Integrated application of antegrade and retrograde recanalization for femoral-popliteal artery chronic total occlusions: outcomes compared with antegrade recanalization
Introduction
Endovascular recanalization is widely preferred for treatment of femoral-popliteal [superficial femoral artery (SFA) and/or proximal popliteal artery (PA)] chronic total occlusion (CTO) because it causes minimal trauma, has few postoperative complications, and has accepted clinical efficacy (1). However, occlusion length, calcification degree, operator experience, and runoff status influence the results of the procedure. Technical failure is still seen in approximately 20% of cases, mainly due to failure to re-enter into arterial true lumen (2). The utility of new devices and a number of different of advanced guide wires, which are specially developed for CTO recanalization, have improved the success rate of endovascular treatment, but it is still technically challenging in some cases. To achieve a satisfactory success rate, shorten operation time, reduce contrast agent dose, and decrease complications, the operator needs to be familiar with different recanalization techniques, including antegrade and retrograde techniques. Antegrade techniques are as following: parallel wire, see-saw, and contralateral wire techniques, and the subintimal tracking and re-entry (STAR) technique, while the commonly employed retrograde techniques include the controlled antegrade and retrograde tracking and dissection (CART) technique, the rendezvous technique, and the bidirectional balloon dilation technique. The application of these techniques has been reported in various studies, but most reports have focused on only one kind of technique (3-6). There is a lack of study about comprehensive analysis of integrated application of antegrade and retrograde techniques for achieving recanalization of femoral-popliteal CTOs, no results compared integrated recanalization with antegrade recanalization either in term of clinical outcomes, vascular restenosis rate, and limb salvage rate. In this retrospective study, we investigate the feasibility and efficacy of integrated antegrade and retrograde recanalization techniques in patients with femoral-popliteal CTOs.
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of our hospital. All patients provided written informed consent for the endovascular procedure. We retrospectively reviewed all lower extremity endovascular procedures performed for the treatment of peripheral arterial disease at our center from June 2011 to October 2014. All patients who had received treatment for femoral-popliteal CTOs (n=205) were included in the study; there were a total of 238 CTOs in these patients. Baseline, preoperative and postoperative data of all patients were retrospectively collected from the case records. All patients underwent detailed examination, including clinical and radiologic evaluation; the dorsal/plantar arterial pulse scores and ankle-brachial index (ABI) were recorded, and lower extremity arterial ultrasonography or computed tomography angiography (CTA) was performed. Indications of arterial occlusion were (I) ABI <0.9 (without severe arterial calcification); (II) reduced or absent dorsal/plantar arterial pulse; and (III) vessel occlusion of femoral-popliteal artery displayed by lower extremity CTA or arterial ultrasonography. And digital subtraction angiography (DSA, Artis zee, Siemens Medical Solutions, Erlangen, Germany) was performed to further assess the vascular condition, followed by subsequent angioplasty if necessary. DSA series was obtained from the distal abdominal aorta down to the level of the ankles by injecting 7 mL contrast at 4 mL/s.
Recanalization procedures
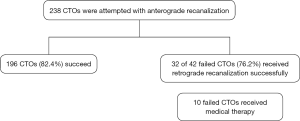
Patients received aspirin (100 mg) and clopidogrel (75 mg) 3 days before the procedure if stent placement was planned. Recanalization procedures were performed in a modern Angio room, consisted of a patient support table, equipment for monitoring blood pressure and the electrocardiograph, and a ceiling suspended frame that allows variable angulation of the X-ray through the patient. Endovascular recanalization for femoral-popliteal artery CTO was performed under local anesthesia. The patient was placed in the supine position; access to the SFA lesion was achieved via the contralateral or ipsilateral femoral artery. A 4F vertebral catheter (Cook, Bloomington, IN, USA) was inserted through a 6F introducer, and baseline diagnostic angiography was performed using an iodinated contrast agent. Antegrade recanalization was attempted firstly, and either intraluminal or subintimal recanalization was performed, depending on CTO length, occlusion and calcification degree. If antegrade angioplasty failed, then retrograde recanalization was attempted (Figure 1).
