
Adrenal and renal abscesses following glue embolization of gastric varices: a case description
Case report
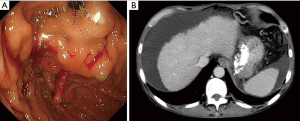
A 59-year-old man with cirrhosis and portal hypertension presented with melena and was found to have bleeding gastric varices on upper endoscopy. 1.2 mL of Histoacryl glue (B Braun Medical, Bethlehem, PA) was injected into gastric varices at the cardia (Figure 1). Haemostasis was achieved and he was discharged. In the subsequent months, he had recurrent episodes of fever partially responsive to antibiotic treatment. During an admission six months after the initial endoscopic treatment, blood cultures yielded Klebisella spp. He was investigated with computed tomography (CT) which revealed multiple multiloculated rim-enhancing lesions in the left adrenal gland and upper pole of the left kidney, with perifocal fat stranding, in keeping with abscesses. The glue cast was seen along the cardia and lesser curvature of the stomach, extending through serpiginous vasculature into the left adrenal gland and adrenal vein. The gastric varices were obliterated.
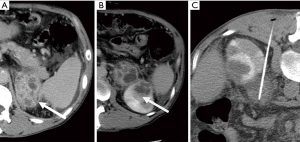
The patient was treated by CT-guided aspiration of the left adrenal abscess (Figure 2) by the interventional radiologist and systemic antibiotics. Culture of the aspirated pus confirmed Klebsiella spp. He improved clinically and follow-up CT six months later showed complete resolution of the abscesses. The patient remained well.
Discussion
Gastric varices are present in up to 78% of patients with portal hypertension and though the risk of bleeding is relatively low (up to 36%), it often presents as torrential bleeding and leads to high mortality (1). Conventional treatment options comprise supportive measures including blood transfusion, drugs such as propranolol, endoscopic intervention including sclerotherapy, ligation, or stenting, and radiological intervention such as transjugular intrahepatic portosystemic shunt (TIPS) or balloon-occluded retrograde transvenous obliteration (BRTO).
In recent years, cyanoacrylate monomer-based glue such as Histoacryl has emerged as a first line endoscopic treatment of gastric varices. The glue is mixed with lipiodol and polymerizes to form a cast upon contact with an ionic substance such as blood. Histoacryl glue is associated with a higher variceal obliteration rate and lower rebleeding risk as compared to other agents such as alcohol, powders, or band ligation (2), hence it is recommended for first line endoscopic treatment in the Baverno VI Consensus and in the American Association for the Study of Liver Disease practice guidelines (3,4).
Histoacryl glue injection is a generally safe treatment with overall complication rate of approximately 1% and mortality risk of 0.5%. Commonly reported complications include variceal rebleeding, ulceration, or erosion, blockage of injection catheter, local thrombosis of the portal venous system, sepsis, or uncommonly distant embolization if there is a right-to-left shunt (5).
Sepsis secondary to Hisoacryl embolization is uncommon and reported on a case basis in the literature. A brief literature review showed scattered reports of post-embolization sepsis involving the splenic vein (6), portal vein (7), pancreas (8), and retrogastric region (9). Lee et al. provided the only account of adrenal abscesses as a complication, when the patients presented 4-6 months afterwards (10).
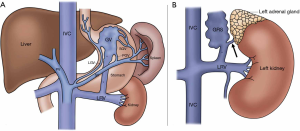
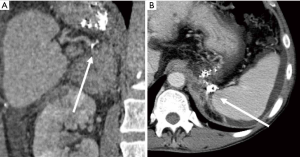
The etiopathogenesis is unknown and we propose a theory based on knowledge accrued by interventional radiologists performing BRTO procedures. Gastric varices are supplied by the left, posterior, as well as short gastric veins, and shunt into the systemic circulation more commonly through a gastrorenal shunt than a gastrocaval shunt. The classic gastrorenal shunt empties into the left renal vein along with the left adrenal vein (Figure 3) (11). We propose that the renal and adrenal abscesses in our patient could have occurred due to reflux of glue cast through the gastrorenal shunt into the adrenal vein, leading to poor clearance of gut microbes received from the portovenous system, thereby creating a septic nidus (12). The direct visualization of the glue cast on CT within the left adrenal gland and adrenal vein provided direct evidence for this theory (Figure 4).
