
A systematic review of chest imaging findings in COVID-19
Introduction
Coronavirus disease 2019 (COVID-19) has rapidly spread across many cities in China and other countries. As of 4 April, 2020, there are over 1,000,000 confirmed cases with more than 50,000 deaths, of which more than 50% of diagnosed cases and deaths have been observed in Unites States, Spain, Italy, and Germany (1). Since the onset of COVID-19 in December 2019, many studies have reported the clinical characteristics and chest imaging appearances of COVID-19, specifically describing a variety of abnormalities in the lungs (2-4).
Although the diagnosis of COVID-19, in terms of a positive or negative test, is primarily based on laboratory tests, chest imaging modalities, including chest X-ray (CXR) and computed tomography (CT), are routine diagnostic approaches used to detect abnormal lung changes. This is due to the fact that coronavirus diseases mainly cause respiratory tract infections as seen in severe acute respiratory syndrome (SARS) and middle east respiratory syndrome (MERS) (5-7), although other organs, including the gastrointestinal tract and cardiovascular system, can also be affected (8-10). However, chest abnormalities associated with COVID-19 are different from those associated with SARS and MERS to some extent, and they are also related to the disease extent and clinical symptoms; thus, the recognition of both common and uncommon imaging findings on chest CT examinations is clinically important. Furthermore, there are some arguments about whether CT should be used as a first-line imaging technique in the diagnosis of COVID-19. In this systematic review and meta-analysis, we analyze the currently available studies documenting radiologic findings and aim to clarify the role of CT imaging in the diagnosis of patients with COVID-19.
Methods
Literature search
We performed a search of PubMed/Medline, Web of Science, ScienceDirect, Google Scholar and Scopus to identify studies reporting about COVID-19 according to the preferred reporting items for systematic reviews and meta-analysis (last search 31 March, 2020) (11,12). Different search terms were used including “novel coronavirus OR SARS-Cov-2 OR COVID-19” and “pneumonia OR infection OR chest CT OR chest imaging”. Because we intended to analyze the chest imaging appearances of patients with COVID-19 in this review, only studies meeting the following criteria were included in the analysis: original research studies reported clinical characteristics and imaging features of COVID-19 patients; studies included at least 10 patients; and studies were published in English literature. Isolated case reports or case series with a sample size of <10 were excluded due to low level of evidence. Editorials, commentaries, opinions and other types of publications were also excluded.
Data extraction
Two independent assessors (ZS and NZ) performed the data extraction with agreement reached by consensus. The following information was extracted from each study for the analysis of chest imaging findings: number of patients enrolled; mean/or median age and sex of participants; lung involvement in terms of the bilateral or unilateral lungs; lesion distribution in lungs including peripheral, central or both peripheral and central distribution; typical abnormalities including ground glass opacities (GGO) and consolidation; and less common findings including a crazy-paving pattern, air bronchogram, patchy shadow, linear opacities, bronchial wall thickening or bronchiectasis, vascular enhancement, and pleural effusion and others. The diagnostic value of CXR or chest CT in the diagnostic assessment of COVID-19 was also analyzed if data were available in the studies. Furthermore, the degree of lung involvement in terms of lesion distribution comparing peripheral with central regions, and the number of affected lobes was analyzed when information was available.
Statistical analysis
We conducted a systematic review of studies regarding diagnostic value of CT in COVID-19, comparison of CT imaging appearances in different clinical groups and COVID-19 on pregnant women or pediatric patients. We conducted a meta-analysis using a random-effects model to calculate the pooled values and their corresponding 95% confidence intervals (95% CI) of different imaging features associated with COVID-19 patients. The Likelihood ratio (LR) Chi-squared statistic test was used to assess the homogeneity across studies of the proportions of patients presenting with the specified imaging features. Measures of homogeneity between studies comparing COVID-19 with non-COVID-19 using Cochran’s Q statistic were performed. Data were entered into SPSS 25.0 (version 24.0; IBM Corporation, Armonk, NY, USA) for statistical analysis.
Results
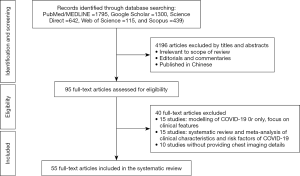
A total of 55 studies were determined (13-32) through the search with reported cases (33-52) ranging from 10 to 1,099 (53-67). Figure 1 is a flow chart outlining the search strategy of selecting these studies. Table 1 lists basic demographics and main chest imaging findings reported in each study. There is very highly significant heterogeneity between studies with respect to mean patient age. After excluding studies which only provided an age range rather than a standard deviation, 25 studies with admissible data were pooled together for analysis of patient’s age with the mean value being 48 years (95% CI: 45.1–50.9). In the following sections, we provided detailed review and analysis of chest imaging findings in COVID-19 patients in these eligible studies.

Full table
Study characteristics and lung involvement
CT was used in 52 studies for the diagnosis of COVID-19, whereas in the study by Arentz et al. (14), CXR was the only imaging modality used in diagnosing all patients. Both CXR and CT were used in one study (21), with chest CT showing superiority over CXR in detecting all types of lung abnormalities, indicating the limited value of CXR (Table 1). Another study by Wong et al. analyzed CXR findings in 64 COVID-19 patients with 69% sensitivity with reverse transcription-polymerase chain reaction (RT-PCR sensitivity 91%) as the gold standard (47). Although CXR resembles CT findings (in 28 patients) in these common abnormal lung findings, it is less sensitive than CT in detecting the abnormalities.
A total of 36 studies (65.5%) reported details regarding bilateral or unilateral lung involvement (Figure 2); of which 17 studies reported a higher percentage of bilateral lung involvement (78.22%, 95% CI: 45–100%) than unilateral lung involvement (20.23%, 95% CI: 9.90–30%) (Tables 1 and 2). These studies consistently reported that the involvement of the bilateral lungs was much higher than that of the unilateral lung in patients with COVID-19, or bilateral involvement was more frequently observed in severe or emergency cases.
