
Justification of whole-body CT in polytrauma patients, can clinical examination help selecting patients?
Introduction
The use of whole-body computed tomography (WBCT) is advocated for rapid and comprehensive objective diagnosis of serious injuries. The proponents of WBCT justify it use due to its potential benefit in detecting unsuspected life-threatening injuries.
Nevertheless, its use is questionable in seemingly normal patients just to allow for an early emergency department (ED) discharge. Furthermore, the risk of developing Radiation-induced cancer can’t be denied particularly in young patients exposed to high dose radiation as is the case in WBCT. We share our experience on this controversial topic and sincerely hope that with increase in the number of published studies on this topic, proper guidelines for use of WBCT in early management of polytrauma patients can be formulated.
The European injury database (IDB) 2014 report mentioned hospital treatment of around 40 million people who had suffered accidents (in all sectors including transport, workplace and school) on an annual basis with deaths reported in 233,000 cases (1). The latest diagnostic imaging dataset statistical release by NHS, England, mentioned approximately 0.38 million total CT scan examinations performed every month in United Kingdom, with no particular reference of polytrauma WBCT figures (2). Sammy et al. published retrospective observational study of Trauma Audit and Research Network (TARN) data from 2012–2014 and reported WBCTs in 16.5% of polytrauma patients with more scans being done in major trauma centres than non-designated hospitals (3). With the advent of major trauma centers across the UK many patients are transferred to CT after initial assessment with targets in place for this scan to be done in a relatively short time window (4).
For a large number of patients, there is no controversy as to whether WBCT should be included as part of their management and most centers have a Radiology proforma with specific requesting criteria, to ensure that the examination is justified. However, there is a seemingly increasing number of patients who appear to fulfil these criteria for WBCT, and in whom the study turns out to be normal with no trauma related pathology. This is of course highly useful in managing the patient, but the justification for scans in these patients becomes a more complicated issue. Also it is being reported that, 1–3% cancers worldwide are caused by medical sources of radiation (5,6).
WBCT on an average exposes each patient to more than 20 mSv of effective radiation dose which increases the risk of cancer mortality of 1 in 900 with radiation dose of 24 mSv in 35-year-old male and 1 in 1,250 with radiation dose of 10–20 mSv in average 45-year adult patient (7-9). Keeping these statistics in perspective, it becomes the responsibility of the medical fraternity to limit the use of whole-body CT in polytrauma patients and proper guidelines regarding the same need to be established. Our study is a step forward in achieving the same.
Methods
This study was performed in a tertiary care major trauma center in north England, as a retrospective database analysis of 150 polytrauma cases, who underwent WBCT from August 2017 to December 2017. All the trauma patients were initially managed in line with advanced trauma life support (ATLS) protocol of the hospital and the decision to proceed for whole-body CT scan was taken by the trauma team Consultant/Senior Registrar based on the indications as mentioned in Table 1.
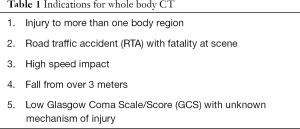
Full table
Informed patient consent were taken during the time of the scan. All the scans were performed on a Siemens Somatom sensation 40 multislice scanner, using Bastion protocol with biphasic contrast injection with the scan triggering at 60 seconds while the contrast is still flowing in.
We recorded age, gender, mechanism of injury, clinical requests and concerned raised, WBCT findings in seven regions of head (including face), cervical spine, thoracolumbar spine, chest, abdomen, pelvis and appendicular skeleton injuries (if asked for) as per our institutional reporting protocol. Dose length product (DLP) of each patient scanned recorded at the end of examination was converted to effective dose using standard recommended formula of multiplying DLP with 0.013 to produce effective dose (ED) in millisievert (10,11).