Antegrade recanalization
When antegrade intraluminal angioplasty was performed, the initial approach was attempted by using a 0.035-, 0.018-, or 0.014-inch hydrophilic guidewire (Terumo, Tokyo, Japan; V18 or PT2, Boston Scientific, Boston, MA, USA) passed through a 4F catheter (Cook Medical Inc., Bloomington, IN, USA) or a microcatheter (TrailBlazer™ Support Catheter; Ev3 Endovascular Inc., Plymouth, MN, USA). In particular, as the sliding technique (7), the hydrophilic guidewire could advance with minimal resistance with the potential risk of inadvertent straying into the subintimal space, and could be suitable for the engagement of recanalized microchannels or subtotal occlusions.
If the guidewire entered into the subintimal space, STAR recanalization was attempted. Under this circumstance, a “U”-shaped loop was created at the tip of the guidewire and it was advanced steadily in the subintimal dissection until it re-entered the true lumen beyond the occlusion.
Retrograde recanalization
If the guidewire failed to pass through the CTO lesion or failed to re-enter the true lumen by the antegrade technique, then retrograde recanalization was considered. The retrograde approach was performed only after the diagnostic angiogram was reviewed by at least two experienced interventional radiologists; the criteria for selecting retrograde angioplasty were: (I) presence of good distal runoffs, with prospects for good patency of the CTO after recanalization, and (II) inadequacy of effluent collaterals supplying blood to distal ischemic areas. When the retrograde recanalization was attempted, the patient was kept in the supine position with the target leg in a 60° external rotation. Angiogram via the proximal sheath was performed to display the appropriate level for retrograde puncture. The puncture site was determined 8–10 cm below the distal end of CTO. A 21-G micro-puncture needle (Cook Medical Inc., Bloomington, IN, USA) was used to puncture, obliquely from caudal to cranial. When access was obtained within the true lumen, a 0.018-, or 0.014-inch hydrophilic guidewire (V18 or PT2, Boston Scientific, Boston, USA) was inserted, and the needle was pulled out. Next, a 4-F sheath was inserted, and then a successful retrograde vascular access was established.
Controlled antegrade and retrograde tracking and dissection (CART) technique
For the CART technique, a guidewire was introduced antegrade from the proximate cap of the CTO and advanced into the subintimal space. The subintimal channel was then enlarged by advancing a looped guidewire or by inflating an antegrade balloon (Admiral Xtreme; Invatec, Brescia, Italy or POWERFLEX® Pro; Cordis, Bridgewater, NJ, USA) to create a plaque dissection and modify the lesion. After that, the wire was introduced via the retrograde puncture access and advanced in the subintimal space of the CTO lesion. After confirming that the retrograde wire had crossed the dissection and linked up with the antegrade wire positioned in the proximal true lumen, all subsequent procedures were performed in the retrograde fashion.
Rendezvous technique
When the retrograde wire was advanced into the subintimal space and unable to return to the true lumen, rendezvous technique would be attempted. Briefly rendezvous technique was attempted as follows: (I) two 4-F vertebral catheters (Cook Medical Inc., Bloomington, IN, USA) or a 4-F catheter and a micro-catheter were placed into the antegrade and retrograde subintimal lumen respectively and iodinated contrast agent was injected through the 4-F catheter gently to find out if there was any other channel through which the guide wire could pass; (II) the two catheters would be advanced to the site, and their heads would be manipulated to be as close to each other as possible; (III) a 0.035- or 0.018-inch hydrophilic guide wire was attempted to pass from the catheter located in the retrograde subintimal lumen to the catheter in the antegrade subintimal lumen. Once the retrograde wire entered the antegrade catheter, the antegrade catheter would be advanced across the occluded artery with support from the retrograde wire and catheter.
Bidirectional balloon angioplasty technique
If the antegrade and retrograde subintimal false channels were parallel and no intersections existed, bidirectional balloon dilation (Admiral Xtreme; Invatec, Brescia, Italy or POWERFLEX® Pro; Cordis, Bridgewater, NJ, USA) would be performed to enlarge the subintimal space to boost subsequent CART or rendezvous technique.