The patient was treated by CT guided percutaneous aspiration of the left adrenal abscess in prone position using a 19-G needle performed the next day, and completed a two-week course of intravenous antibiotics. Culture of the aspirated pus yielded Klebsiella species, which was consistent with his persistent Klebisella bacteremia on prior repeat blood cultures. His fever soon subsided, white cell counts normalized, and he was discharged 6 days after the drainage with no further septic complaints afterwards. Gallium whole-body scintigram performed one month later did not find any gallium-avid focus in the left adrenal bed. Follow-up CT scan six months later showed complete resolution of both the renal and left adrenal abscesses, with only mild stranding remaining in the left retroperitoneal space. There was no evidence of recanalization of gastric varices.
This case highlights that the potential complication, be it thrombosis or sepsis, depends very much on the anatomy of the portosystemic shunts. Awareness of this association and the relevant anatomy is key to enable appropriate investigations for early diagnosis and treatment in patients who present with sepsis after variceal embolization.
Conclusions
We report a rare case of delayed development of renal and adrenal abscesses following Histoacryl glue embolization of gastric varices, demonstrating the anatomy of the classic gastrorenal shunt. Physicians should be aware of this association, including the relevant anatomy, and be ready to investigate appropriately to permit early diagnosis and treatment.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/qims-19-1026). The authors have no conflicts of interest to declare.
Ethical Statement: IRB approval was not required for this article per guidelines of our institution’s IRB and no informed consent was required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Akahoshi T, Hashizume M, Shimabukuro R, Tanoue K, Tomikawa M, Okita K, Gotoh N, Konishi K, Tsutsumi N, Sugimachi K. Long-term results of endoscopic Histoacryl injection sclerotherapy for gastric variceal bleeding: a 10-year experience. Surgery 2002;131:S176-81. [Crossref] [PubMed]
- Weilert F, Binmoeller KF. Endoscopic Management of Gastric Variceal Bleeding. Gastroenterology Clinics 2014;43:807-18. [Crossref] [PubMed]
- de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: report of the Baveno VI consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol 2015;63:743-52. [Crossref] [PubMed]
- Garcia-Tsao G, Sanyal A, Grace N, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38. [Crossref] [PubMed]
- Al-Hillawi L, Wong T, Tritto G, Berry PA. Pitfalls in histoacryl glue injection therapy for oesophageal, gastric and ectopic varices: A review. World J Gastrointest Surg 2016;8:729-34. [Crossref] [PubMed]
- Liu CH, Tsai FC, Liang PC, Lee CZ, Yang PM. Splenic vein thrombosis and Klebsiella pneumoniae septicemia after endoscopic gastric variceal obturation therapy with N-butyl-2-cyanoacrylate. Gastrointest Endosc 2006;63:336-8. [Crossref] [PubMed]
- Chang CJ, Shiau YT, Chen TL, Hou MC, Sun CH, Liao WC, Lin HC, Lee SD. Pyogenic portal vein thrombosis as a reservoir of persistent septicemia after cyanoacrylate injection for bleeding gastric varices. Digestion 2008;78:139-43. [Crossref] [PubMed]
- Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Suga T. Inflammatory tumor in pancreatic tail induced by endoscopic ablation with cyanoacrylate glue for gastric varices. J Gastroenterol 2004;39:475-8. [Crossref] [PubMed]
- Hussain I, Kwek AEB, Meyyur Aravamudan V, Chong CH, Ang TL. A Rare Case of Retrogastric Abscess Occurring Six Months after N-Butyl-2-Cyanoacrylate Injection into Gastric Varices. Case Rep Med 2018;2018:7028578. [Crossref] [PubMed]
- Lee BY, Jang JY, Jeong SW, Bok GH, Ham JH, Cho JY, Lee JS, Shim CS. Two cases of adrenal abscesses following Histoacryl (N-butyl-2-cyanocrylate) injection. Gut Liver 2011;5:242-4. [Crossref] [PubMed]
- Saad WEA, Kitanosono T, Koizumi J, Hirota S. The Conventional Balloon-Occluded Retrograde Transvenous Obliteration Procedure: Indications, Contraindications, and Technical Applications. Techniques in Vascular and Interventional Radiology 2013;16:101-51. [Crossref] [PubMed]
- Wright G, Matull WR, Zambreanu L, et al. Recurrent bacteremia due to retained embolized glue following variceal obliteration. Endoscopy 2009;41 Suppl 2:E56-57. [Crossref] [PubMed]


