Humongous right atrial lipoma: a correlative CT and MR case report
Introduction
Primary cardiac neoplasms are rare, occurring in only 0.001-0.03% of patients in autopsy series (1). Although histologically benign in the sense that they do not metastasize, benign cardiac neoplasms may lead to significant morbidity and mortality by affecting blood flow and causing arrhythmias and emboli (1). Lipomas are the second most common benign cardiac tumor after myxomas (1). They are encapsulated collections of adipose cells and can manifest in a wide age group. Many are discovered incidentally, but some can manifest due to symptomatic obstruction to blood flow or compression of the ventricles, especially if they have arisen in the pericardial space. They may arise in both an epicardial and endocardial location, although the majority appears to be sub-epicardial, expanding into the pericardial space.
We hereby describe a case of a giant cardiac lipoma arising from the sub-endocardium of the free wall of the right atrium cavity and projecting into the atrial cavity.
Case description
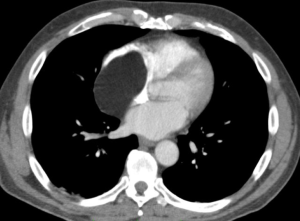
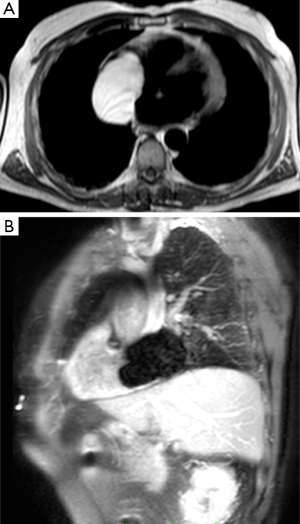
A 66-year-old man was referred to our department for further investigation of a right atrial mass identified on ultrasound examination (US) examination carried out in another hospital during a visit of occupational medicine. The patient complained for the past few months of shortness of breath during exercise. There were no significant electrocardiographic findings on electrocardiogram. US examination revealed an oval, large, hypoechoic mass measuring 53 mm × 27 mm in maximum diameter, arising from the free wall of right atrium with a broad base of attachment and projecting into the cavity; this mass did not determine obstruction to blood flow or compression of the adjacent ventricles and the patient had preserved left ventricular systolic function with global ejection fraction of 60%. According to US findings, a diagnosis of atrial myxoma was made. After US examination the patient underwent cardiac MR imaging in order to better understand the anatomy and the nature of the lesion. MR was performed using the superconducting system 1.5T MR (Gyroscan Intera, Philips Medical System, Best, The Netherlands) with a maximum gradient capability of 30 mT/m and maximum slew rate of 150 mT/ms. MR acquisition was triggered by ECG and were acquired T1-weighted sequence and cine-MR images in the short-axis, vertical long-axis and horizontal long-axis planes for displaying cardiac contraction. Short time inversion recovery (STIR) sequence was obtained in order to suppress fatty tissue signal. Finally were acquired 3D delayed-enhancement 10, 15 and 20 min after the intravenous injection of Gd-DTPA at 0.1 mmoL/kg. MR confirmed the presence in the right atrial cavity of an oval well circumscribed and encapsulated mass with sharp and regular margins, measuring 7.6 mm × 5.5 cm in maximum diameter and projecting into the right atrial cavity. This mass was homogeneously hyperintense on T1-weighted images (Figure 1A) and completely hyperintense on fat-suppressed sequence STIR; in addition the mass did not show enhancement after intravenous administration of contrast material (Figure 1B). The mass showed close relationship with the superior vena cava without signs of infiltration and did not determine obstruction to blood flow or compression to the ventricles. In order to support MR findings, a cardiac CT exam was subsequently carried out before and after administration of 100 mL of iodinated material contrast. On CT scan, the lesion appeared as a homogeneous, encapsulated, hypodense mass arising from the endocardium, projecting into the right atrial chamber, with no enhancement after contrast administration (Figure 2). Both MR and CT examinations were suggestive for a large sub-endocardial atrial lipoma. Subsequently, the patient underwent surgical excision of the lesion. The surgery was performed through a median sternotomy with aorto-bicaval cardiopulmonary by pass, total extra corporeal circulation, anterograde cardioplegia and then with the incision of the right atrium. The mass occupying the whole atrium, the inferior vena cava and infiltrating great part of the free wall of the atrium was isolated and removed. It was not possible to reconstruct the free wall of the right atrium with a pericardium patch; therefore the surgeons used a wide patch of Gore-Tex measuring 6 cm × 6 cm in maximum diameter. The final diagnosis was consistent with a large atrial lipoma (Figure 3).