Full table
Of the remaining 19 studies that did not report the details of lung involvement on chest CT, 8 reported involvement of pulmonary lobes or segments, with more than two lobes observed in all the studies (Table 1). Two studies only reported the percentage of lung abnormalities on CXR and chest CT (17,21), while the remaining nine studies did not report lung involvement (25,27,32,39,42,52,63,65,66). Eighteen studies (32.7%) reported the percentages of distribution of abnormalities or lesions in the peripheral or central or both peripheral and central lung regions on chest CT, with peripheral distribution (65.35%, 95% CI: 25.93–100%), peripheral plus central (31.12%, 95% CI: 1.96–74.07%) showing significant dominance compared with central distribution (3.57%, 95% CI: 0.99–9.80%). Wu et al. reported only the average involvement of lung segments (49), while three studies analyzed the risk of pregnant women and neonates born to mothers with COVID-19 (32,56,66), and another four studies reported COVID-19 in adults and children (39,42,50,62) which were described in detail later.
Normal chest CT images
Of the 55 studies, 26 (47.3%) reported normal chest CT findings in patients with COVID-19 (Table 1). The percentage of normal chest CT findings ranged from the lowest 0.7% to the highest 56%, depending on the severity of the disease with high normal rates reported in asymptomatic patients or with mild symptoms. The pooled value was 13.31% (95% CI: 0.74–38.36%). Furthermore, ≥20% of normal chest CT findings were noted in 10 out of 26 studies (38.5%).
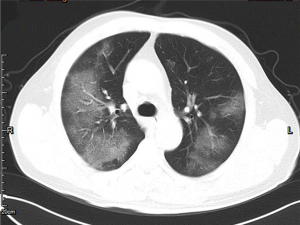
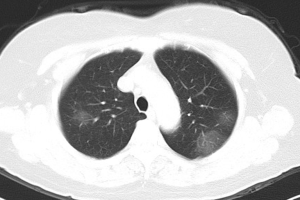
Most common chest CT imaging findings
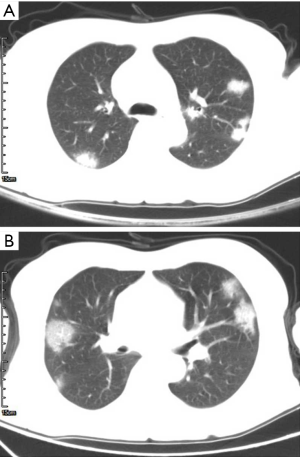
GGO and consolidation represented the most common abnormalities and were reported in 94.5% (52/55) of the studies (Table 1). The imaging appearances of these two abnormal findings were presented as either pure GGO (58.05%, 95% CI: 16.67–100%) (Figures 2,3) or GGO mixed with consolidation (52.99%, 95% CI: 19.05–76.79%) or consolidation (44.18%, 95% CI: 1.61–71.46%) only (Figure 4). The percentage of GGO or consolidation or both of them was reported in 80% of the studies (44/55) whereas in the remaining 11 studies, only bilateral GGO with or without consolidation was reported in 5 studies without providing details regarding the percentage of these lesions in study participants (24,48,53,57,59), and GGO with patchy shadows or crazy-paving pattern in 3 studies (32,38,66). The remaining 3 studies did not provide any information about these abnormal changes (34,56,62).
Other common and less common chest CT imaging findings
In addition to GGO and consolidation, other abnormal changes in the lungs were reported in 50% of the studies (28/55) (Table 1). These included common findings such as a crazy-paving pattern (Figure 5), air bronchogram (Figure 6), linear opacities (Figure 7), local or bilateral patchy shadowing (Figure 8), and interlobular septal thickening (Figure 9). Less common appearances were shown in 61.8% of the studies (34/55) including fibrous stripes (Figure 10), vascular enhancement (Figure 11), bronchiectasis (Figure 12), pleural effusion (Figure 13), nodules (Figure 14), bronchial wall thickening, spider web sign, and lymphadenopathy and others (Table 1).
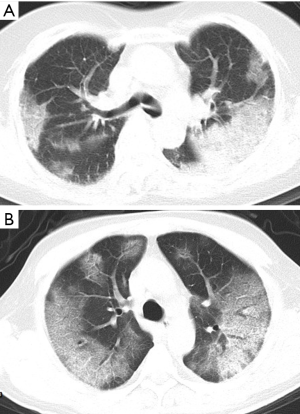
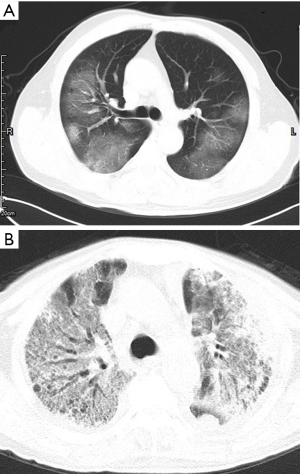
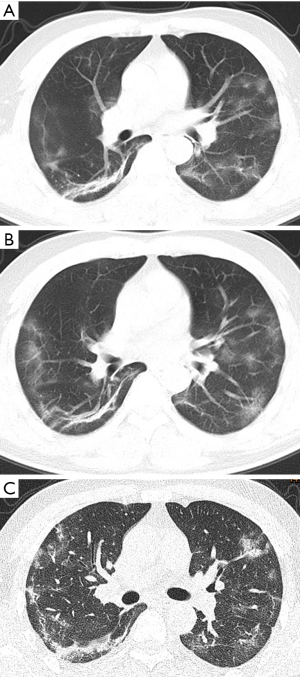
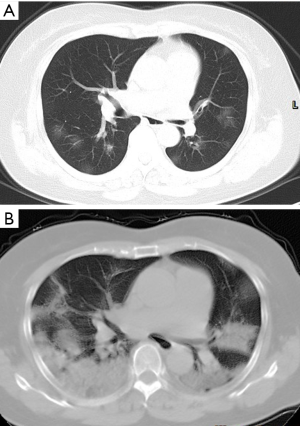
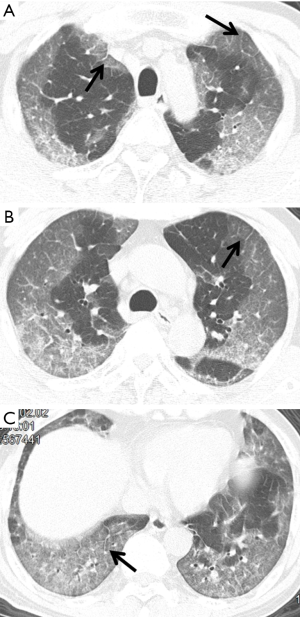
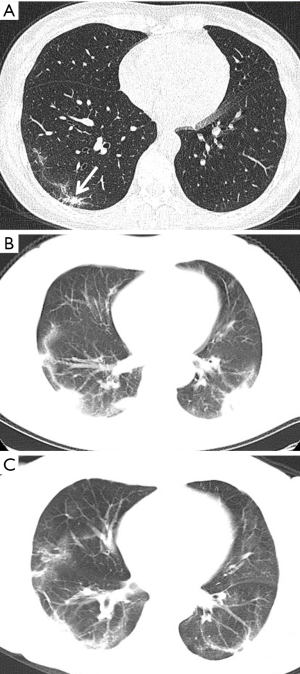

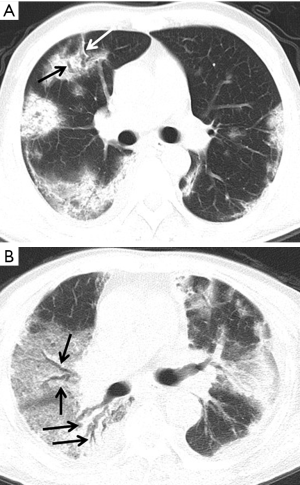
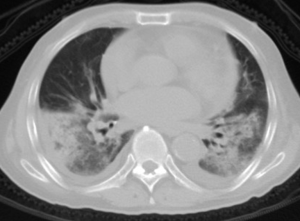
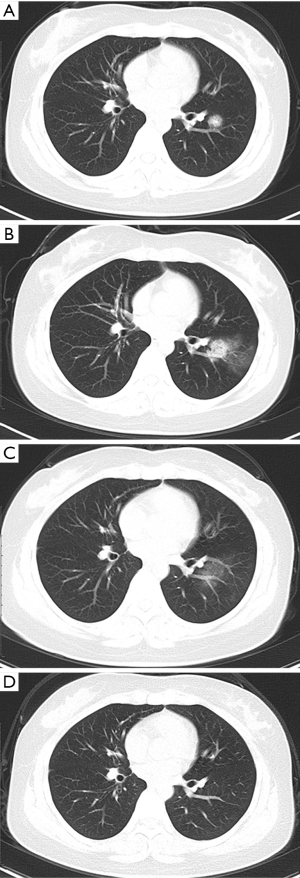
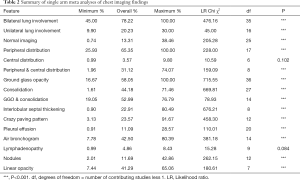
Table 2 is a summary of the meta-analysis of these imaging findings. As shown in the table, there was highly significant heterogeneity across studies with regard to the reported percentages of these findings (P<0.001), except for central distribution of pulmonary lesions and lymphadenopathy which did not show significant difference (P=0.084–0.102).
Diagnostic value of chest CT in COVID-19
