
Ultrasound diagnosis of an inflammatory granuloma secondary to a fishbone in the gallbladder
Introduction
The accidental ingestion of a foreign body is common in clinic, of which fishbone is the most common. In most cases, the fishbone passes through the gastrointestinal tract without getting stuck (1). The rate of perforation is very low with reports of <1% of foreign bodies perforating bowel (2). Due to anatomy of the bowel, the most common site of perforation is the terminal ileum (3). Penetration in the duodenum and the development of a granuloma of the gallbladder is quite rare. Furthermore, the clinical symptoms with a foreign body perforation are nonspecific and different, and a definite preoperative diagnosis may be challenging.
Case presentation
A 56-year-old man presented to a local hospital complaining of transient abdominal pain, bloating, nausea, vomit, decreased appetite, and low fever for several days. His symptoms relieved after having a rest without treatment. Days later, he was referred to our hospital for further treatment with a slight discomfort again.
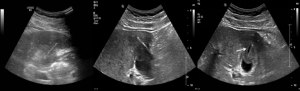
In our outpatient department, this patient underwent a contrast-enhanced ultrasound examination. The B-mode images showed a hypoechoic mass (49 mm × 41 mm) with an unclear boundary at the gallbladder fundus invading the right lobe of the liver parenchyma nearby and with a hyperechoic ‘strip’ (30 mm × 2 mm) inside. Except for the central part, enhanced ultrasound showed that lesion was hyperechoic in arterial and portal venous phase, isoechoic to hypoechoic in delayed phase (Figure 1). The lesion was diagnosed as an inflammatory granuloma located at the transition site of the gallbladder fundus and liver parenchyma. The non-enhanced part was considered to be a purulent cavity. The hyperechoic ‘strip’ was considered as a foreign body, with no obvious sign indicating the origin of this foreign body. After hospitalization, this patient completed the laboratory test within the following three days, which showed a mild increase of the white cell (9.73×109/L) and one tumor marker (carcinoembryonic antigen, CEA: 5.03 ng/mL). Next, the patient had B-mode ultrasound again, which showed the hyperechoic ‘strip’ moved slightly. A fistula was seen in the hypoechoic mass (Figure 2).

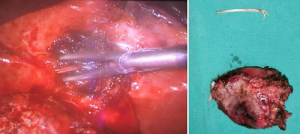
After the consultation, the hepatobiliary surgeon decided to perform cholecystectomy surgery for this patient. During the laparoscopy surgery process, the duodenal perforation, adjacent omentum, and duodenal adhesion were noted, and a fishbone in purulent liver parenchyma near the inflammatory granuloma at the gallbladder fundus was confirmed (Figure 3). After the operation, the patient recovered well and was discharged without complications.
Discussion
There have been a few reports of liver abscess caused by foreign body perforation (4,5). However, the granuloma secondary to a fishbone in the gallbladder is extremely rare and never reported.
Tracing the patient’s medical history back, he had no memory about this fishbone because the fishbone had not gotten stuck on the throat or esophagus during being swallowed. Small and linear bones have more chances of easy distal passage as compared with large and triangular bones (6). The tumor mark CEA of the patient elevated possibly related to the inflammatory response of the hepatobiliary system (7).
This fishbone passed through the spacious stomach cavity and reached the curved narrow duodenum. Duodenal perforation and omentum adhesion explained that the hard and sharp fishbone punctured the wall of duodenum, which caused the patient's initial discomfort. After that, the fishbone was pushed by the abdominal organs to reach the gallbladder fossa, and then penetrated the bottom wall of the gallbladder and then the liver parenchyma, led to the chronic inflammatory response of the body, i.e., the formation of the inflammatory granuloma and abscess. The fishbone might also move slightly following the patient’s breathing or posture changing, which could explain the intermittent discomfort of the patient. The interval US examination recorded the slight movement of the fishbone. This case report provides a reference for clinicians.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/qims.2020.03.13). The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pinero Madrona A, Fernández Hernández JA, Carrasco Prats M, Riquelme Riquelme J, Parrila Paricio P. Intestinal perforation by foreign bodies. Eur J Surg 2000;166:307-9. [Crossref] [PubMed]
- Mateus JE, Silva C, Beirão S, Pimentel J. Hepatic Abscess Induced by Fish Bone Migration: Two Case Reports. Acta Med Port 2018;31:276-9. [Crossref] [PubMed]
- Dai J, Kapadia CR. Transverse colon perforation secondary to fish bone ingestion. J Surg Case Rep 2019;2019:rjy368. [Crossref] [PubMed]
- Bekki T, Fujikuni N, Tanabe K, Amano H, Noriyuki T, Nakahara M. Liver abscess caused by fish bone perforation of stomach wall treated by laparoscopic surgery: a case report. Surg Case Rep 2019;5:79. [Crossref] [PubMed]
- Lemaître M, Cabral D, Salomon E, Geri G. En route to the liver: an fishbone's unexpected journey. Intensive Care Med 2018;44:1148-9. [Crossref] [PubMed]
- Devaraja K, Nayak DR, Bhandarkar AM, Sharma PV. Usual suspects: the foreign bodies of the aerodigestive tract. BMJ Case Rep 2018. [Crossref] [PubMed]
- Hall C, Clarke L, Pal A, Buchwald P, Eglinton T, Wakeman C, Frizelle F. A Review of the Role of Carcinoembryonic Antigen in Clinical Practice. Ann Coloproctol 2019;35:294-305. [Crossref] [PubMed]


