Lymphoepithelial carcinoma arising from the maxillary antrum: a clinicopathological report of a rare lesion in an unusual site
Introduction
Lymphoepithelial carcinoma (LEC) was first described in 1921 by Schminke and Regaud, although the term LEC was coined by Hilderman et al. in 1962 (1,2). Following several attempts to classify the nasopharyngeal carcinomas, “lymphoepithelial” carcinoma of the sinonasal tract has recently been accepted as a distinct entity which is topographically distinct, yet histologically similar to the former (3). It is a poorly differentiated carcinoma equivalent to WHO type 3 nasopharyngeal carcinoma (4). Most commonly, it affects the nasal cavity, followed by the paranasal sinuses; rarely involving both. Even though salivary gland-associated LEC is a well documented entity, it is extremely uncommon in the sinonasal tract. This neoplasm has a strong aetiological association with Epstein-Barr virus (EBV) and mysteriously strong racial prevalence, with approximately 75% of affected people being Mongolian (3).
The following case report describes an Indian female with LEC of the right maxillary sinus who responded favourably to radiotherapy and remained disease free with no locoregional or distant metastasis for 20 months.
Case report
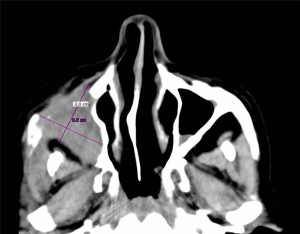
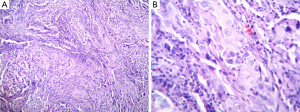
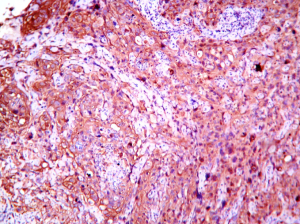
A 45-year-old Indian woman presented with a 2-month history of painful swelling in the right middle third of the face. She also reported right-side epistaxis of 45 days duration. There were no associated otolaryngological or neurological symptoms and recent history of trauma or chronic sinonasal infections were negative. Her medical and family history was non-contributory. The extraoral examination showed diffuse, firm and tender swelling on the right cheek causing some facial asymmetry. No regional lymphadenopathy was evident in the neck examination. The intraoral examination revealed hard and tender swelling, causing buccal vestibular obliteration in the right maxillary premolar-molar region. Laboratory investigations showed normal results. Paranasal sinus view revealed a hazy mass in the right antrum with evidence of irregular bony destruction. Computed tomographic (CT) scan showed a heterogeneously enhancing soft tissue mass (3.5 cm × 3 cm) with evidence of irregular bone destruction of the anterior and posterior walls of the right maxillary sinus. Central necrosis of the tumor mass was evident with the hypodense area at the centre and the medial side of the tumor mass (Figure 1). The histopathological examination revealed large round to ovoid epithelial cells infiltrating the connective tissue in irregular islands (Figure 2A). At higher magnification the tumor cells showed vesicular nuclei with prominent nucleoli and lightly staining cytoplasm with indistinct cell borders resulting in syncytial appearance (Figure 2B). Tumor cells showed moderate amount of pleomorphism and mitosis but there was no significant necrosis. The background stroma showed as dense infiltration of lymphocytes and plasma cells with few germinal centres between the tumor islands. Immunohistochemistry was performed and the cells were found to be diffusely positive for pancytokeratin (panCK) (Figure 3) revealing the epithelial nature of the tumor cells. Chromogenic in-situ hybridization for EBV encoded RNAs (EBERs) showed negative result. Based on the histopathological and immunohistochemical findings, the lesion was finally diagnosed as LEC involving the right maxillary antrum. She was subjected to external beam radiotherapy by antero-lateral portals on Cobalt60 machine. A cumulative dose of 70 Gray (Gy) was delivered with a dose of 2.0 Gy five times a week. Our patient responded satisfactorily to the treatment and has been without any evidence of LEC recurrence after 20 months.
Discussion
The LEC frequently affects nasopharynx, salivary glands and the larynx; LEC involving the maxillary sinus being exceedingly rare and seldom reported (2). Tumors involving extra pharyngeal sites with similar histologic features have been named lymphoepithelioma-like carcinomas (5). However, the use of this term has been abandoned for sinonasal tract LECs which are now regarded as a distinct entity. This is done primarily to separate it from sinonasal undifferentiated carcinoma (SNUC), which has a unique aggressive clinical disease course (3,6). The high incidence rate of sinonasal LEC among Southeast Asian countries and its rarity in other ethnic groups suggest that racial and geographical factors play a role in the development of these lesions. The association between certain human leukocyte antigen (HLA) types, the southern Chinese diet and EBV in its pathogenesis is well documented (3,7). EBV plays an important role in the pathogenesis of these lesions and this association is much stronger in Asians than in whites (6,7). Our case showed absence of the virus in LEC by IHC and in situ hybridization (EBERs). Prognosis of the maxillary sinus LEC is independent of the presence or absence of the virus, thus use of IHC for EBV determination is unnecessary. Determination of the EBV status is more valuable in diagnosing distant tumors which are suspected metastases (6).