The performance of chest CT in the diagnostic assessment of COVID-19 patients was reported in 9 studies documenting different aspects related to chest CT performance (13,15,19,27-29,45,61,67). The study conducted by Ai and colleagues is the first study thus far to determine the diagnostic value of chest CT in patients with COVID-19 (13). The authors analyzed 1,014 patients with suspected COVID-19, and all these patients underwent chest CT scans and nucleic acid test (RT-PCR). Of the 1,014 patients, 601 (59%) had positive RT-PCR results, and positive chest CT findings were observed in 97% of the 601 patients. With RT-PCR as the diagnostic reference for COVID-19, their results showed that the sensitivity, specificity, positive predictive value, and negative predictive value of CT were 97%, 25%, 65% and 83%, respectively. The high false positive rate of CT in detecting abnormal lung changes could be due to significant overlap with pneumonia caused by other factors such as viral pneumonia. The authors also conducted a further analysis of 258 patients who underwent multiple RT-PCR tests, and 15 of these patients showed conversion from initial negative to later positive test results. Initial chest CT images were positive in 67% of these patients, and 93% of the patients presented with typical CT imaging appearances consistent with COVID-19 diagnosis. Based on the results of a comparative analysis of the diagnostic value of CT, similar diagnostic performance was found with no significant differences between different age groups (<60 vs. ≥60 years) and between male and female patients (13). CT changes were also comparable with RT-PCR conversion according to the study conducted by Wang et al. (44).
The study conducted by Bai et al. reported the performance of radiologists in interpreting chest CT images for differentiation of COVID-19 from viral pneumonia (15). In this retrospective study, the authors assessed the accuracy of three Chinese radiologists in reading the chest CT images of 219 patients with COVID-19 and 205 patients without COVID-19. Four American radiologists reviewed 58 age-matched cases by using the similar approach as the Chinese radiologists did. The sensitivity of these seven radiologists was 80%, 67%, 97%, 93%, 83%, 73%, and 70%, respectively, and the specificity was 100%, 93%, 7%, 100%, 93%, 93%, and 100%, respectively. This study concluded that the radiologists from these two countries demonstrated high specificity but moderate sensitivity in differentiating CT images of COVID-19 from those of viral pneumonia (15). However, results of this study need to be interpreted with caution due to selection bias of participant screening strategy and the stage of pneumonia associated with the diagnostic value of CT.
The study conducted by Li et al. further confirmed the high performance of CT in the diagnosis of COVID-19 (27). By reviewing the CT images of 51 patients with COVID-19 and 2 patients with viral pneumonia, they reported a misdiagnosis rate of 3.9% for CT for COVID-19. Similar to the limitation inherent in the study by Bai et al., selection bias of the number of patients with different types of pneumonia raises concerns about concluding CT with high diagnostic value. Although their findings support the use of CT as a standard technique for the diagnosis of COVID-19, CT lacks specificity in distinguishing abnormal lung changes caused by different types of viruses (27). Similar findings were shown in Li’s study with 28% of COVID-19 patients having normal chest CT (29). Authors used CT visual quantitative method to assess lung involvement which is defined as total severity score. They concluded that chest CT alone is not suitable as a screening tool due to its association with misdiagnosis in some patients, while their approach of visual quantitative analysis has 82.6% sensitivity and 100% specificity, thus, serving as an accurate technique to assess clinical severity of COVID-19. With use of similar CT cutoff score, Li et al. (28) reported the CT sensitivity and specificity of 80% and 82.8% for detecting abnormal changes.
