coronary angiography. J Med Imaging Radiat Oncol 2012;56:5-17.
- Sun Z, Choo GH, Ng KH. Coronary CT angiography: current status and continuing challenges. Br J Radiol 2012;85:495-510.
- Sun Z, Ng KH. Multislice CT angiography in cardiac imaging. Part III: radiation risk and dose reduction. Singapore Med J 2010;51:374-80.
- Achenbach S, Marwan M, Ropers D, et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogramtriggered high-pitch spiral acquisition. Eur Heart J 2010;31:340-6.
- Lell M, Marvan M, Schepis T, et al. Prospectively ECGtriggered high-pitch spiral acquisition for coronary CT angiography using dual source CT: technique and initial experience. Eur Radiol 2009;19:2576-83.
- Matter CM, Stuber M. Hahrendorf.Imaging of the unstable plaque: how far have we got? Eur Heart J 2009;30:2566-74.
- Hoffmann U, Moselewski F, Nieman K, et al. Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable angina by multidetector computed tomography. J Am Coll Cardiol 2006;47:1655-62.


