Computed tomography angiography diagnosis of tracheo-innominate fistula: a case report and review of literature
Introduction
A tracheo-innominate fistula (TIF) is a rare complication of tracheostomy placement, developing after less than 1% of surgical tracheostomies. It usually occurs within 3 days to 6 weeks after surgery (1,2). The development of a TIF is devastating and nearly uniformly fatal without treatment (3). Even with treatment, the survival rate is low, as operative mortality is greater than 50%, and fewer than 50% of patients withstanding surgery survive more than 2 months (1,4).
Case report
A 64-year old female nursing home resident presented with uncontrollable bleeding from her tracheostomy. The patient experienced a pontine infarct seven weeks previously, which resulted in severe neurological deficits. The tracheostomy had been inserted at that time.
The tracheostomy cuff was initially inflated, which tamponaded the bleeding, but subsequent deflation of the cuff resulted in a loss of 500 mL of bright red blood. Translaryngeal intubation was performed and a cuffed oro-endotracheal tube was placed distal to the tracheostomy cannula to prevent blood from accumulating in the lungs.
A TIF was suspected and computed tomographic angiography (CTA) of the neck was performed to isolate the source of the hemorrhage. The CTA was performed by using a 16-detector row CT scanner (General Electric LightSpeed 16; General Electric, Fairfield, CT) scanning from the mid brain to the aortic arch. Scan parameters were 120 kV, 350 mA, 0.6 second rotation time, 1.25 mm slice thickness, 1.0 mm reconstruction interval, and pitch of 0.938:1. Intravenous injection of 105 mL of nonionic iodinated contrast media (iohexol, Omnipaque 300, GE Healthcare Inc., Princeton, NJ) was administered with an automatic dual syringe injector at a rate of 4 mL/s, followed by 30 mL of saline solution at a rate of 2.5 mL/s (Stellant D Dual Syringe CT Injection System, Indianola, PA). The injection was timed with a bolus tracking technique.
Initial multiplanar reconstructions (MPRs) and maximum-intensity projections (MIPs) were produced on the CT scanner console. The axial images were transferred to a workstation (Vitrea 4.1; Vital Images, Minnetonka, MN), where additional MPRs, MIPs, and 3-dimensional volume-rendered (3D VR) images were created.
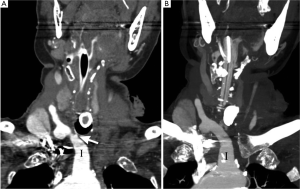
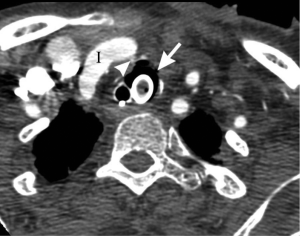
The CTA of the neck revealed extravasation of contrast into the airway and pooling around the tracheostomy cuff, in the hypopharynx and in the oropharynx (Figure 1). The fistulous connection between the proximal innominate artery and the trachea was visualized better on the initial coronal MPRs (Figure 2a), than on the initial coronal MIPs or axial source images (Figures 2b,3). Further MIP and 3D VR image processing and removal of the overlying structures clearly demonstrated the fistulous tract (Figure 4a,b).


An open surgical repair was not feasible due to associated comorbidities. Emergent endovascular treatment was therefore undertaken. Arteriography revealed extravasation at the level of the innominate artery. Using a retrograde right common carotid artery approach, a modified, covered stent was placed into the innominate artery. After ballooning the graft, a completion angiogram revealed no further extravasation from the innominate artery. Excellent flow in the aorta and right common carotid artery were observed.
Discussion
A TIF is an uncommon occurrence encountered following placement of a tracheostomy. A TIF has been described both as early (1) and late term tracheostomy complications (5). Although the exact pathogenesis is not entirely understood, known risk factors include low placement of the stoma, infection and pressure necrosis from high cuff pressure (6). Hamano et al. described 10 patients with TIFs in whom an endotracheal granuloma resulted in inflammation extending to the surrounding tissue (7).
The majority of tracheoarterial fistulas communicate with the innominate artery (1,7). Tracheo-carotid arterial fistulas are less common.
The small size of the fistula presents a major diagnostic challenge (1). While bronchoscopy had been indicated as the diagnostic procedure of choice (1,6,8), CTA can be helpful in surgical planning by identifying the fistula and the responsible vessel. Non-invasive CTA has already been proven to be an accurate modality and is widely used in pre-procedural assessment of aortoesophageal (9), intracranial (10,11), coronary (12,13), peripheral arterial (14,15), aortocaval (16) and iatrogenic (17,18) fistulas.
TIF visualization with catheter angiography is well documented (4,8,19,20). Use of multidetector CT with 3D reconstructions has been described prior to (21) and following (19) the repair of a TIF and for prophylactic innominate artery transsection (22). If an endovascular repair is selected, a CT angiogram demonstrating the location of the pathology allows for precise placement of the stent. Prior imaging can also help direct open surgical repair. CTA has several advantages relative to conventional angiography including a reduction in the radiation dose of at least two to three times (23) and more rapid acquisition times.
