Multidetector CT assessment of partial anomalous pulmonary venous return in association with sinus venosus type atrial septal defect
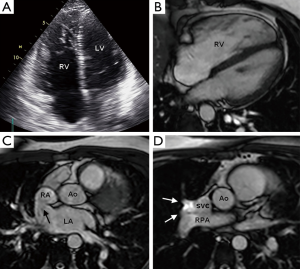
A 32-year-old man with no significant past medical history presented with a history of exertional dsyncope and palpitations. Clinical examination was unremarkable. Electrocardiogram showed partial right bundle branch block with abnormal repolarisation in V2-V4 and a transthoracic echocardiogram (TTE) showed a dilated and hypertrabeculated right ventricle (Figure 1A). A cardiac MRI study was undertaken for suspected arrythmogenic right ventricular cardiomyopathy. This showed a superior sinus venosus type atrial septal defect (SV-ASD) with partial anomalous pulmonary venous return (PAPVR) of the right superior pulmonary vein into the superior vena cava (SVC) as the cause for right heart enlargement (Figure 1B-D). Volumetric MRI data showed a left to right shunt fraction of 2:1. A multidetector computed tomography (MDCT) angiography study was undertaken to map the pulmonary veins prior to surgical referral. This showed the anterior and posterior right upper lobe segmental veins draining via a common channel into the distal SVC at the mouth of the SV-ASD and also showed the apical right upper lobe segmental vein draining separately into the proximal SVC, 2 cm cranial to the SV-ASD (Figure 2).
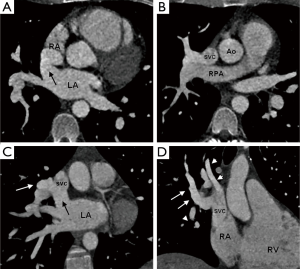
SV-ASD represents 2-12% of all ASDs and most commonly involves a communication between the right atrium-SVC junction and the left atrium (superior SV-ASD) (1). There is a frequent association with PAPVR of the right upper lobe into the SVC in 80-90% of cases which further enhances the volume of left to right shunting with an increased likelihood of pulmonary hypertension (2). Standard TTE windows may struggle to identify both a SV-ASD and PAPVR. Recently MRI and MDCT have been shown as reliable techniques for establishing the diagnosis, defining pulmonary venous anatomy and quantifying the left to right shunt fraction (3). MDCT is particularly well suited to pulmonary venous assessment because of its high spatial resolution (0.4-0.6 mm), fast acquisition speed and wide volume coverage which enables detection of very small anomalous vessels which may be overlooked on standard MRI sequences. While other forms of ASD may be amenable to percutaneous closure, treatment of SV-ASD usually requires surgery to close the defect and redirect any PAPVR (4).
Disclosure: The authors declare no conflict of interest.
References
- Oliver JM, Gallego P, Gonzalez A, Dominguez FJ, Aroca A, Mesa JM. Sinus venosus syndrome: atrial septal defect or anomalous venous connection? A multiplane transoesophageal approach. Heart 2002;88:634-8. [PubMed]
- Gaca AM, Jaggers JJ, Dudley LT, Bisset GS 3rd. Repair of congenital heart disease: a primer--Part 2. Radiology 2008;248:44-60. [PubMed]
- Kafka H, Mohiaddin RH. Cardiac MRI and pulmonary MR angiography of sinus venosus defect and partial anomalous pulmonary venous connection in cause of right undiagnosed ventricular enlargement. AJR Am J Roentgenol 2009;192:259-66. [PubMed]
- Hildick-Smith DJ, O’Sullivan M, Wisbey CR. Amplatzer device closure of atrial septal defects in mature adults: analysis of 76 cases. Heart 2004;90:334-5. [PubMed]