After successful recanalization of the CTO, using either the antegrade or retrograde method, contrast was injected to confirm that the catheter was in the true lumen of distal artery. A 260-cm guidewire was then exchanged to perform the subsequent procedures in an antegrade manner. Balloon angioplasty (Admiral Xtreme; Invatec, Brescia, Italy or POWERFLEX® Pro; Cordis, Bridgewater, NJ, USA) was advanced through the antegrade approach, and self-expandable stents (Protégé™ EverFlex™; Invatec, Brescia, Italy or S.M.A.R.T.® CONTROLTM; Cordis, Bridgewater, NJ, USA) were implanted for correction of flow-limiting dissection or >30% residual stenosis. The procedure was considered successful if angiography revealed <30% residual stenosis of the recanalized segment. Upon completion of the procedure, for patients with retrograde puncture, a guide-wire and balloon catheter (Admiral Xtreme; Invatec, Brescia, Italy or POWERFLEX® Pro; Cordis, Bridgewater, NJ, USA) was moved into the punctured artery and dilated with the distal sheath was withdrawn. The puncture site would be compressed manually until hemostasis was accomplished. The balloon was then removed, and the patency of the artery access site was confirmed by angiography. After the procedure, the distal access site was covered with a standard circular bandage for 4 hours. The post intervention regime included dual antiplatelet therapy with aspirin (100 mg/d) and clopidogrel (75 g/d) for at least 3 months and lifelong aspirin (100 mg/d).
Outcome evaluation and definitions
Modified thrombolysis in myocardial ischemia (mTIMI) flow grades was used to assess the blood flow through the recanalized artery and distal tissue reperfusion post-procedure immediately as follows (8): mTIMI 0 (no perfusion): absence of any antegrade flow beyond the occlusive artey; mTIMI 1 (penetration without perfusion): faint antegrade flow beyond the occlusive artey, with incomplete filling of the distal territory; mTIMI 2 (partial reperfusion): delayed antegrade flow, with complete filling of the distal territory; and mTIMI 3 (complete perfusion): normal flow that filled the distal territory completely. Improvement of ABI and pulse volume score was also used as subjective indicators to assess the immediate outcome of the procedure. Pulse volume score was graded on a scale from 0 to 3, where 0: no pulse palpated; 1: low grade pulse; 2: middle grade pulse; and 3: normal pulse.
Follow-up protocol
Arterial duplex sonography or lower limb CTA was used to monitor target lesion patency during follow-up. In those who had arterial restenosis or recurrent ischemic symptoms, DSA was performed and reintervention attempted if necessary. Restenosis or reocclusion was recorded. Patency was defined as <50% stenosis in the target vessel. Pulse volume score, ABI, clinical symptoms improvement, and limb salvage were assessed at each follow-up visit. Decrease in ulceration size by more than 50% was considered as an improvement. Above-ankle amputation was considered as a failure of limb salvage.
Statistical analysis
SPSS version 20.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. The grouped t test was used to compare ABI before and after treatment. Rutherford score, mTIMI flow grade, and pulse score before and after treatment were compared using the Mann-Whitney U test. The Kaplan-Meier method was used to calculate the primary patency rate and limb salvage rate over time. Two-sided P≤0.05 indicated the statistical significance.