The study by Wang et al. reported temporal changes of CT findings in 90 patients over different stages of disease progression (45). Their results showed the pattern of CT findings was related to the disease extent and progression, reaching peaked during days of 6–11, followed by persistence of high levels. This study provides insight into the change of CT imaging patterns in COVID-19 patients.
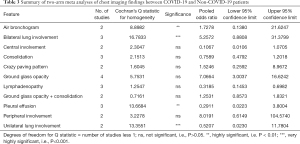
Three studies conducted by Cheng et al., Zhao et al. and Zhu et al. along with Bai et al. reported chest CT imaging differences between COVID-19 and non-COVID-19 patients (15,19,61,67). The study by Bai et al. compared the two groups of patients with inclusion of more than 200 cases in each group, representing so far the largest sample size in this aspect (15), while the other 3 studies compared two groups of patients with relatively small sample size of less than 100 patients in each group. Table 3 summarises meta analyses of imaging findings between COVID-19 and non-COVID-19. There is no significance difference in most of the imaging findings, except for bilateral lung involvement and air bronchogram with higher proportions in the COVID-19 group, unilateral lung involvement and pleural effusion which were higher in the non-COVID-19 patients.
Full table
Comparison of chest CT findings between clinical groups with COVID-19
Of the 55 studies, nearly half of the studies (43.6%, 24/55) compared chest CT findings in different clinical groups with results demonstrating significant differences in some of the CT appearances in urgent/severe/critically ill patient groups compared with mild/moderate or non-urgent/non-severe patient groups. Of these 24 studies, only 11 provided the details of chest CT imaging appearances in different groups and determined significant differences in particular findings between these groups. Table 4 lists the results of these 11 studies regarding some specific findings showing significant differences. Due to heterogeneity across these studies, only a systematic review was performed to analyze imaging findings related to different groups.

Full table
Of these 11 studies, four compared chest CT findings of patients in different stages (according to the onset of symptoms) (16,37,63,65), three compared patients based on disease severity (28,52,60), another three studies focused on clinical outcomes between patients who died/non-survivor and those who recovered/survivor (55,58,64). The remaining study by Inui et al. compared asymptomatic with symptomatic patients from the cruise ship “Diamond Princess”, with significantly higher percentage of normal chest CT scans seen in the asymptomatic patients than in the symptomatic group (P=0.012) (26). The frequency of abnormal findings, including linear or fibrous opacities, lymphadenopathy, pleural effusion, and bronchial wall thickening or distortion, was found to be significantly higher in severe/critical groups or patients in advanced situations than in early/intermediate or moderate groups (16,28,55,60,63). Common findings including GGO and consolidation did not show significant differences between different clinical groups in most of the studies, except in the study of Zhou et al. (63) who reported a significantly higher prevalence of GGO in the early phase than in the advanced phase of the disease. By contrast, in the same study conducted by Zhou et al., GGO plus reticular pattern was found to be significantly higher in the advanced phase than in the early phase. Five studies compared the crazy-paving pattern between different groups (16,28,37,58,65), but reported inconsistent findings (Table 4).
Chest imaging findings in pregnant women or pediatric patients with COVID-19
Seven studies reported findings in pregnant women with COVID-19 or in pediatric patients or neonates (32,39,42,50,56,62,66). Liu and colleagues reviewed CT scans of 15 pregnant women with confirmed COVID-19 pneumonia (32). In the early stage of disease onset, CT showed GGO, while CT findings evolved into consolidation and crazy-paving pattern as disease progressed. None of the neonates delivered during this study were infected with COVID-19. Su et al. analyzed clinical and imaging findings of 9 children and 14 families who tested positive of COVID-19. Although both adults and children presented similar findings of abnormal lung changes, 55.6% of children had normal chest CT scans which is higher than 28.6% of normal chest imaging in the adult patients (42).
The studies by Zeng et al. and Zhu et al. presented findings from a different perspective as authors performed an analysis of 33 and 10 neonates born to mothers diagnosed with COVID-19, respectively (56,66). In these retrospective studies, the authors analyzed the outcomes of neonates born to mothers with confirmed COVID-19. The chest CT findings of these pregnant women showed typical pneumonia changes such as GGO and consolidation. Zhu et al. reported that in 7 out of 10 neonates, CXR showed abnormal appearances consisting of lung infections, respiratory syndrome, and pneumothorax. The test results of COVID-19 were negative in all the neonates (66). This is consistent with the findings of another study reporting similar clinical features in 9 pregnant women with confirmed COVID-19 (68). In contrast, the study by Zeng et al. showed that 3 out of 33 neonates tested positive and this indicated that vertical transmission of virus from mothers to fetuses cannot be ruled out, hence close monitoring of neonates is necessary to detect the potential risk of COVID-19 (56).
The three other studies focused on analysis of pediatric patients with COVID-19 (39,50,62). Qiu et al. in their retrospective study investigated clinical features in 36 children with COVID-19 (39). All patients in their cohort presented with mild or moderate symptoms, whereas nearly half of them showed no abnormalities on chest imaging examinations. Similar findings were also reported by Zheng et al. who analyzed 25 confirmed pediatric children (62). Nearly one-third of chest CT scans (33.3%) were normal, while abnormal findings of pneumonia-related appearances were similar to those observed in adult patients. Xie et al. analyzed the chest CT imaging features of 20 pediatric patients with confirmed COVID-19, of which 13 had a history of close contact with family members who had received a diagnosis of COVID-19 and 7 had co-existing congenital or acquired diseases (50). Common abnormalities, such as GGO and consolidation, were also observed in more than half of the patients, accompanied by fibrotic lesions, air bronchogram, and interlobular septal thickening in the advanced stage. Subpleural lesions with local infiltration were observed in all patients. The “white lung” change was observed in the critical stage showing progression of lesions to diffuse involvement of the lungs. These chest CT findings are considerably similar to those reported in adult patients; thus, the diagnosis of COVID-19 still relies on a combination of clinical and imaging findings.
Findings of these studies indicate that adults tend to be more contracted with COVID-19 than children. When children are infected, the symptoms are mild compared to moderate or severe symptoms that are commonly seen in adults, and this is likely due to the presence of comorbidities in elderly patients such as diabetes, hypertension or cardiovascular disease which are associated with poor prognosis or high mortality.