Discussion
The overall frequency of cardiac tumors is quite low, with an estimated prevalence of 0.002-0.3% at autopsy and 0.15% on echocardiographic series (1). The majority of primary cardiac tumors are benign; of these, myxoma is by far the commonest, with lipomas and fibromas occurring less frequently (2,3). Metastatic involvement of the heart is approximately 40 times more prevalent than primary cardiac tumors. Metastatic spread can be by direct invasion (from adjacent neoplasms such as those of the bronchus and breast), hematologic spread (such as malignant melanoma, lymphoma, or leukemia), or transvenous spread through the great veins (such as renal cell carcinoma or hepatoma) (2,3). The initial diagnostic imaging modality likely to be employed in the assessment of suspected cardiac neoplasia is transthoracic echocardiography (3). This is limited in its imaging capability by several well-described factors such as operator experience, restricted field of view, and unfavorable patient body habitus, potentially leading to incomplete assessment of an invading cardiac mass (3). Transesophageal echocardiography is not limited by issues of suitable acoustic windows but is an invasive technique and has a relatively narrow field of view, thus offering only limited views of relevant structures, in particular the aortic arch, inferior vena cava, and left ventricular apex. Both echocardiographic techniques are limited in their ability to allow characterization of soft-tissue masses (3). Cardiac MR is an established technique in the evaluation of cardiac neoplasia (4). It is non-invasive, does not use radiation, and offers multiplanar imaging without restrictions on the available field of view. This allows accurate confirmation of the presence of a space-occupying lesion, localization and assessment of the extent of involvement, evaluation of the functional impact of the lesion, and tissue characterization. The subsequent information yielded provides an accurate assessment of any cardiac or juxtacardiac mass, emphasizing that cardiac MR imaging has an important role to play not only in the diagnosis but also for prognosis and appropriate treatment planning. The advantages of cardiac MR imaging over the more widely accessible echocardiography are superior resolution and soft-tissue contrast, greater ability to allow tissue characterization, and, through its much larger fields of view, an ability to demonstrate involvement of the adjacent mediastinum and lungs in a malignant process. An important diagnostic limitation of cardiac MR imaging is the inability to demonstrate the presence of calcifications within the mass; therefore, MR should always be combined with either plain radiography or CT to assess for the presence of calcifications. CT is faster, easier to perform, and generally has more reliable image quality. Conversely, MR imaging has better soft-tissue contrast than CT and allows much greater flexibility in the selection of imaging planes.
In this article, we report a case of primary giant cardiac lipoma not diagnosed by US examination that needed MR and CT evaluation in order to better understand the features and the nature of the lesion. Primary cardiac lipomas are benign neoplasms composed of mature adipose tissue and are histologically similar to extracardiac soft-tissue lipomas (1). The number of reported cases is not clear because some series do not differentiate between lipoma and lipomatous hypertrophy of the atrial septum (1), which is not a true neoplasm. In asymptomatic patients, the tumors may be found incidentally because of a chest X-ray abnormality (5) or heart murmur (6). Intracavitary lipomas may cause obstruction with related symptoms. Lipomas in the pericardial space may compress the ventricles (1) or may cause shortness of breath by displacing the lungs without affecting left ventricular function (7). There have been a few reported cases of children with tuberous sclerosis with multiple cardiac lipomas; generally, however, cardiac lipomas do not occur as part of a syndrome (1). They frequently arise from the epicardial surface, usually from a broad pedicle, and grow into the pericardial space (1,7). They may also arise from the endocardium and grow as broad-based, pedunculated masses into any of the cardiac chambers (1). The echocardiographic appearance