Results
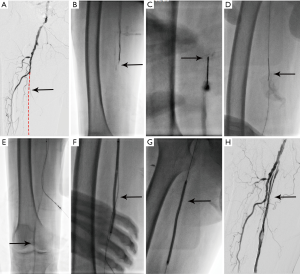
Between June 2011 to October 2014, 205 patients with 238 femoral-popliteal CTOs were attempted with endovascular recanalization at our centre. Successful recanalization was achieved in 228 of the 238 CTOs—a success rate of 95.8%. Antegrade recanalization was successful in 196 CTOs (intraluminal angioplasty in 76 and subintimal angioplasty in 120)—a primary technical success rate of 82.4% (196/238). Of the 42 cases where the antegrade technique failed, 32 were successfully recanalized by the retrograde technique: 6 cases by retrograde intraluminal recanalization, 10 by the CART technique, 10 by the rendezvous technique, and 6 by the bidirectional balloon technique. Table 1 shows the general condition and clinical data of the patients who received successful recanalization. For retrograde puncture access, direct SFA puncture was used in 13 cases, PA puncture in 6, and anterior tibial artery puncture in 13 (Figures 2,3). The average lengths of the CTOs treated successfully with antegrade and retrograde recanalization were 9.3±5.5 and 18.5±6.4 cm, respectively (P<0.001). A mean number of 1.6±0.7 stents were placed in the femoral-popliteal arteries in the 228 CTOs (one stent in 78 limbs, two stents in 134 limbs, and three stents in 16 limbs), and the mean diameter of stents used was 5.79±0.41 mm. In addition, 41 patients received concurrent infrapopliteal endovascular recanalization. The integrated antegrade and retrograde approach failed to achieve recanalization in 7 CTOs. One patient had had the history of cerebral infarction and another could not tolerate a lengthy procedure due to joint deformities; in these patients, the procedure was discontinued just after retrograde puncture was performed. In the other 8 CTOs, retrograde puncture failed due to poor distal runoff vessels.
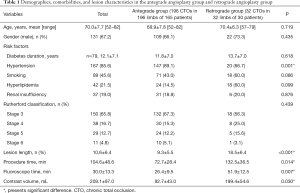
Full table

No life-threatening complication occurred during any of the procedures. Procedure-related complications occurred in 19 (8.3%) CTOs (14 CTOs in the antegrade group vs. 5 CTOs in the retrograde group, P=0.091). Distal embolism occurred in 11 CTOs (9 in antegrade group and 2 in the retrograde group); of these, 3 patients were managed by urokinase infusion (500,000 IU), and the other 8 by urokinase infusion (500,000 IU) plus thrombus aspiration using a 6F guiding catheter. Local hematoma at the puncture site occurred in 5 patients: in 2 patients at the antegrade puncture site and in 3 patients at the retrograde puncture site. Dissections occurred in 3 patients in antegrade group, and were treated with repeated balloon dilation or remedial stent implantation.
Immediate outcome and follow-up
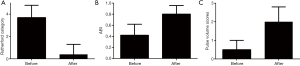
Angiography immediately after the procedure in all successfully recanalized CTOs showed mTIMI grade 2 blood flow in 59 CTOs and grade 3 blood flow in 169 CTOs. The median, first and third quartiles of mTIMI flow grade before treatment were 1, 1, 2 and all of them after treatment was 3. The mean mTIMI score increased from 1.4±0.5 before the procedure to 2.9±0.3 after the procedure (P<0.001); the change was from 1.4±0.5 to 2.9±0.3 in the antegrade group and from 1.3±0.4 to 2.9±0.2 in the retrograde group (P=0.09). The median, first and third quartiles of Rutherford score before were 3, 3, 4 and all of them after the treatment was 0. The mean Rutherford score improved from 3.7±1.1 before the procedure to 0.4±0.8 after the procedure (P<0.001); the change was from 3.6±1.1 to 0.2±0.6 in antegrade group and from 4.5±0.1 to 1.0±1.1 in the retrograde group; P=0.459. The mean ABI increased from 0.47±0.18 before the procedure to 0.78±0.15 after the procedure (P<0.001); the change was from 0.48±0.18 to 0.79±0.16 in antegrade group and from 0.41±0.13 to 0.76±0.13 in the retrograde group; P=0.438. The median, first and third quartiles of pulse score before and after treatment were 0, 0, 1 and 2, 2, 3. Mean dorsal/plantar arterial pulse scores increased from 0.46±0.49 before the procedure to 2.28±0.76 after the procedure (P<0.001); the change was from 0.48±0.50 to 2.30±0.76 in the antegrade group and from 0.48±0.51 to 2.30±0.79 in the retrograde group; P=0.771; Figure 4).