Discussion
To the best of our knowledge, this is the first comprehensive review and analysis of the current literature on the chest imaging features of patients with COVID-19. The review summarizes the following key findings from the literature. First, chest CT findings, including GGO, consolidation, air bronchogram, crazy-paving pattern, linear opacities and bronchial wall thickening or distortion, are nonspecific because they can also be seen in pneumonia caused by other pathogens such as viral pneumonia. Furthermore, there was a relatively high proportion of normal chest CT scans, especially in early stage or asymptomatic patients (69-71). This highlights the importance of combining CT with clinical examination for the diagnosis of COVID-19. In addition, there exists inconsistency between clinical symptoms and imaging appearances, especially in early stage of COVID-19 (72,73). Second, despite potential role of CT in differentiating nonsevere from severe or critically ill patients and its clinical value in determining the disease extent and progression, this can be achieved with use of CXR, thus further highlighting the limited value of CT in COVID-19. Third, the analysis of the current literature is based on most of the studies (95%) conducted in China, with nearly all of them advocating the use of chest CT in the diagnosis of COVID-19. More evidence is needed from studies reporting patients with COVID-19 in other countries. Countries such as United States, Italy, Spain, Germany and France have more than 100,000 confirmed cases in each country (1); thus, more research findings from these countries are expected to be reported soon, although CT is not commonly used in these countries according to some early reports (14).
Currently, there are four review articles available on the chest imaging and clinical findings of COVID-19 (74-77). Ye et al. in their pictorial review presented a spectrum of chest CT findings associated with COVID-19 including a brief review of 14 studies which reported CT findings (74). Rodriguez-Morales et al. conducted a systematic review and meta-analysis of clinical, laboratory and imaging features of COVID-19 (75). Authors included 19 studies for the meta-analysis, while another 39 case reports for the descriptive analysis. Although imaging findings were included in their analysis, only information about bilateral and unilateral lung involvement, and GGO was analyzed, while other detailed findings were not included because their analysis focused more on clinical and laboratory characteristics. Salehi and colleagues analyzed chest imaging findings in 30 studies, of which 19 were case series and 11 were case reports (76). They analysis included GGO, consolidation, lung and lobar involvement, and CT findings in relation to different age groups and stage of the disease, but was limited to the analysis of cases studies. A recent study by Borges do Nascimento et al. analyzed chest imaging findings in 51 studies, but authors did not perform meta-analysis of these imaging features in their review as they briefly summarized these imaging findings while focusing more on clinical characteristics (77). Our review represents a more in-depth analysis of 55 original studies with exclusion of isolated case reports. Further, we analyzed typical, atypical CT findings and diagnostic value of CT in COVID-19 patients. In addition, comparisons of COVID-19 with non-COVID-19 studies with regard to imaging differences indicate another unique aspect of this meta-analysis. Analysis of chest abnormalities in pregnant women, children and neonates also adds extra information to these previous reviews. Thus, this systematic review and meta-analysis offers insight into clarifying the role of using chest CT in the diagnosis of COVID-19 patients.
Although increasing studies on this trending topic are available in the literature, the sample size is still small in most of these studies that were reviewed. Majority of the current reports is dominated by case studies documenting individual institution’s experience of diagnosing and treatment COVID-19 patients. Only two studies in this review included more than 1,000 cases, whereas 72.2% of the studies included <100 patients (Table 1). Furthermore, most of them reported only general imaging findings of chest CT without conducting further analysis or comparison of these findings in different categorized groups. Case reports were excluded from the analysis because they only present some initial experience of chest imaging findings in COVID-19 without providing details of frequency on abnormal lung changes. Publications in Chinese language were also excluded to avoid duplicate publication of similar research findings in English literature. Another limitation is the lack of information on mortality associated with COVID-19 because only six studies thus far have reported mortality, which ranged from 1.4% to 52.4% (14,21,30,45,58,65). Additional studies with short- to long-term follow-up of patients with COVID-19 are required so that our understanding of disease progression, including radiological abnormalities, can be improved.
As the number of COVID-19 cases continue to increase every day with no effective treatment or vaccine available so far, radiologists will encounter an increasing number of cases, with both typical and atypical manifestations of lung infection. Therefore, it is important for them to be familiar with imaging findings of COVID-19 pneumonia and assist their communication with other healthcare providers for management of COVID-19 patients. Recommendations and advice guidelines for the diagnosis and treatment of patients with COVID-19, including pregnant women and pediatric patients, are already available (78-80). The advice guidelines for COVID-19-associated pneumonia include suggestions and recommendations for clinical diagnosis and typical and atypical chest CT/CXR image manifestations based on stages, from ultra-early to progression and dissipation stages (78). This article provides guidance for frontline clinicians, including radiologists, for early diagnosis and identification of abnormal changes associated with COVID-19 and characterization of the disease extent based on CT imaging appearances. Recommendations of the diagnostic strategy for treating pediatric patients with respiratory infection and women with COVID-19 during pregnancy and puerperium are also available (79,80). According to these recommendations, chest imaging, particularly a chest CT scan, is considered an essential technique for the diagnosis and evaluation of abnormalities in the lungs. However, this contradicts with the recent statements about the appropriate use of chest imaging in COVID-19 (81-83).
The American College of Radiology statement states that CT should not be used as the first-line technique to diagnose COVID-19 due to its limited specificity in differentiating lung abnormalities (81). The Radiological Society of North America (RSNA) has also published a statement developed by imaging experts across the United States to provide guidance to radiologists reporting CT findings attributable to suspected COVID-19 pneumonia. Four categories were proposed for reporting CT findings which are potentially related to COVID-19, and routine use of CT as a screening tool is not recommended (82). The Fleischner Society has just released a consensus statement on the role of chest imaging in the management and diagnosis of COVID-19 (83). According to these recommendations, chest imaging is not indicated as a screening tool in asymptomatic or mild clinical feature patients, while chest CT is indicated for moderate to severe features of COVID-19, regardless of the laboratory test results. Although most radiology societies are not recommending the routine use of CT for screening COVID-19, the number of CT scans performed for suspected cases has significantly increased. More evidence is urgently needed to clarify the role of CT in the diagnosis of patients with COVID-19, especially findings from countries outside China are needed to determine its clinical value because most of the studies that support the use of CT as a routine and frontline technique are reported by researchers from China, thus the role of CT could be overestimated (84,85). According to a recent study, only chest radiographs were used in the diagnosis of 21 critically ill COVID-19 patients in Washington State with high accuracy in detecting all abnormal lung changes (14). More research findings from other countries are expected to provide a different view on the judicious use of CT in CIVID-19.
