Thoracic wall trauma—misdiagnosed lesions on radiographs and usefulness of ultrasound, multidetector computed tomography and magnetic resonance imaging
Introduction
Blunt injuries to the chest wall are the third most common injuries in trauma patients, next to injuries to the head and extremities, resulting from motor vehicle collisions, falls, and blows from blunt objects. The spectrum of injuries includes chest wall contusion, haematoma in the chest wall or extrapleural space, and fractures. These injuries account for approximately 25% of trauma-related deaths in the United States (1). Thoracic trauma has an overall fatality rate of 10.1%, which is higher in patients with cardiac or tracheobronchial-oesophageal injuries (2). Most thoracic trauma is primarily evaluated at the emergency room (ER) using simple chest X-ray. Because of its low sensibility, some chest wall lesions such as rib and costal cartilage fractures, sternoclavicular dislocation and soft tissue lesions may be missed.
Computed tomography (CT) is the main imaging modality used to evaluate thoracic trauma, including rib fractures and associated complications. Studies have shown that CT may demonstrate significant diseases (e.g., thoracic aortic injury) in patients with normal initial radiographs (3). Furthermore, CT has been credited with changing management in up to 20% of chest trauma patients with abnormal initial radiographs (4). Use of multidetector CT (MDCT) helps in reconstructing multiplanar volume-rendered images, while CT angiography can be used to identify vascular injury.
By contrast, other authors have emphasized that unnecessarily MDCT scans expose patients to potentially harmful ionizing radiation. For instance, when performing after a normal chest radiograph, CT diagnoses only one major injury for every 67 studies (5). Rodriguez et al. have designed a cohesive summary algorithm so-named NEXUS Chest X-ray, which consists of seven criteria (age >60 years; rapid deceleration mechanism; chest pain; intoxication; altered mental status; distracting painful injury; and chest wall tenderness) and exhibits a sensitivity of 99.0% [95% confidence interval (CI), 98.2–99.4%) and a specificity of 13.3% (95% CI, 12.6–14.0%) for detecting clinically significant injuries, reinforcing the efficacy of X-ray chest imaging in the evaluation of all blunt trauma patients (6). Ultrasonography (US) is increasingly being used for trauma patients to help identify fractures, haemothorax, pneumothorax and to evaluate cardiac function. Magnetic resonance imaging (MRI) is not routinely used to identify acute traumatic thorax injury; however, it can be used to help identify stress fractures, rib fractures, adjacent soft-tissue injury, and intercostal muscle strains (7). This article aimed to review the role of different imaging methods in evaluating thoracic wall trauma.
Rib fractures
Rib fractures represent an important indicator of trauma severity; of note, morbidity and mortality increase as the number of fractured ribs increases. In one manuscript previously reported, 81% of patients with two or more rib fractures had either haemothorax or pneumothorax (8). The supine frontal radiograph is usually the initial imaging study obtained in a trauma patient, despite some authors have reported the modest sensitivity of anteroposterior (AP) chest radiograph for thoracic injuries. As a matter of fact, in this study of 374 patients with blunt trauma, approximately half of all pneumothorax, rib fractures, and pulmonary contusions were not apparent on AP chest radiograph (9). Nevertheless, some studies have shown that posteroanterior (PA) radiograph has a good specificity but not sensitivity for rib fracture, although its sensitivity is higher than those of AP radiograph (10). In fact, up to 50% of rib fractures are missed at radiography, even when images with dedicated oblique rib views are obtained. Dedicated rib views rarely provide any additional information that would change management and should be avoided (7). The American College of Radiology (ACR) has established an algorithm for the imaging evaluation of rib fractures (11). The first decision involves evaluation of the mechanism of injury. For blunt trauma with a high-energy mechanism, CT angiography or contrast-enhanced chest CT should be performed. In these situations, the examination is tailored to investigate soft-tissue, vascular, and internal organ injuries. Chest radiography is a complementary examination; injuries are underestimated on AP radiograph when compared with CT images (12). Other authors have reported the role of US in the detection of rib fractures. US is more sensitive in the detection of rib fractures including chondral rib fractures, as compared with conventional radiography (78% and 12%, respectively). Trans-thoracic US of the chest is useful in the evaluation of a wide range of peripheral, parenchymal, pleural, and chest wall diseases and missed rib fractures (13).