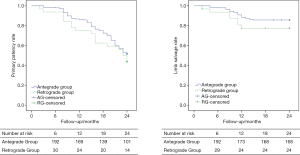
Follow-up data were available for all 228 successfully treated CTOs (arterial duplex sonography in 132 patients with 158 CTOs) and lower limb CTA in 63 patients with 70 CTOs). Primary patency rate at 6, 12, and 24 months after angioplasty was 98.0% (192/196), 86.2% (169/196), and 51.5% (101/196) in the antegrade group and 93.8% (30/32), 75.0% (24/32), and 43.8% (14/32) in the retrograde group, respectively; the differences were not statistically significant (log rank test; P=0.346; Figure 5). According to the lower limb CTA images (63 patients with 70 CTOs), in a stent-based analysis, 13 of 70 stents (18.6%) showed fractures (2 cases in the CTO with one stent, 4 cases in the CTO with two stents and 7 cases in the CTO with three stents). A second intervention was performed in 60 of the 95 patients who had reocclusion in the antegrade group and in 12 of the 18 patients with reocclusion in the retrograde group. Among the 38 patients with rest pain, pain relief was achieved and analgesia discontinued in 35 patients. Of the 29 patients with tissue loss, complete healing was achieved in 20 patients; improvement was seen in 5 patients. Planned minor amputations were performed in 4 patients immediately after the interventional procedure because of irreversible gangrene. Above-ankle amputation was performed in 29 patients and above-knee in 6 patients during the follow-up. Limb salvage rates were 98.0% (192/196), 88.3% (173/196), and 85.7% (168/196) in the antegrade group and 93.8% (30/32), 78.1% (25/32), and 78.1% (25/32) in the retrograde group at 6, 12, and 24 months, respectively (log rank test; P=0.198; Figure 5).
Discussion
The aim of this study was to assess the efficacy of integrated antegrade and retrograde recanalization techniques applied for femoral-popliteal CTOs in patients. The primary technical success rate of antegrade recanalization was 82.4%, which is similar to other published reports (82–100%) (2,9-11). However, when it was combined with the retrograde recanalization strategy, the success rate increased to 95.8%. The main reason for recanalization failure in this study was the lack of an appropriate access site for retrograde puncture because of poor distal runoff. At the end of follow-up (24 months), the patency rate and limb salvage rate were 43.8% and 78.1% respectively in the integrated group, which is similar to previous reports (9,11). These Figures suggest that integrated application of antegrade and retrograde recanalization is an effective method for femoral-popliteal CTO recanalization.
The prevalence of atherosclerosis, diabetes, and hyperlipidemia has been rising in China due to population and changing of the dietary constitutes in China (12), which resulted in more peripheral arterial occlusive diseases. Although bypass surgery provides good long-term patency of treated arteries in patients with peripheral arterial occlusive diseases (13), endovascular treatment for obstructive lesions of the SFA is less invasive and has been effective, but can be challenging in the presence of severe calcification and poor runoff, when the technical failure rate is as high as 28% (1,2,14). Retrograde recanalization has generally been considered a supplementary technique. The rationale underlying retrograde recanalization is that the distal fibrous cap of the CTO is less rigid than the proximal fibrous cap and therefore it allows the guidewire to pass through the CTO lesion more easily (15). Different retrograde techniques, including CART, rendezvous technique, and bidirectional balloon angioplasty, can be used in cases where antegrade crossing has been unsuccessful, but when and how to use these techniques is crucial for operators. Based on our experience, when the guidewire failed to pass through the CTO lesion with the antegrade approach, different retrograde techniques was optimized depended upon the guidewire location. If retrograde intraluminal recanalization fails, we prefer to attempt the CART technique first (16). The principle of CART is to create a subintimal dissection that is limited to the area of the CTO lesion, which facilitated guidewire re-enter the distal true lumen. In the present study, the CART technique was successfully applied in ten CTOs. The common causes for failure of the CART technique are long CTO lesion length or failure to re-enter the true lumen channel.