An alternative modality to CXR or chest CT in diagnosing lung changes of COVID-19 is the use of ultrasound which has been reported in some case studies (86-90). These case reports indicate the potential value of lung ultrasound as a secondary screening modality when RT-PCR is not available or as an alternative to CT in pregnant and pediatric patients. A recent study from Italy compared bedside lung ultrasound with CT in 12 patients with COVID-19 and showed excellent correlation between these two modalities in detecting lung abnormalities (88). Further studies are required to confirm the usefulness of lung ultrasound in the diagnosis and management of COVID-19.
In conclusion, this systematic review and meta-analysis provides a detailed analysis of the current literature on chest imaging findings in COVID-19 patients. Despite widespread use of CT in these studies, its clinical value needs to be determined due to lacking specificity in differentiating imaging appearances caused by different types of pneumonia. Diagnosis of COVID-19 is still to be confirmed by clinical and laboratory examinations. CXR still plays a role in the identification and detection of abnormal lung changes, while chest CT could serve as a complementary role in evaluating potential complications, disease severity and progression rather than a routine diagnostic approach. Appropriate guidelines should be followed with regard to the judicious use of CT in the diagnosis of COVID-19.
Acknowledgments
Authors would like to thank Mr. Gil Stevenson for his assistance in the statistical analysis.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/qims-20-564). ZS serves as an unpaid associate editor of Quantitative Imaging in Medicine and Surgery. The other authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Coronavirus disease (COVID-19) Situation Report-75. Published April 4, 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200404-sitrep-75-covid-19.pdf?sfvrsn=99251b2b_4
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Li M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JTK, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199-207. [Crossref] [PubMed]
- Gralinski LE, Menachery VD. Return of the Coronavirus: 2019-nCoV. Viruses 2020;12:135. [Crossref] [PubMed]
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W. China Novel Coronavirus Investigating and Research Team. A Novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727-33. [Crossref] [PubMed]
- Paul NS, Roberts H, Butany J, Chung T, Gold W, Mehta S, Konen E, Rao A, Provost Y, Hong HH, Zelovitsky L, Weisbrod GL. Radiologic pattern of disease in patients with severe acute respiratory syndrome: the Toronto experience. Radiographics 2004;24:553-63. [Crossref] [PubMed]
- Nicolaou S, Al-Nakshabandi NA, Muller NL. SARS: imaging of severe acute respiratory syndrome. AJR Am J Roentgenol 2003;180:1247-9. [Crossref] [PubMed]
- Das KM, Lee EY, Enani MA, AlJawder SE, Singh R, Bashir S, Al-Nakshbandi N, AlDossari K, Larsson SG. CT correlation with outcomes in 15 patients with acute Middle East respiratory syndrome coronavirus. AJR Am J Roentgenol 2015;204:736-42. [Crossref] [PubMed]
- Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, Jiang B. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet 2020;395:e52. [Crossref] [PubMed]
- Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020;17:259-60. [Crossref] [PubMed]
- Gao QY, Chen YX, Fang JY. 2019 novel coronavirus infection and gastrointestinal tract. J Dig Dis 2020;21:125-6. [Crossref] [PubMed]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [Crossref] [PubMed]
- Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, Tierney JF. PRISMA-IPD Development Group. Preferred Reporting Items for a systematic review and meta-analysis of individual participant data: The PRISMA-IPD Statement. JAMA 2015;313:1657-65. [Crossref] [PubMed]
- Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020. Epub ahead of print. [Crossref] [PubMed]
- Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi LB, Wang DC, Mei J, Jiang XL, Zeng QH, Egglin TK, Hu PF, Agarwal S, Xie F, Li S, Healey T, Atalay MK, Liao WH. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M. Chest CT findings in coronavirus disease19 (COVID19): relationship to duration of infection. Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Chang D, Lin M, Wei L, Xie L, Zhu G, Dela Cruz CS, Sharma L. Epidemiologic and clinical characteristics of Novel Coronavirus infections involving 13 patients outside Wuhan, China. JAMA 2020;323:1092-3. [Crossref] [PubMed]
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13. [Crossref] [PubMed]
- Cheng Z, Lu Y, Cao Q, Qin L, Pan Z, Yan F, Yang W. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am J Roentgenol 2020. Epub ahead of print. [Crossref] [PubMed]
- Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020;295:202-7. [Crossref] [PubMed]
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu H, Shan H, Lei CL. Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JJ, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Cheng Z, Li G, Zheng ZJ, Qiu S Q, Luo J, Ye CJ, Zhu SY, Zhong NS. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med 2020. Epub ahead of print. [Crossref] [PubMed]
- Guan CS, Lv ZB, Yan S, Du YN, Chen H, Wei LG, Xie RM, Chen BD. Imaging features of coronavirus disease 2019 (COVID-19): Evaluation on thin-section CT. Acad Radiol 2020. Epub ahead of print. [Crossref] [PubMed]
- Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D. Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia. AJR Am J Roentgenol 2020. Epub ahead of print. [Crossref] [PubMed]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- Hu Z, Song C, Xu C, Jin G, Chen Y, Xu X, Ma H, Chen W, Lin Y, Zheng Y, Wang J, Hu Z, Yi Y, Shen H. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci 2020. Epub ahead of print. [Crossref] [PubMed]