We compared pre-test clinical requests stating mechanism of injury and clinical query with WBCT findings and categorized the patients in seven categories: Category 1: Normal Scans; Category 2: Clinically expected Major Injuries; Category 3: Clinically expected Minor Injuries (low risk injuries with no risk of morbidity or mortality if remained undiagnosed) with rest of negative scan; Category 4: Clinically expected CT findings with Unexpected Minor (non-serious) Injuries; Category 5: Clinically expected CT findings with Unexpected Major (serious) injuries; Category 6: Unexpected Minor (non-serious) Injuries; Category 7: Unexpected Major (serious) injuries. Categories 2 & 3 of clinically expected major and minor injuries included patients with fewer injuries than expected. Total numbers in each category were calculated and inferences discussed. Also the mean radiation dose in scans with normal findings and scans with positive CT findings was calculated.
Results
On analysis of data related to indications for WBCT in our study, we found 61 patients being referred for WBCT due to fall from height (commonest reason being fall from stairs). Thirty-nine and 36 patients had road traffic accident and high speed impact respectively, while 8 patients presented with injury to more than one body region and 6 presented with low GC Scale with unknown mechanism of injury. The results were tabulated as depicted in the Table 2.
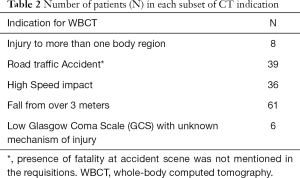
Full table
Based on the clinical suspicion raised and WBCT findings, patients were divided in seven categories as shown in Table 3. Out of 150 patients included in the study, WBCT scans were positive in 104 cases while 46 patients (30.67%) had normal scans, with no trauma related pathology. Clinically expected major and minor injuries were seen in 61 (40.67%) and 20 (13.33%) patients respectively. Out of the total 46 normal scans, 25 requisitions were made just on the basis of mechanism of injury, and no obvious clinical concerns were raised. Sixteen (10.67%) cases had a mix of expected CT findings, coexisting with unexpected findings, which included 5 (3.33%) cases of unexpected major (serious) injuries, and eleven cases of unexpected minor injuries. Clinically unexpected injuries were seen in 7 (4.67%) cases of which 1 (0.67%) was serious case of fracture of body of sternum. Six (4%) patients had unexpected minor/subtle injuries, which included isolated cases of superficial soft tissue haematomas, small subgaleal haematoma with no intracranial injuries, rib fractures with no flail chest or intrathoracic injuries and transverse process fractures with the remainder of the scan being negative.
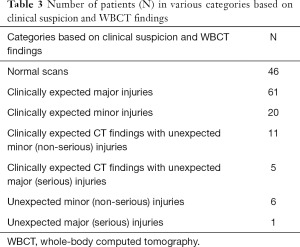
Full table
Table 4 shows number of patients sent for each indication under various categories. There is no statistical association between the indication and expected CT findings with p value of 0.697 (Chi-square: 19.981; degrees of freedom: 24; P value: 0.69785613; Yates' Chi-square: 20.741; Yates' P value: 0.65395327).
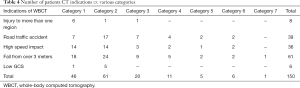
Full table
However, we realized that most of normal scans, on basis of percentage (6/8=75%) were seen in patients sent for WBCT with indication of injury to more than one region, and highest percentage (5/6=83%) of clinically expected major injuries were seen in patients sent with low Glasgow coma scale/score. No unexpected major or minor injuries were seen in both these indication subgroups.
Further, the data was analysed based on the clinical suspicion of various types of injuries and CT findings (Table 5).

Full table
Bivariate statistical analysis was done with chi square test, which showed statistical significance with p value less than 0.001 (chi-square: 31.993; degrees of freedom: 2; P value<0.001). One hundred six patients out of 150 showed WBCT results as clinically expected. Overall, mean age of the total number of patients was 49.18 years and that of patients with a normal scan was 45.2 years. Mean radiation dose for the entire study group was 22.45 mSv and that for normal patients study group was 21.19 mSv. There were 29 and 11 patients of less than 25 years in the entire study group and normal study group respectively. Among the clinically expected injuries, 30 cases (20%) of clinically expected major and minor injuries (with no unexpected injuries) with very good correlation with the history and physical examination findings, only limited CT scan instead of WBCT would have sufficed.