If the CART technique fails, we usually resort to the rendezvous technique. During rendezvous procedure, retrograde wire from the distal catheter to proximal catheter is performed within the limited subintimal space of CTO lesion. The rendezvous technique was firstly reported by Kim et al. (17) for coronary CTO interventions. Shimada et al. subsequently used the technique for recanalization of a challenging infrapopliteal CTO in a 75-year-old diabetic man with critical limb ischemia (CLI) (18). In the present study, ten CTOs were treated with the rendezvous technique after CART failed. The following tips may improve the success rate of the rendezvous technique: (I) The operative subintimal space should not be dilated, and be limited in the area of the CTO lesion to avoid involvement of normal arteries; and (II) the antegrade catheter should be advanced through the CTO to the distal true lumen step by step while the retrograde sheath was pulled out.
When the antegrade and retrograde subintimal space are separated from each other without any communication, bidirectional balloon dilation angioplasty technique can be performed in an attempt to disrupt arteriosclerotic material or the dissection membrane separating the balloons from each other, which facilitated a subsequent CART or rendezvous technique.
When retrograde recanalization is attempted in combination with antegrade recanalization, a retrograde puncture access must be preserved for any subsequent operation. According to the previous reports, the most common puncture site for retrograde access is the PA; the success rate is 82–100% which, combined with stents placement, can provide a good long-term effect. Other vascular puncture points for retrograde recanalization include the distal SFA and the anterior tibial artery (5,19). Choice of the puncture point depends on the state of the outflow. Based on our experience, infrapopliteal arteries are prior to popliteal artery because popliteal artery cross behind the knee joint, and puncture or sheath placement is inconvenient at this level. If two or more infrapopliteal arteries are patent, anyone can be punctured; but if only one artery is patent, it is better to perform distal SFA or PA puncture and avoid the risk of damage to the only infrapopliteal outflow vessel.
Conclusions
Integrated application of antegrade and retrograde recanalization for the treatment of femoral-popliteal chronic total occlusion is effective and safe. When antegrade angioplasty fails, appropriate use of retrograde angioplasty can increase success rates of CTO recanalization.
Acknowledgements
Funding: This study was funded by the National Natural Science Foundation of China (Nos. 81000652; 81370041, 81271683), Science Foundation of Shanghai Jiaotong University Affiliated Sixth People’s Hospital (No. ynlc201611), and Shanghai key discipline of medical imaging (No. 2017ZZ02005).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of our hospital. All patients provided written informed consent for the endovascular procedure.
References
- Lenti M, Cieri E, De Rango P, Pozzilli P, Coscarella C, Bertoglio C, Troiani R, Cao P. Endovascular treatment of long lesions of the superficial femoral artery: results from a multicenter registry of a spiral, covered polytetrafluoroethylene stent. J Vasc Surg 2007;45:32-9. [Crossref] [PubMed]
- Jacobs DL, Motaganahalli RL, Cox DE, Wittgen CM, Peterson GJ. True lumen re-entry devices facilitate subintimal angioplasty and stenting of total chronic occlusions: Initial report. J Vasc Surg 2006;43:1291-6. [Crossref] [PubMed]
- Ueshima D, Ashikaga T, Shimura T, Hatano Y, Sasaoka T, Kurihara K, Yoshikawa S, Maejima Y, Isobe M. Popliteal Retrograde Approach is Effective and Safe for Superficial Femoral Artery Chronic Total Occlusion. Ann Vasc Dis 2015;8:220-6. [Crossref] [PubMed]