Although CT has been reported to identify tracheal compression by an artery (22), intimate contact of an artery with the trachea (8), arterial erosion (21) and mediastinal infiltration (8), actual visualization of a fistula with CTA has not yet been reported. To our knowledge, this is the first reported case clearly illustrating the TIF course with CTA and demonstrating its impact on subsequent management.
Preoperative diagnosis of a TIF allows for operative management using either an endovascular or open surgical approach. Since publication of the first endovascular repair with stent grafting 10 years ago (24), this therapeutic option has become widely accepted (2,25,26). It has been found useful particularly in patients with multiple comorbidities as either a temporizing (8,19) or a definitive measure (24). Review of five TIF cases with 14 to 24 month follow up treated with endografts by Sorial et al. (27) demonstrated that three patients survived. The option of endovascular embolization of the innominate artery has also been discussed in the literature (26).
The traditional open approach with ligation of the innominate artery (6) and debridement of the affected trachea (1,28) is the mainstay of surgical treatment with survival ranging from 25% (29,30) to less than 50% (4).
We compared the quality of TIF visualization on axial images vs. various post-processing techniques including MPRs, MIPs and 3D VR. We found better visualization of the fistula on the sagittal and coronal MPRs.
Part of the benefit of MPRs can be explained by the predominant craniocaudal orientation of the fistulous tract, which is in the plane of these reformations. The narrow shape of a TIF (1) and its short dimension in the anterior-posterior plane render visualization on axial images rather challenging. The ability to visualize a narrow contrast column with MPRs has been illustrated during analysis of a thin stenotic lumen in carotid arteries (31).
On the initial MIPs performed with the entire data set, the faint TIF was obscured because it was less dense than the overlapping high attenuation pool of extravasated contrast material and the prominent eroded vessel. This limitation is inherent in MIPs’ display of only the highest attenuation values, with loss of depth perception within the displayed plane (32-35). The resulting superimposition artificially alters and hides small structures.
Unlike MIPs, MPRs use all attenuation values in the data set (32). This improves visualization of a thin contrast filled fistulous tract surrounded by adjacent high density vessels, pooling endotracheal contrast, and the tracheostomy cannula.
Three dimensional imaging, and especially volume rendering, has been shown to be valuable for accurately depicting small vascular structures (36) and narrow contract columns (37). After prior localization with MPRs and removal of overlying structures, the 3D images and matching MIPs provided clear delineation of the spatial relationship of the slender fistulous tract to the anatomic structures of interest. This information has been shown to be of value specifically in innominate artery surgical planning (22).
On 3D imaging, it is helpful to decrease the artifact from the dense tracheostomy cannula with a bone subtraction algorithm (38).
In conclusion, this is the first report of a clearly visualized TIF with CTA together with a review and analysis of the relative utility of various image post-processing techniques. We believe that CT angiography has an important role in management of this devastating condition, as it enables expedited diagnosis in a critical setting requiring emergent intervention.
Acknowledgements
We thank Noah Weg, MD and Daniel Alterman, MD for manuscript critique, Criticus P. Marak, MD for critical care insights.
Disclosure: The authors declare no conflict of interest.
References
- Allan JS, Wright CD. Tracheoinnominate fistula: diagnosis and management. Chest Surg Clin N Am 2003;13:331-41.
- Cohen JE, Klimov A, Rajz G, et al. Exsanguinating tracheoinnominate artery fistula repaired with endovascular stent-graft. Surg Neurol 2008;69:306-9.
- Kapural L, Sprung J, Gluncic I, et al. Tracheo-innominate artery fistula after tracheostomy. Anesth Analg 1999;88:777-80.
- Gelman JJ, Aro M, Weiss SM. Tracheo-innominate artery fistula. J Am Coll Surg 1994;179:626-34.
- Epstein SK. Late complications of tracheostomy. Respir Care 2005;50:542-9.
- Grant CA, Dempsey G, Harrison J, et al. Tracheo-innominate artery fistula after percutaneous tracheostomy: three case reports and a clinical review. Br J Anaesth 2006;96:127-31.
- Hamano K, Kumada S, Hayashi M, et al. Hemorrhage due to tracheoarterial fistula with severe motor and intellectual disability. Pediatr Int 2008;50:337-40.
- Sessa C, Costache V, Porcu P, et al. Tracheoinnominate artery fistula: combined endovascular and surgical management by emergency stent-graft placement followed by cryopreserved arterial allograft repair. Ann Vasc Surg 2006;20:731-5.
- Geisbüsch P, Kotelis D, Weber TF, et al. Endovascular repair of ruptured thoracic aortic aneurysms is associated with high perioperative mortality and morbidity. J Vasc Surg 2010;51:299-304.
- Nakagawa M, Sugiu K, Tokunaga K, et al. Usefulness of 3-dimensional CT angiograms obtained by 64-section multidetector row CT scanner for dural arteriovenous fistula. J Neuroimaging 2009;19:179-82.
- Wu HC, Ro LS, Chen CJ, et al. Isolated ocular motor nerve palsy in dural carotid-cavernous sinus fistula. Eur J Neurol 2006;13:1221-5.