- Inui S, Fujikawa A, Jitsu M, Kunishima N, Watanabe S, Suzuki Y, Umeda S, Uwabe Y. Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19). Radiology: Cardiothorac Imaging 2020. doi: 10.1148/ryct.2020200110. [Crossref]
- Li Y, Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol 2020. Epub ahead of print. [Crossref] [PubMed]
- Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, Li C. The Clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol 2020. Epub ahead of print. [Crossref] [PubMed]
- Li K, Fang Y, Li W, Pan C, Qin P, Zhong Y, Liu X, Huang M, Liao Y, Li S. CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19). Eur Radiol 2020. Epub ahead of print. [Crossref] [PubMed]
- Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, Xiao W, Wang YN, Zhong MH, Li CH, Li GC, Liu HG. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020. Epub ahead of print. [Crossref] [PubMed]
- Liu W, Tao ZW, Lei W, Ming-Li Y, Kui L, Ling Z, Shuang W, Yan D, Jing L, Liu HG, Ming Y, Yi H. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl) 2020. Epub ahead of print. [Crossref] [PubMed]
- Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, Zheng C. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: A preliminary analysis. AJR Am J Roentgenol 2020. Epub ahead of print. [Crossref] [PubMed]
- Liu H, Liu F, Li J, Zhang T, Wang D, Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J Infect 2020. Epub ahead of print. [Crossref] [PubMed]
- Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, Xiong Y, Cheng Z, Gao S, Liang K, Luo M, Chen T, Song S, Ma Z, Chen X, Zheng R, Cao Q, Wang F, Zhang Y. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis 2020. Epub ahead of print. [Crossref] [PubMed]
- Ng MY, Lee M, Yang J, Yang F, Li X, Wang H, Lui M, Lo C, Leung B, Khong P, Hui C, Yuen K, Kuo M. Imaging profile of the COVID-19 infection: Radiologic findings and literature review. Radiology Cardiothorac Imaging 2020. https://doi.org/. [Crossref]
- Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, Hu Q, Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol 2020. Epub ahead of print. [Crossref] [PubMed]
- Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Qian GQ, Yang NB, Ding F, Ma AHY, Wang ZY, Shen YF, Shi CW, Lian X, Chu JG, Chen L, Wang ZY, Ren DW, Li GX, Chen XQ, Shen HJ, Chen XM. Epidemiologic and Clinical Characteristics of 91 Hospitalized Patients with COVID-19 in Zhejiang, China: A retrospective, multi-centre case series. QJM 2020. Epub ahead of print. [Crossref] [PubMed]
- Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis 2020. Epub ahead of print. [Crossref] [PubMed]
- Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020;20:425-34. [Crossref] [PubMed]
- Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, Ling Y, Jiang Y, Shi Y. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295:210-7. [Crossref] [PubMed]
- Su L, Ma X, Yu H, Zhang Z, Bian P, Han Y, Sun J, Liu Y, Yang C, Geng J, Zhang Z, Gai Z. The different clinical characteristics of corona virus disease cases between children and their families in China - the character of children with COVID-19. Emerg Microbes Infect 2020;9:707-13. [Crossref] [PubMed]
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020. Epub ahead of print. [Crossref] [PubMed]
- Wang L, Gao YH, Lou LL, Zhang GJ. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Respir J 2020. Epub ahead of print. [Crossref] [PubMed]
- Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, Shi H, Zhou M. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: A longitudinal study. Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Wang K, Kang S, Tian R, Zhang X, Zhang X, Wang Y. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin Radiol 2020;75:341-7. [Crossref] [PubMed]
- Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung T, Lee EYP, Wan EYF, Hung FNI, Lam TPW, Kuo M, Ng MY. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology 2019. Epub ahead of print. [Crossref] [PubMed]
- Wu J, Liu J, Zhao X, Guo D, Fang Z, Chen L, Huang H, Li C. Clinical characteristics of imported cases of COVID-19 in Jiangsu Province: A multicenter descriptive study. Clin Infect Dis 2020. Epub ahead of print. [Crossref] [PubMed]
- Wu J, Wu X, Zeng W, Guo D, Fang Z, Chen L, Huang H, Li C., Chest CT. Findings in Patients With Coronavirus Disease 2019 and Its Relationship With Clinical Features. Invest Radiol 2020;55:257-61. [Crossref] [PubMed]
- Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol 2020;55:1169-74. [Crossref] [PubMed]
- Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R, Hu T, Ding Y, Lin L, Gan Q, Luo L, Tang X, Liu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020;47:1275-80. [Crossref] [PubMed]
- Xu YH, Dong JH, An WM, Lv XY, Yin XP, Zhang JZ, Dong L, Ma X, Zhang HJ, Gao BL. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect 2020;80:394-400. [Crossref] [PubMed]
- Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, Li SB, Wang HY, Zhang S, Gao HN, Sheng JF, Cai HL, Qiu YQ, Li LJ. Clinical findings in a group of patients infected withthe 2019 novel coronavirus (SARS-Cov 2) outside of Wuhan, China: retrospective case series. BMJ 2020. [Crossref] [PubMed]
- Yang W, Cao Q, Qin L, Wang X, Cheng Z, Pan A, Dai J, Sun Q, Zhao F, Qu J, Yan F. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):A multi-center study in Wenzhou city, Zhejiang, China. J Infect 2020;80:388-93. [Crossref] [PubMed]
- Yuan M, Yin W, Tao Z, Tan W, Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS One 2020 19;15:e0230548.