- Cao J, Lu HT, Wei LM, Zhao JG, Zhu YQ. Rendezvous technique for recanalization of long-segmental chronic total occlusion above the knee following unsuccessful standard angioplasty. Vascular 2016;24:157-65. [Crossref] [PubMed]
- Shin S, Kim S, Ko YG, Hong MK, Jang Y, Choi D. Retrograde distal superficial femoral artery approach in the supine position for chronic superficial femoral artery occlusion. Korean Circ J 2014;44:184-8. [Crossref] [PubMed]
- Igari K, Kudo T, Toyofuku T, Inoue Y. Controlled antegrade and retrograde subintimal tracking technique for endovascular treatment of the superficial femoral artery with chronic total occlusion. Ann Vasc Surg 2015;29:1320.e7-10. [Crossref] [PubMed]
- Godino C, Sharp AS, Carlino M, Colombo A. Crossing CTOs-the tips, tricks, and specialist kit that can mean the difference between success and failure. Catheter Cardiovasc Interv 2009;74:1019-46. [Crossref] [PubMed]
- Wei LM, Zhu YQ, Zhao JG, Wang J, Lu HT, Zhang PL. Retrograde Transplantar Arch Angioplasty of Below-the-Knee Arterial Occlusions: Outcomes Compared to Antegrade Recanalization. Acad Radiol 2014;21:1475-82. [Crossref] [PubMed]
- Aihara H, Soga Y, Mii S, Okazaki J, Yamaoka T, Kamoi D, Shintani Y, Ishikawa T. RECANALISE Registry Investigators. Comparison of Long-Term Outcome After Endovascular Therapy Versus Bypass Surgery in Claudication Patients With Trans-Atlantic Inter-Society Consensus-II C and D Femoropopliteal Disease. Circ J 2014;78:457-64. [Crossref] [PubMed]
- Kougias P, Chen A, Cagiannos C, Bechara CF, Huynh TT, Lin PH. Subintimal placement of covered stent versus subintimal balloon angioplasty in the treatment of long-segment superficial femoral artery occlusion. Am J Surg 2009;198:645-9. [Crossref] [PubMed]
- Lammer J, Zeller T, Hausegger KA, Schaefer PJ, Gschwendtner M, Mueller-Huelsbeck S, Rand T, Funovics M, Wolf F, Rastan A, Gschwandtner M, Puchner S, Ristl R, Schoder M. Heparin-bonded covered stents versus bare-metal stents for complex femoropopliteal artery lesions: the randomized VIASTAR trial (Viabahn endoprosthesis with PROPATEN bioactive surface [VIA] versus bare nitinol stent in the treatment of long lesions in superficial femoral artery occlusive disease). J Am Coll Cardiol 2013;62:1320-7. [Crossref] [PubMed]
- Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med 2010;362:1090-101. [Crossref] [PubMed]
- Pulli R, Dorigo W, Guidotti A, Fargion A, Alessi Innocenti A, Pratesi C. The role of infrainguinal bypass surgery in the endovascular era. Ann Vasc Dis 2014;7:7-10. [Crossref] [PubMed]
- Met R, Van Lienden KP, Koelemay MJ, Bipat S, Legemate DA, Reekers JA. Subintimal angioplasty for peripheral arterial occlusive disease: a systematic review. Cardiovasc Intervent Radiol 2008;31:687-97. [Crossref] [PubMed]
- Godino C, Carlino M, Al-Lamee R, Colombo A. Coronary chronic total occlusion. Minerva Cardioangiol 2010;58:41-60. [PubMed]
- Surmely JF, Tsuchikane E, Katoh O, Nishida Y, Nakayama M, Nakamura S, Oida A, Hattori E, Suzuki T. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol 2006;18:334-8. [PubMed]
- Kim MH, Yu LH, Mitsudo K. A new retrograde wiring technique for chronic total occlusion. Catheter Cardiovasc Interv 2010;75:117-9. [PubMed]
- Shimada Y, Kino N, Yano K, Tonomura D, Takehara K, Furubayashi K, Kurotobi T, Tsuchida T, Fukumoto H. Transcollateral Retrograde Approach With Rendezvous Technique for Recanalization of Chronically Occluded Tibial Arteries. J Endovasc Ther 2012;19:620-6. [Crossref] [PubMed]
- Affonso BB, Golghetto Domingos FU, da Motta Leal Filho JM, Maciel MJ, Cavalcante RN, Bortolini E, Carnevale FC. Retrograde Proximal Anterior Tibial Artery Access for Treating Femoropopliteal Segment Occlusion: A Novel Approach. Ann Vasc Surg 2016;33:237-44. [Crossref] [PubMed]