of lipomas varies with their location. Lipomas in the pericardial space may be completely hypoechoic (8) or be completely echogenic. Lipomas arising from the interatrial septum have been mistaken for myxomas (9); however, lipomas have a broad base of attachment (9) and are not as mobile as myxomas. Although lipomas can be differentiated from typical myxomas, they cannot be distinguished from other cardiac masses with similar morphologic characteristics at echocardiography. Both CT and MR imaging can help to identify the presence of fat with a high degree of specificity and can therefore be used to correctly diagnose cardiac lipomas. In our case, the mass showed the typical features of an adipose lesion, presenting high signal intensity on T1 weighted images, low signal intensity on STIR sequences with no enhancement after intravenous contrast material administration. On CT scan, the mass behaved according to its nature and histology, appearing homogeneously hypodense with no enhancement after contrast material administration. The main differential diagnosis is lipomatous infiltration of the interatrial septum. This is characterized by infiltration of adipocytes between the atrial muscle cells and is defined as any deposit of fat in the atrial septum exceeding 2 cm in transverse diameter. However, lipomatous hypertrophy of the interatrial septum is caused by an increase in the number of adipocytes, not hypertrophy, so that the term is actually a misnomer (1). It is unencapsulated and occurs in older overweight patients who frequently are in atrial fibrillation. On MR imaging, it again will demonstrate the well-described high-signal-intensity characteristics of fat with sparing of the fossa ovalis and a consequent dumbbell shape (10-12). Appropriate treatment of cardiac lipoma consists of surgical resection, thus avoiding the morbidity associated with late complications.
In conclusion the multiplanar assessment of the anatomy, tissue characteristics, and functional impact of a cardiac or juxta-cardiac mass obtained by cardiac MR imaging allows accurate differentiation among benign and malignant tumors and can overcome the limits of conventional US that usually lead to an incomplete assessment of cardiac masses.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Burke A, Virmani R. Tumors of the heart and great vessels. In: Atlas of tumor pathology. Series 3, Fasc 16. Washington, DC: Armed Forces Institute of Pathology, 1996:1-98.
- Urba W, Longo DL. Primary solid tumors of the heart. In: Kapoor AS, editor. Cancer and the heart. New York: Springer-Verlag, 1986:62.
- Sparrow PJ, Kurian JB, Jones TR, Sivananthan MU. MR imaging of cardiac tumors. Radiographics 2005;25:1255-76. [PubMed]
- Puvaneswary M, Edwards JR, Bastian BC, Khatri SK. Pericardial lipoma: ultrasound, computed tomography and magnetic resonance imaging findings. Australas Radiol 2000;44:321-4. [PubMed]
- Semelka RC, Shoenut JP, Wilson ME, Pellech AE, Patton JN. Cardiac masses: signal intensity features on spin-echo, gradient-echo, gadolinium-enhanced spin-echo, and TurboFLASH images. J Magn Reson Imaging 1992;2:415-20. [PubMed]
- Siripornpitak S, Higgins CB. MRI of primary malignant cardiovascular tumors. J Comput Assist Tomogr 1997;21:462-6. [PubMed]
- Hananouchi GI, Goff WB 2nd. Cardiac lipoma: six-year follow-up with MRI characteristics, and a review of the literature. Magn Reson Imaging 1990;8:825-8. [PubMed]
- Kamiya H, Ohno M, Iwata H, Ohsugi S, Sawada K, Koike A, Ogawa K, Yano Y, Hayase S, Horiba M. Cardiac lipoma in the interventricular septum: evaluation by computed tomography and magnetic resonance imaging. Am Heart J 1990;119:1215-7. [PubMed]
- Mullen JC, Schipper SA, Sett SS, Trusler GA. Right atrial lipoma. Ann Thorac Surg 1995;59:1239-41. [PubMed]
- Doshi S, Halim M, Singh H, Patel R. Massive intrapericardial lipoma, a rare cause of breathlessness. Investigations and management. Int J Cardiol 1998;66:211-5. [PubMed]
- Mousseaux E, Idy-Peretti I, Bittoun J, et al. MR tissue characterization of a right atrial mass: diagnosis of a lipoma. J Comput Assist Tomogr 1992;16:148-51. [PubMed]
- Heyer CM, Kagel T, Lemburg SP, Bauer TT, Nicolas V. Lipomatous hypertrophy of the interatrial septum: a prospective study of incidence, imaging findings, and clinical symptoms. Chest 2003;124:2068-73. [PubMed]