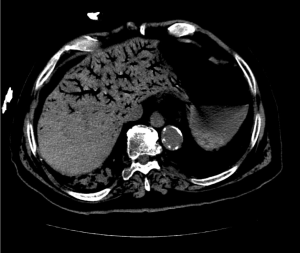
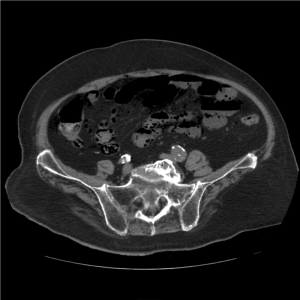
Classic pneumatosis intestinalis and hepatic portal venous gas in setting of severe abdominal aorta atherosclerosis
An 86-year-old man with extensive past medical history including cardiovascular diseases and coronary artery bypass grafting, chronic heart failure (EF 35-40%), hypertension, cerebrovascular attack, dementia (poor baseline mental status); deep vein thrombosis, history of falls and recent admission for right non displaced tibial and fibular fractures who was referred from skilled nursing facility to Emergency Department for evaluation of dehydration, hyperkalemia and worsening of mental status. Patient was found hypotensive and hypoxic. Severe sepsis was suspected and patient was resuscitated with intravenous fluid. On physical examination, abdomen was distended and tender with no bowel sounds. Figures 1-3 show hepatic portal venous gas (HPVG), pneumatosis intestinalis (PI) indicated by intestinal submucosal gas, and sever atherosclerotic calcification of the aorta at the same time on computed tomography (CT).
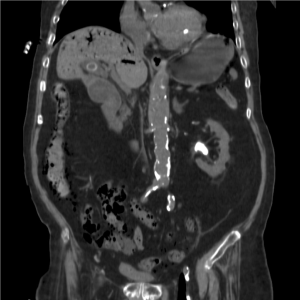
The patient clinical condition was too critical to be stabilized by surgical intervention, and eventually he died of septic shock. PI is most commonly developed as a result of bowel ischemia and mesenteric infarction, but might be the result of various non-ischemic conditions like trauma, infection, inflammation, obstruction, neoplasm, iatrogenic and idiopathic causes (1). Presence of PI and HPVG at the same time is an important radiological sign, since it usually shows portentous abdominal pathology (2). Advanced imaging techniques such as CT have increased the sensitivity for detection. CT has allowed visualization of small amounts of intraabdominal air that could not be seen at conventional abdominal radiography, and effectively reveals PI and HPVG earlier which results in early intervention and increased likelihood of survival (3,4).
The presence of severe abdominal aorta atherosclerosis in this patient might be an indicator of mesenteric atherosclerotic disease and ischemia, which is common in the elderly population. Such an ischemic condition could turn into angina or infarction by acute arterial occlusion due to emboli, specifically originated from unstable atherosclerotic plaques.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wayne E, Ough M, Wu A, et al. Management algorithm for pneumatosis intestinalis and portal venous gas: treatment and outcome of 88 consecutive cases. J Gastrointest Surg 2010;14:437-48. [PubMed]
- Wiesner W, Mortelé KJ, Glickman JN, et al. Pneumatosis intestinalis and portomesenteric venous gas in intestinal ischemia: correlation of CT findings with severity of ischemia and clinical outcome. AJR Am J Roentgenol 2001;177:1319-23. [PubMed]
- Sebastià C, Quiroga S, Espin E, et al. Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. Radiographics 2000;20:1213-24; discussion 1224-6. [PubMed]
- Kernagis LY, Levine MS, Jacobs JE. Pneumatosis intestinalis in patients with ischemia: correlation of CT findings with viability of the bowel. AJR Am J Roentgenol 2003;180:733-6. [PubMed]