Quite a backup: pericardial varices in a patient with hereditary antithrombin deficiency
Introduction
A 39 year-old female with known hypertension, gastro-esophageal reflux disease, and hereditary anti-thrombin deficiency (hATD) on life-long anti-coagulation presented to our emergency room with acute atypical chest and epigastric pain. Her hATD was diagnosed five years prior when repeated deep vein thromboses were discovered. At that time, the patient was started on life-long anticoagulation with warfarin and was able to consistently achieve therapeutic levels.
Case report
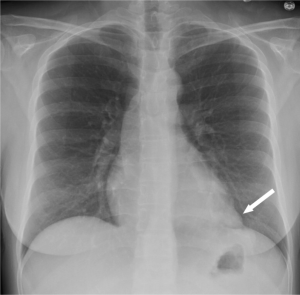
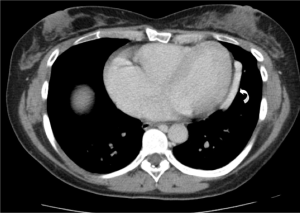
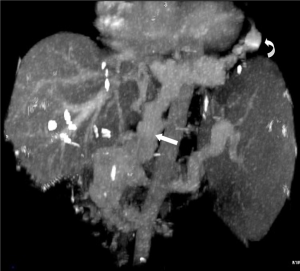
Physical examination of the patient was unremarkable except for mild tenderness to palpation in the epigastric region. Chest radiograph was significant for a circumscribed opacity in the left cardiophrenic angle, isodense to the heart (Figure 1). Contrast-enhanced computed tomography (CT) of her chest, abdomen and pelvis demonstrated evidence of portal thrombosis with cavernous transformation and extensive varices with extension to the left pericardium (Figures 2-4).

Discussion
Anti-thrombin (AT) is a vitamin-K independent glycoprotein that is endogenously produced by the liver and inhibits thrombin, factor Xa, and factor IXa (1).
While rare, hATD, the first identified hereditary thrombophilia, has an autosomal dominant pattern with variable penetrance (2). Individuals with hATD, like other inherited thrombophilias, have a genetic predisposition for forming venous thromboembolisms. The initial thrombotic event in 40% of people with hATD occur spontaneously while the remaining 60% occur in association with other pro-thrombotic risk scenarios such as pregnancy, oral contraceptive use, surgery, and trauma. In a large Spanish study approximately 13% of venous thromboembolisms were caused by inherited thrombophilias (3). The most common anatomical sites include deep veins of the lower extremities and mesenteric veins with up to 60% of patients developing recurrent thrombotic events (4).
While the incidence and prevalence of cardiac varices in patients with inherited thrombophilias remains unknown, 20% of patients with portal hypertension appear to have cardiac varices with most occurring on the right (90%) compared to the left (5).
Currently, patients with hATD and one or more spontaneous thrombosis are recommended to start indefinite anti-coagulation (6). In the setting of acute thrombosis in patients with hATD, heparin should be used with caution as it typically quantitatively lowers AT levels by up to 30% (7). A pooled concentration of AT has been used, and is recommended, for patients with hATD and recurrent or severe thrombosis despite anti-coagulation or with difficulty achieving therapeutic levels of anti-coagulation (8).
Acknowledgements
We would like to thank Jason DiPoce, MD for help with CT image post processing.
Disclosure: The authors declare no conflict of interest.
References
- Khor B, Van Cott EM. Laboratory tests for antithrombin deficiency. Am J Hematol 2010;85:947-50. [PubMed]
- Mackie M, Bennett B, Ogston D, et al. Familial thrombosis: inherited deficiency of antithrombin III. Br Med J 1978;1:136-8. [PubMed]
- Mateo J, Oliver A, Borrell M, et al. Laboratory evaluation and clinical characteristics of 2,132 consecutive unselected patients with venous thromboembolism--results of the Spanish Multicentric Study on Thrombophilia (EMET-Study). Thromb Haemost 1997;77:444-51. [PubMed]
- Thaler E, Lechner K. Antithrombin III deficiency and thromboembolism. In: Prentice CR. ed. Clinics in Haematology, Saunders, London, 1981:369.
- Wachsberg RH, Yaghmai V, Javors BR, et al. Cardiophrenic varices in portal hypertension: evaluation with CT. Radiology 1995;195:553-6. [PubMed]
- Bauer KA. The thrombophilias: well-defined risk factors with uncertain therapeutic implications. Ann Intern Med 2001;135:367-73. [PubMed]
- Hirsh J, Bauer KA, Donati MB, et al. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133:141S-159S.
- Bucur SZ, Levy JH, Despotis GJ, et al. Uses of antithrombin III concentrate in congenital and acquired deficiency states. Transfusion 1998;38:481-98. [PubMed]