In majority of maxillary sinus LECs, patients are either asymptomatic or present with non-specific obstructive nasal symptoms. Small sized tumors with overlapping symptoms are often misdiagnosed as chronic sinusitis, nasal polyp or lacrimal duct obstruction (2,8). In the present case, patient had maxillary swelling, due to tumor expansion through a defect in the posterolateral wall of the right maxillary sinus. Rarely, the patient may present with epistaxis, as in our case. There are no pathognomic radiological features of maxillary sinus LEC, hence the final diagnosis cannot be confirmed clinicoradiologically (2). Maxillary sinus LEC presents a diagnostic challenge to the oral diagnostician who may find it difficult to make a pre-operative diagnosis. Definitive diagnosis of a LEC is established by the histopathological and immunohistochemical analysis. LEC has typical microscopic features showing epithelial cells with eosinophilic cytoplasm with an intermixed reactive lymphoplasmacytic infiltrate. Immunohistochemistry shows strong staining for panCK in the epithelial component of LECs, whereas immunereactivity for melanin A marker and CK 20 is negative (2,5).
It is very important to make the correct diagnosis for the appropriate treatment. For proper treatment planning, CT scans and magnetic resonance imaging are used to assess the local extent of the tumor (6). The definitive diagnosis is often deferred and this indolent tumor is typified by locally advanced disease at diagnosis. Sinonasal LECs prefer spreading locally and none have shown neck metastasis, similar to our case. Even though, local spread is fairly common at the time of diagnosis, the prognosis remains favourable as compared to other poorly differentiated epithelial tumors (6). This is probably due to the presence of prominent lymphoid tissue, which may represent a host response against the tumor, and to its biological characteristics, including responsiveness to radiotherapy (9). Even though, surgery has been the treatment choice for maxillary sinus tumors, there is no established treatment approach for LECs due to rarity of the reported cases. LEC is known to be radiosensitive and hence radiation is the cornerstone of therapy, even when there is lymph node metastasis. With extensive or advanced disease, adjuvant chemotherapy (pre-, concurrent, or post-radiation) and neck management may be required (2,10). Our treatment plan included a course of radiotherapy without chemotherapy, as there was no neck involvement. The recurrence rate for maxillary sinus LEC is as high as 25 percent, necessitating a long term follow-up with CT scans (2,3).
In summary, we report a case of EBV-negative LEC of the maxillary sinus with detailed clinical, histopathological and immunohistochemical information. This report should serve to remind us that even a harmless appearing swelling could be a rare malignancy. Only a cautious approach aided with wisely chosen diagnostic tests can help to make a pre-operative diagnosis of this rare and challenging tumor. It is therefore, imperative for the maxillofacial diagnosticians to maintain a high index of suspicion to allow for early recognition and timely referral of the patients.
Disclosure: The authors declare no conflict of interest.
References
- Hilderman WC, Gordon JS, Large HL Jr, Carroll CF Jr. Malignant lymphoepithelial lesion with carcinomatous component apparently arising in parotid gland. A malignant counterpart of benign lymphoepithelial lesion? Cancer 1962;15:606-10. [PubMed]
- Mohammed D, Jaber A, Philippe M, Kishore S. Lymphoepithelial carcinoma in the maxillary sinus: a case report. J Med Case Rep 2012;6:416. [PubMed]
- Zong Y, Liu K, Zhong B, Chen G, Wu W. Epstein-Barr virus infection of sinonasal lymphoepithelial carcinoma in Guangzhou. Chin Med J (Engl) 2001;114:132-6. [PubMed]
- Wu FY, Yang ES, Willey CD, Ely K, Garrett G, Cmelak AJ. Refractory lympho-epithelial carcinoma of the nasopharynx: a case report illustrating a protracted clinical course. Head Neck Oncol 2009;1:18. [PubMed]
- Han AJ, Xiong M, Gu YY, Lin SX, Xiong M. Lymphoepithelioma-like carcinoma of the lung with a better prognosis. A clinicopathologic study of 32 cases. Am J Clin Pathol 2001;115:841-50. [PubMed]
- Rytkönen AE, Hirvikoski PP, Salo TA. Lymphoepithelial carcinoma: two case reports and a systematic review of oral and sinonasal cases. Head Neck Pathol 2011;5:327-34. [PubMed]
- Spencer CR, Skilbeck CJ, Thway K, Nutting CM. Lymphoepithelial carcinoma of the parotid gland: a rare neck lump. JRSM Short Rep 2012;3:28. [PubMed]
- Som PM, Brandwein M. Sinonasal cavities. Inflammatory diseases, tumors, fractures and postoperative findings. In: Som PM, Hugh D. eds. Head and neck imaging (3rd ed). St Louis: Mosby, 1996:57.
- Ambrosio MR, Mastrogiulio MG, Barone A, Rocca BJ, Gallo C, Lazzi S, Leoncini L, Bellan C. Lymphoepithelial-like carcinoma of the parotid gland: a case report and a brief review of the western literature. Diagn Pathol 2013;8:115. [PubMed]
- Tsang WYW, Chan JKC. Lymphoepithelial carcinoma. In: Barnes EL, Eveson JW, Reichart P, Sidransky D. eds. Pathology and genetics of tumours of head and neck tumours. (Kleihues P, Sobin LH, series editors. World Health Organization classification of tumours.) Lyon, France: IARC Press, 2005:18.