Surprisingly, 25 (16%) scans were requested due to high risk mechanism of injury without any obvious clinical concern, which were normal. thus again signifying the importance of clinical evaluation before raising the request for whole-body CT.
Discussion
The evidence given by Huber-Wagner et al. in their published paper was overwhelmingly convincing for the inclusion of whole-body CT in the pathway of multiple injured patients, as it is found beneficial in improving outcome and is therefore part of standard protocol for workup in these patients (12). However, the study had several limitations and most important being preselection of high risk patients with suspicion of severe injuries, who mostly benefitted from CT scanning, as also in our study, where there was statistically significant association found in patients suspected of major injury and final WBCT outcome (8).
We compared our results with previous published studies. High clinical correlation in our study was seen in 70.66% of the cases, which was comparable to the results of Linder et al. who stratified patients in three groups based on clinical examination as high risk, intermediate risk and low risk with positive WBCT seen in 74.5%, 44.8% and 0% of cases in three groups respectively. The authors recommended observation with re-examination in mentally alert patients, who suffered with high-energy trauma with no features of intoxication or major injuries on clinical examination (9). Long et al. also reported no mortality benefit with routine use of WBCT in comparison to organ selective imaging in their randomized controlled trial and suggested adoption of selective imaging strategy by emergency clinicians driven by history and physical examination (13). In our study, we realised the fallacy of referring patients only on fixed indications based on protocol, as 25 (16%) scans, were requested due to high risk mechanism of injury without any obvious clinical concerns and all of these turned out normal. Also, in-depth analysis revealed, that in patients with indication of ‘injury to more than one region of body’, 4 out of 6 patients with normal study gave history of alleged assault with good GCS. No unexpected major or minor injuries were seen in this subgroup, hence WBCT in these patients could have been avoided by doing good clinical examination or keeping them under supervision. We also found, highest percentage (5/6=83%) of clinically expected major injuries in patients sent with indication of ‘low Glasgow coma scale/score’.
Davies et al. also proposed use of clinical scoring system based on clinical signs of trauma to more than one body region, Glasgow Coma Scale, haemodynamic abnormality, respiratory abnormality and mechanism of injury (14), however, forming a clinical score was not one of the objective of our study. There are several studies, which have also suggested use of clinical prediction rules to safely omit unnecessary WBCTs reducing radiation dose and cost (15-17).
Contrastingly, Shannon et al. reported poor correlation of clinical findings with WBCT findings and the discrepancy is likely due to inclusion of fewer injuries than expected as a separate category. Additionally, they also mentioned clinical discordance in cases where there were more injuries than expected, whereas, the use of CT in patients with both expected and unexpected injuries was justified in our study due to clinical signs of injury to more than one body part in most of these patients (18).
By incorporating findings of thorough clinical examination, we can not only prevent unnecessary WBCT examinations done in polytrauma cases, but also prevent radiation exposure to the tune of approximately 20 millisieverts to many patients.
Limitations of our study included: small sample size; the possibility that we may have overestimated the clinical correlation cannot be ruled out; patients with fewer injuries than expected were not separately categorized; and no follow-up of patients.
Conclusions
In our study, 106 out of 150 (70.7%) patients showed clinically expected WBCT findings. The association between clinical expectation/concern raised and the WBCT findings was statistically significant in patients suspected of major injuries. There was no statistical association between the indications of CT and CT outcome. Hence, caution should be exercised in advising WBCT to polytrauma patients just on the basis of mechanism of injury and without any real clinical concerns, as seen in 25 (16.7%) patients with normal WBCT findings in our study. Therefore, good clinical examination can obviate the need of WBCT in many suspected polytrauma patients resulting in reduction of number of unnecessary normal CT examinations, thereby preventing high radiation exposure and its potential side effects to the patients. We recommend revision of whole-body CT indications in suspected polytrauma patients with inclusion of positive clinical examination findings in all categories irrespective of mechanism of injury, although, further studies are recommended for framing universal guidelines. In addition, we recommend regular feedback of WBCT findings to ED Consultants in order to update their selection of patients for WBCT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was done in line with Ethical committee guidelines of the hospital.
