An abdominal desmoid-type fibromatosis
A 31-year-old male presented with a palpable abdominal mass discovered by himself incidentally without any symptoms. He has no previous systemic disease. Physical examination revealed a large and firm mass in lower abdomen without tenderness. Laboratory test was not remarkable.
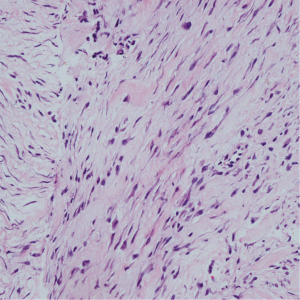
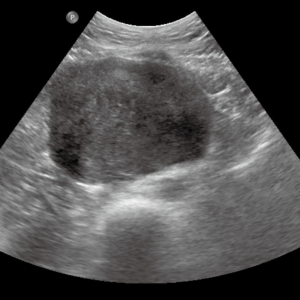
The ultrasound machine used in this study was a Philips iU22 unit (Philips, Bothell, WA). Sonography of the abdomen showed an ovoid, well-defined, mobile mass in the mid and lower abdominal regions, surrounded by bowel loops. The mass had a heterogeneous hypoechoic texture, and no calcifications and cystic area were noted (Figure 1). Color Doppler Flow Imaging (CDFI) detected no blood flow. There was no enlarged lymph node or ascites. Magnetic resonance (MR) imaging revealed a 7 cm × 10 cm mass arising from the mesentery, with intermediate signal intensity on T1-weighted images (Figure 2A), heterogeneous intermediate and high signal intensity on T2-weighted images (Figure 2B) and restricted diffusion on diffusion-weighted MR imaging (DWI). These imaging findings suggested a mesenteric neoplasm, likely a gastrointestinal stromal tumor (GIST) or lymphoma.
To avoid sampling of necrosis tissue which might lead to an inconclusive diagnosis, contrast enhanced ultrasound (CEUS) guided core biopsy was performed (MI 0.08-0.11) with 2.4 mL contrast agent (Bracco Sonovue) administrated through a forearm vein. The ultrasound machine used in CEUS was an Aloka ProSound Alpha 10 unit (Aloka, Japan). The whole tumor showed markedly inhomogeneous enhancement from 12 s after injection, achieving the maximum enhancement at approximately 20 s, and then contrast agent was washed out gradually since 27 s (Video 1). Tissue specimens were taken from enhanced region and non-enhanced region separately to get a diagnosis and explore the correlation between contrast enhancement pattern and histopathology.
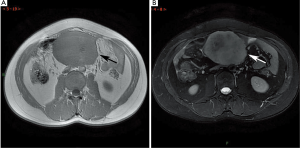
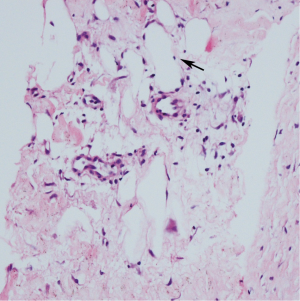
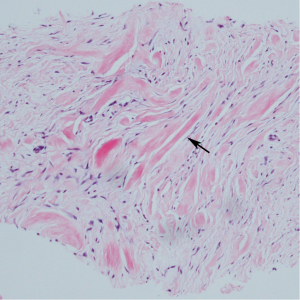
Microscopically, the tumor was mainly composed of spindle-shaped cells of fibroblasts and striated muscle cells in abundant collagen stroma (Figure 3), with keloid-like collagen deposition identified (Figure 4). Enhanced region showed more prominent vascularity compared to the non-enhanced region (Figure 5), but the degree and distribution pattern of high cellularity areas and collagenous stroma was indifferent in two tissue specimens. Immunohistochemically, the spindle cells were positive for viementin, SMA and Bcl-2, and negative for S100, Actin, Desmin and CD34. These results were consistent with desmoid-type fibromatosis. Surgery was performed. Laparotomy revealed a large solid mass about 10 cm × 10 cm located at the root of mesentery. The mass was excised totally. Grossly, the mass was firm, gray-white colored without distinct capsule and had a wave-like appearance. No hemorrhage and necrosis was seen.
Desmoid-type fibromatosis was a rare slow growing benign and musculoaponeurotic tumor. According to the literature, the imaging features of desmoid-type fibromatosis on CT and MR are related to various proportions and distribution of collagen and fibroblast content within the lesion. In this case, the enhancement with CEUS reflected the degree of vascularity in the tumor, but not correlated with the histopathologic character. It is noteworthy that there is no cystic change in the tumor, whereas GIST typically demonstrated with hemorrhage and necrosis, which may help to suggest the differential diagnosis.
Acknowledgements
This study was supported by Beijing Municipal Science & Technology Commission No. Z131107002213016 and Beijing Hope Run Special Fund of China Cancer Research Foundation (CCRF) No. LC2013A04.
Disclosure: The authors declare no conflict of interest.