Incidental finding of elongated ventral duct in a case of pancreatic divisum mimicking double pancreatic ducts on magnetic resonance cholangiopancreaticography—a rare normal variant
Introduction
Congenital anomalies and normal variants of pancreas are often missed till second decade and usually present later with recurrent pancreatitis or upper gastrointestinal obstruction. Recognition of these variants is extremely significant as they are surgically correctable. Moreover, identifying these anomalies may prevent ductal injury during surgery. We report an uncommon variant of pancreatic duct with pancreatic divisum and long ventral duct and also discuss the embryologic development (1).
Case presentation
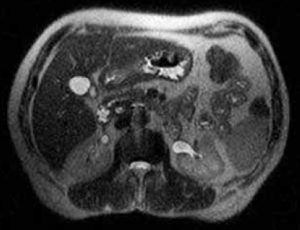
A 35-year-old female patient presented with a 2-month history of upper abdominal pain along with jaundice. On general physical examination there was icterus and tenderness in the right upper quadrant of abdomen. Routine laboratory investigations showed elevated conjugated and unconjugated bilirubin suggesting obstructive jaundice. Magnetic resonance imaging (MRI) of upper abdomen was advised along with magnetic resonance cholangiopancreaticography (MRCP) to rule out choledocholithiasis and for detailed evaluation of hepatobiliary system. On MRI there was evidence of cholelithiasis and choledocholithiasis (Figure 1) along with presence of pancreatic divisum as both ventral and dorsal ducts were opening separately into duodenum into major & minor ampulla respectively. The ventral duct draining posterior head and uncinate process of pancreas was quite elongated mimicking duplication of pancreatic duct, which was quite uncommon finding (Figures 1,2,3). We could not find similar image of this unusual variant in the literature.


Discussion
Pancreas develops from fusion of dorsal and ventral buds which develop as outgrowths of primitive foregut between fifth and seventh week of gestation. The anterior head, body and tail of pancreas develop from dorsal and posterior head and uncinate process from ventral bud. The ductal systems also unite after this fusion. The portion of dorsal duct distal to fusion is known as main pancreatic duct and remaining proximal part as duct of Santorini (which opens in minor papilla). The part of ventral duct between fusion and major papilla is termed as duct of Wirsung. Therefore pancreatic duct is most commonly seen as a bifid configuration with a dominant duct of Wirsung (2).
The other less common variants include an absent duct of Santorini, a dominant duct of Santorini without divisum, pancreatic divisum, ansa pancreatica, duplication anomalies and cystic dilatations of terminal portions of the ducts of Wirsung and Santorini (Wirsungocele and Santorinicele) (1,2).
Pancreatic divisum results from failure of fusion of dorsal and ventral ducts of pancreas. It occurs in approximately 4 to 14 percent of the population. It has three subtypes. Type 1 or classical divisum is the most common type in which no communication exists between the dorsal and ventral pancreatic ducts. Type 2 has absent ventral duct and type 3 shows a small communicating branch between the two (3). Nevertheless, in all these cases major drainage of pancreatic secretions is through the minor papilla via the duct of Santorini, except the posterior head and uncinate process which drains into the major papilla via the duct of Wirsung with the common bile duct (CBD). Its clinical significance is still questionable as some cases of pancreatic divisum are associated with recurrent pancreatitis and other cases are detected as incidental findings in asymptomatic patients (4).
It can be diagnosed using various non-invasive imaging modalities like multidetector computed tomographic scans & MRCP along with invasive modalities like endoscopic retrograde cholangiopancreaticography (ERCP). On imaging, it can be seen as ventral duct which does not communicate with the dorsal duct joining with distant CBD to drain through the major ampulla and the dorsal pancreatic duct in direct continuity with the duct of Santorini draining into minor ampulla (5).
Though pancreatic divisum is not a rare variant, but extra-long ventral duct mimicking double pancreatic ducts as was seen in our case was quite unusual.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mortelé KJ, Rocha TC, Streeter JL, Taylor AJ. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics 2006;26:715-31. [PubMed]
- Türkvatan A, Erden A, Türkoğlu MA, Yener Ö. Congenital variants and anomalies of the pancreas and pancreatic duct: imaging by magnetic resonance cholangiopancreaticography and multidetector computed tomography. Korean J Radiol 2013;14:905-13. [PubMed]
- Quest L, Lombard M. Pancreas divisum: opinio divisa. Gut 2000;47:317-9. [PubMed]
- Yu J, Turner MA, Fulcher AS, Halvorsen RA. Congenital anomalies and normal variants of the pancreaticobiliary tract and the pancreas in adults: part 2, Pancreatic duct and pancreas. AJR Am J Roentgenol 2006;187:1544-53. [PubMed]
- Nijs EL, Callahan MJ. Congenital and developmental pancreatic anomalies: ultrasound, computed tomography, and magnetic resonance imaging features. Semin Ultrasound CT MR 2007;28:395-401. [PubMed]