References
- Bauer R, Steiner M, Kisser R, Macey SM, Thayer D. Accidents and injuries in the EU. Results of the EuroSafe Reports. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2014;57:673-80. [Crossref] [PubMed]
- . Available online: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2018/06/Provisional-Monthly-Diagnostic-Imaging-Dataset-Statistics-2018-06-21.pdfDiagnostic Imaging Dataset Statistical Release.
- Sammy IA, Chatha H, Bouamra O, Fragoso-Iñiguez M, Lecky F, Edwards A. The use of whole-body computed tomography in major trauma: variations in practice in UK trauma hospitals. Emerg Med J 2017;34:647-52. [Crossref] [PubMed]
- Standards of practice and guidnce for trauma radiology in severely injured patients. Available online: https://www.rcr.ac.uk/sites/default/files/docs/radiology/pdf/BFCR(11)3_trauma.pdf
- Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004;363:345-51. [Crossref] [PubMed]
- Brenner DJ, Hall EJ. Computed Tomography — An Increasing Source of Radiation Exposure. N Engl J Med 2007;357:2277-84. [Crossref] [PubMed]
- Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology 2004;232:735-8. [Crossref] [PubMed]
- Wutzler S, Marzi I. Routine total-body CT for trauma room patients—life saver or needless radiation exposure? J Thorac Dis 2016;8:3040-1. [Crossref] [PubMed]
- Linder F, Mani K, Juhlin C, Eklöf H. Routine whole body CT of high energy trauma patients leads to excessive radiation exposure. Scand J Trauma Resusc Emerg Med 2016;24:7. [Crossref] [PubMed]
- Inoue Y, Nagahara K, Tanaka Y, Miyatake H, Hata H, Hara T. Methods of CT Dose Estimation in Whole-Body 18F-FDG PET/CT. J Nucl Med 2015;56:695-700. [Crossref] [PubMed]
- Huda W, Ogden KM, Khorasani MR. Converting Dose-Length Product to Effective Dose at CT. Radiology 2008;248:995-1003. [Crossref] [PubMed]
- Huber-Wagner S, Lefering R, Qvick LM, Körner M, Kay MV, Pfeifer KJ, Reiser M, Mutschler W, Kanz KG. Working Group on Polytrauma of the German Trauma Society. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet 2009;373:1455-61. [Crossref] [PubMed]
- Long B, April MD, Summers S, Koyfman A. A Whole body CT versus selective radiological imaging strategy in trauma: an evidence-based clinical review. Am J Emerg Med 2017;35:1356-62. [Crossref] [PubMed]
- Davies RM, Scrimshire AB, Sweetman L, Anderton MJ, Holt EM. A decision tool for whole-body CT in major trauma that safely reduces unnecessary scanning and associated radiation risks: An initial exploratory analysis. Injury 2016;47:43-9. [Crossref] [PubMed]
- Kendall JL, Kestler AM, Whitaker KT, Adkisson MM, Haukoos JS. Blunt abdominal trauma patients are at very low risk for intra-abdominal injury after emergency department observation. West J Emerg Med 2011;12:496-504. [Crossref] [PubMed]
- Corwin MT, Sheen L, Kuramoto A, Lamba R, Parthasarathy S, Holmes JF. Utilization of a clinical prediction rule for abdominal-pelvic CT scans in patients with blunt abdominal trauma. Emerg Radiol 2014;21:571-6. [Crossref] [PubMed]
- Mahoney E, Agarwal S, Li B, Dechert T, Abbensetts J, Glantz A, Sherburne A, Kurian D, Burke P. Evidence-based guidelines are equivalent to a liberal computed tomography scan protocol for initial patient evaluation but are associated with decreased computed tomography scan use, cost, and radiation exposure. J Trauma Acute Care Surg 2012;73:573-8. [Crossref] [PubMed]
- Shannon L, Peachey T, Skipper N, Adiotomre E, Chopra A, Marappan B, Kotnis N. Comparison of clinically suspected injuries with injuries detected at whole-body CT in suspected multi-trauma victims. Clin Radiol 2015;70:1205-11. [Crossref] [PubMed]