Types of rib injuries
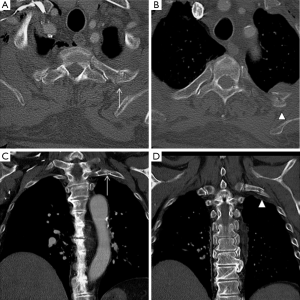
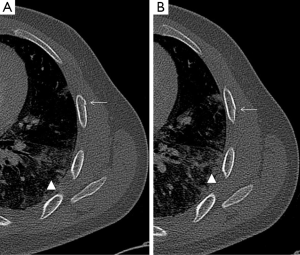
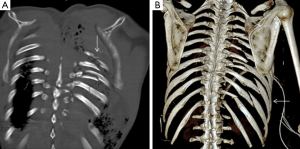
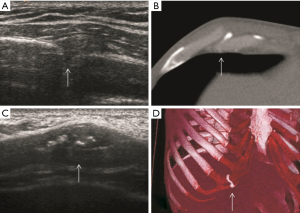
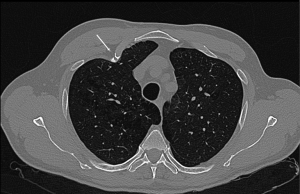
A nondisplaced rib fracture is defined as a rib fracture with complete cortical disruption but with maintained alignment, usually involving the medullar bone and both the inner and outer cortices (Figure 1); it is seen such a lucent line on radiographs or CT images (14). Stress rib fractures are overuse injuries that occur when there is an abnormal force on normal underlying bone. These begin with a small stress on the bone, which with repeat injury results in a microtrabecular fracture that may progress to rib fracture. These injuries are rare, although possibly underdiagnosed, and most often seen in workers who perform repetitive motions and athletes. Detection of non-displaced and stress rib fractures on radiographs is difficult, and these injuries may be seen radiographically only at follow-up imaging, after signs of healing have manifested (7). On the contrary, MRI can show immediately an area of oedema (high T2 signal) after a traumatic event. When cortical disruption and a substantial abnormality in alignment are evident, a rib fracture is classified as displaced. Displacement may be minimal or obvious. Displaced fractures may be identified on radiographs or CT images (Figure 1). Injury to the surrounding tissues and structures can occur, and several lethal complications such an aortic injury have been documented in the literature (15). A buckle fracture of the rib occurs when there is disruption of either the inner or outer cortex (Figure 2) with no observable fracture of the other cortex (16). Some researchers have reported that the term buckle is derived from engineering terminology that describes disruption of the inner or tensile side of a structure that is placed under force (7,17). Flail chest (“volet”) is a traumatic condition in which there are three or more contiguous ribs with fractures in two or more places (Figure 3). Fractures usually occur in the anterior and anterolateral portions of the middle to lower ribs (1). These fractures create a flail segment that can move paradoxically relative to the remainder of the chest during respiration in a spontaneously ventilating patient. Although imaging can show fractures, it is the clinical examination that will demonstrate paradoxical motion. Flail chest serves as a marker for significant intrathoracic injury, since more than one-half of the affected patients may have associated injuries that require surgical treatment (18).