- Early SA, Meany TB, Fenlon HM, et al. Coronary artery fistula; coronary computed topography--the diagnostic modality of choice. J Cardiothorac Surg 2008;3:41.
- Yang S, Zeng MS, Zhang ZY, et al. Sixty-four-multi-detector computed tomography diagnosis of coronary artery anomalies in 66 patients. Chin Med J (Engl) 2010;123:838-42.
- Peynircioğlu B, Ergun O, Hazirolan T, et al. Stent-graft applications in peripheral non-atherosclerotic arterial lesions. Diagn Interv Radiol 2008;14:40-50.
- Chen JK, Johnson PT, Fishman EK. Diagnosis of clinically unsuspected posttraumatic arteriovenous fistulas of the pelvis using CT angiography. AJR Am J Roentgenol 2007;188:W269-73.
- von Heesen M, Sperling J, Plusczyk T, et al. Multimodal approach in coincidence of covered ruptured abdominal aortic aneurysm and aortocaval fistula. Dtsch Med Wochenschr 2010;135:2296-9.
- Rooijens PP, Serafino GP, Vroegindeweij D, et al. Multi-slice computed tomographic angiography for stenosis detection in forearm hemodialysis arteriovenous fistulas. J Vasc Access 2008;9:278-84.
- Cavagna E, D’Andrea P, Schiavon F, et al. Failing hemodialysis arteriovenous fistula and percutaneous treatment: imaging with CT, MRI and digital subtraction angiography. Cardiovasc Intervent Radiol 2000;23:262-5.
- Wall LP, Gasparis A, Criado E. Endovascular therapy for tracheoinnominate artery fistula: a temporizing measure. Ann Vasc Surg 2005;19:99-102.
- Yang FY, Criado E, Schwartz JA, et al. Trachea-innominate artery fistula: retrospective comparison of treatment methods. South Med J 1988;81:701-6.
- Ghai B, Makkar JK, Bakshi J, et al. Survival of a child without sequelae after tracheoarterial fistula. Paediatr Anaesth 2007;17:588-91.
- Hasegawa T, Zaima A, Hisamatsu C, et al. Minimally invasive innominate artery transection for tracheomalacia using 3-dimensional multidetector-row computed tomographic angiography: report of a case. J Pediatr Surg 2010;45:E1-4.
- Siegel MJ. Multiplanar and three-dimensional multi-detector row CT of thoracic vessels and airways in the pediatric population. Radiology 2003;229:641-50.
- Deguchi J, Furuya T, Tanaka N, et al. Successful management of tracheo-innominate artery fistula with endovascular stent graft repair. J Vasc Surg 2001;33:1280-2.
- Vianello A, Ragazzi R, Mirri L, et al. Tracheoinnominate fistula in a Duchenne muscular dystrophy patient: successful management with an endovascular stent. Neuromuscul Disord 2005;15:569-71.
- Takasaki K, Enatsu K, Nakayama M, et al. A case with tracheo-innominate artery fistula. Successful management of endovascular embolization of innominate artery. Auris Nasus Larynx 2005;32:195-8.
- Sorial E, Valentino J, Given CA, et al. The emergency use of endografts in the carotid circulation to control hemorrhage in potentially contaminated fields. J Vasc Surg 2007;46:792-8.
- Ailawadi G. Technique for managing tracheo-innominate artery fistula. Op Tech Thorac Cardiovasc Surg 2009;14:66-72.
- Yoshida K, Ohshima H, Iwata K, et al. Rupture of the innominate artery following tracheostomy: report of a case. Surg Today 1998;28:433-4.
- Grillo HC, Mathisen DJ. Cervical exenteration. Ann Thorac Surg 1990;49:401-8; discussion 408-9.
- Hirai T, Korogi Y, Ono K, et al. Maximum stenosis of extracranial internal carotid artery: effect of luminal morphology on stenosis measurement by using CT angiography and conventional DSA. Radiology 2001;221:802-9.
- Lell MM, Anders K, Uder M, et al. New techniques in CT angiography. Radiographics 2006;26:S45-62.
- Napel S, Marks MP, Rubin GD, et al. CT angiography with spiral CT and maximum intensity projection. Radiology 1992;185:607-10.
- Calhoun PS, Kuszyk BS, Heath DG, et al. Three-dimensional volume rendering of spiral CT data: theory and method. Radiographics 1999;19:745-64.
- Saba L, Mallarini G. Differences between MIP and MPR techniques in the carotid artery stenosis degree measurement. Evaluation using multi-detector-row CT angiograph. Minerva Cardioangiol 2008;56:21-7.
- Remy J, Remy-Jardin M, Giraud F, et al. Angioarchitecture of pulmonary arteriovenous malformations: clinical utility of three-dimensional helical CT. Radiology 1994;191:657-64.
- Saba L, Sanfilippo R, Montisci R, et al. Assessment of intracranial arterial stenosis with multidetector row CT angiography: a postprocessing techniques comparison. AJNR Am J Neuroradiol 2010;31:874-9.
- Lell M, Anders K, Klotz E, et al. Clinical evaluation of bone-subtraction CT angiography (BSCTA) in head and neck imaging. Eur Radiol 2006;16:889-97.