- Zeng L, Xia S, Yuan W, Yan K, Xiao F, Shao J, Zhou W. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhang N, Xu X, Zhou L, Chen G, Li Y, Yin H, Sun Z. Chest CT imaging features of critically ill COVID-19 patients. Research Square 2020. doi: 10.21203/rs.3.rs-18094/v1. [Crossref]
- Zhang X, Cai H, Hu J, Lian J, Gu J, Zhang S, Ye C, Lu Y, Jin C, Yu G, Jia H, Zhang Y, Sheng J, Li L, Yang Y. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhao D, Yao F, Wang L, Zheng L, Gao Y, Ye J, Guo F, Zhao H, Gao R. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: A multicenter study. AJR Am J Roentgenol 2020;214:1072-7. [Crossref] [PubMed]
- Zheng F, Liao C, Fan QH, Chen HB, Zhao XG, Xie ZG, Li XL, Chen CX, Lu XX, Liu ZS, Lu W, Chen CB, Jiao R, Zhang AM, Wang JT, Ding XW, Zeng YG, Cheng LP, Huang QF, Wu J, Luo XC, Wang ZJ, Zhong YY, Bai Y, Wu XY, Jin RM. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr Med Sci 2020. [Epub ahead of print]. doi: 10.1007/s11596-020-2172-6. [Crossref]
- Zhou Z, Guo D, Li C, Fang Z, Chen L, Yang R, Li X, Zeng W. Coronavirus disease 2019: initial chest CT findings. Eur Radiol 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song Bin, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. [Crossref] [PubMed]
- Zhou S, Wang Y, Zhu T, Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. AJR Am J Roentgenol 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhu W, Xie K, Lu H, Xu L, Zhou S, Fang S. Initial clinical features of suspected Coronavirus Disease 2019 in two emergency departments outside of Hubei, China. J Med Virol 2020. Epub ahead of print. [Crossref] [PubMed]
- Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Xia S, Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr 2020;9:51-60. [Crossref] [PubMed]
- Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet 2020;395:809-15. [Crossref] [PubMed]
- Xu R, Du M, Li L, Zhen Z, Wang H, Hu X. CT imaging of one extended family cluster of corona virus disease 2019 (COVID-19) including adolescent patients and “silent infection”. Quant Imaging Med Surg 2020;10:800-804. [Crossref] [PubMed]
- Zeng Y, Fu J, Yu X, Huang Z, Yin X, Geng D, Zhang J. Should CT be used as a screening or follow-up tool for asymptomatic patients with SARS-CoV-2 infection? Quant Imaging Med Surg 2020. Epub ahead of print. [Crossref]
- Wáng YX. A call for caution in extrapolating chest CT sensitivity for COVID-19 derived from hospital data to patients among general population. Quant Imaging Med Surg 2020;10:798-9. [Crossref] [PubMed]
- Hu X, Chen J, Jiang X, Tao S, Zhen Z, Zhou C, Wang J. CT imaging of two cases of one family cluster 2019 novel coronavirus (2019-CoV) pneumonia: inconsistency between clinical symptoms amelioration and imaging sing progression. Quant Imaging Med Surg 2020;10:508-10. [Crossref] [PubMed]
- Zhang B, Zhang J, Chen H, Yang K, Zhang S. Unmatched clinical presentation and chest CT manifestation in a patient with severe coronavirus disease 2019 (COVID-19). Quant Imaging Med Surg 2020. Epub ahead of print. [Crossref] [PubMed]
- Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol 2020. Epub ahead of print. [Crossref] [PubMed]
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, Alvarado-Arnez LE, Bonilla-Aldana DK, Franco-Paredes C, Henao-Martinez AF, Paniz-Mondolfi A, Lagos-Grisales GJ, Ramírez-Vallejo E, Suárez JA, Zambrano LI, Villamil-Gómez WE, Balbin-Ramon GJ, Rabaan AA, Harapan H, Dhama K, Nishiura H, Kataoka H, Ahmad T, Sah R. Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19). Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis 2020. Epub ahead of print. [Crossref] [PubMed]
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic review of imaging findings in 919 patients. AJR Am J Roentgenol 2020. Epub ahead of print. [Crossref] [PubMed]
- Borges do Nascimento IJ, Cacic N, Abdulazeem HM, von Groote TC, Jayarajah U, Weerasekara I, Esfahani MA, Civile VT, Marusic A, Jeroncic A, Carvas N Junior, Pericic TP, Zakarija-Grkovic I, Meirelles Guimarães SM, Luigi Bragazzi N, Bjorklund M, Sofi-Mahmudi A, Altujjar M, Tian M, Arcani DMC, O'Mathúna DP, Marcolino MS. Novel Coronavirus Infection (COVID-19) in Humans: A scoping review and meta-analysis. J Clin Med 2020. [Crossref] [PubMed]
- Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, Fang C, Huang D, Huang LQ, Huang Q, Han Y, Hu B, Hu F, Li BH, Li YR, Liang K, Lin LK, Luo LS, Ma J, Ma LL, Peng ZY, Pan YB, Pan ZY, Ren XQ, Sun HM, Wang Y, Wang YY, Weng H, Wei CJ, Wu DF, Xia J, Xiong Y, Xu HB, Yao XM, Yuan YF, Ye TS, Zhang XC, Zhang YW, Zhang YG, Zhang HM, Zhao Y, Zhao MJ, Zi H, Zeng XT, Wang YY, Wang XH; for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM). A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 2020;6;7:4.
- Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, Li FB, Lin R, Tang LF, Wang TL, Wang W, Wang YS, Xu WZ, Yang ZH, Ye S, Yuan TM, Zhang CM, Zhang YY. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr 2020. Epub ahead of print. [Crossref] [PubMed]
- Poon LC, Yang H, Lee JCS, Copel JA, Leung TY, Zhang Y, Chen D, Prefumo F. ISUOG Interim Guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet Gynecol 2020. Epub ahead of print. [Crossref] [PubMed]
- Access 2020;13.
- Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology Cardiothorac Imaging 2020. https://doi.org/. [Crossref]
- Rubin GD, Haramati LB, Kanne JP, Schluger NW, Yim JJ, Anderson DJ, Altes T, Desai SR, Goo JM, Inoue Y, Luo F, Prokop M, Richeldi L, Tomiyama N, Leung AN, Ryerson CJ, Sverzellati N, Raoof S, Volpi A, Martin IBK, Kong C, Bush A, Goldin J, Humbert M, Kauczor HU, Mazzone PJ, Remy-Jardin M, Schaefer-Prokop CM, Wells AU. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Hope MD, Raptis CA, Shah A, Hammer MM, Henry TS. six signatories. A role for CT in COVID-19? What data really tell us so far. Lancet 2020. Epub ahead of print. [Crossref]
- Liu WH, Wang X, Cai Z, Wang X, Huang X, Jin Z. Chest CT as a screening tool for COVID-19 in unrelated patients and asymptomatic subjects without contact history is unjustified. Quant Imaging Med Surg 2020. Epub ahead of print. [Crossref] [PubMed]
- Buonsenso D, Pata D, Chiaretti A. COVID-19 outbreak: less stethoscope, more ultrasound. Lancet Respir Med 2020. Epub ahead of print. [Crossref] [PubMed]
- Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med 2020. Epub ahead of print. [Crossref] [PubMed]
- Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano Donati K, Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci 2020;24:2776-80. [PubMed]
- Poggiali E, Dacrema A, Bastoni D, Tinelli V, Demichele E, Mateo Ramos P, Marcianò T, Silva M, Vercelli A, Magnacavallo A. Can lung US help critical care clinicians in the early diagnosis of novel coronavirus (COVID-19) pneumonia? Radiology 2020. Epub ahead of print. [Crossref] [PubMed]
- Wang YXJ, Liu WH, Yang M, Chen W. The role of CT for Covid-19 patient's management remains poorly defined. Ann Transl Med 2020;8:145. [Crossref] [PubMed]