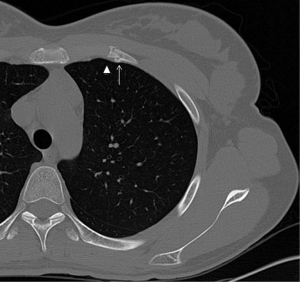
Injuries of the costal cartilage
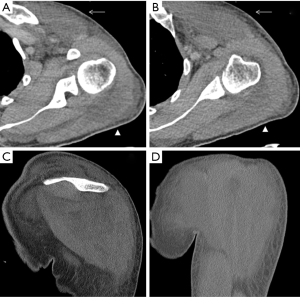
Injury to the rib-cartilage complex can occur at multiple sites along the anatomic arc from spine to sternum. Injuries to the chondrocostal junction (Figure 4) are termed rib separations, while nearby disruptions of the chondrosternal junction are called rib disruptions. The cartilage may itself be fractured (19). Radiographs, although useful for detecting osseous abnormalities, are insensitive to detect cartilage and soft-tissue abnormalities. Because costal cartilage injuries are often located in the junctional regions; chondrosternal and chondrocostal, the overlapping osseous structures in these areas limit the usefulness of radiographs. A Canadian study from Subhas et al. showed that cross-sectional techniques such as CT, US and MRI are more sensitive to detect these injuries (Figure 5) (20). On CT, cartilage density is relatively uniform (70–120 HU), in which this value is higher than fat and muscle but lower than calcium (Figure 6). Costal cartilage fractures are visualized as a low-density area through the costal cartilage, with surrounding calcifications near old fractures and gas density within the cleft in some cases. Swelling of surrounding soft tissue could also be seen. Other imaging techniques such as MDCT, US and MRI have been evaluated. In the largest published series, Malghem et al. described a series of eight patients with 15 costal cartilage injuries diagnosed on CT in all patients and on US in three of them. Their patient population was young (mean age, 27.5 years), and all of them had a prior traumatic injury, related to contact sports in three patients (19). Costal cartilage injuries are readily visible on MRI because of the high signal from the surrounding oedema; they are often more conspicuous than those of CT images. Even in cases of remote injury, high T2 signal was visualized at the site of fracture that was presumably due to non-union given the persistent clinical symptoms. In fact, the characteristically imaging appearance of MRI for cartilage injuries, as in ribs fractures, is an increase oedema-like signal on T2 at the site of injury. Also, oedema-like signal T2 could be seen in the surrounding soft tissue in recent or subacute injuries (<3 months). A fracture line, which is not always present, appears as a localized linear oedema-like decreased T1 and increased T2 signal, and it is best to be visualized on the fluid-sensitive sequences (fat-saturated fast spin-echo T2-weighted or STIR-weighted sequences) and in the coronal plane (20).
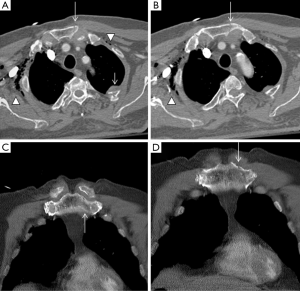
Sternal or clavicular fractures
Sternal fractures may result from deceleration injuries or direct blows to the anterior chest wall. Fractures commonly involve the sternal body and the manubrium. Although sternal fractures have been viewed as a marker for high-energy trauma (21), a simple sternal fracture may also occur as an isolated injury (22). However, displaced sternal fractures and those with associated manubrial-sternal joint disruption frequently occur with an association to thoracic, cardiac, and spinal injuries. Sternal fractures are best demonstrated on multiplanar reformatted CT images (Figures 7,8). Occasionally, a fracture line may be difficult to detect on axial CT, and the presence of anterior mediastinal haemorrhage could be the clue for diagnosis (1). Some anatomical variants can be expected (Figure 9); for instance, the xiphoid process has several morphologic variants (pointed, oval, and forked shapes; one, two or more xiphoid foramina) that are well evaluated by MDCT (23,24). These findings should be kept in mind for avoiding diagnostic imaging mistakes.

Clavicle fractures mostly occur in young adults as the result of a sports injury or direct trauma (Figure 10). Clavicle fractures secondary to minor trauma have been rarely reported associated to a tumour, such as multiple myeloma (25). In cases of fractures secondary to minor trauma, a pathological aetiology should always be excluded. Most nondisplaced or minimally displaced injuries can be treated conservatively (26).
Sternoclavicular dislocation
Sternoclavicular dislocations account for fewer than 5% of all dislocations of the scapular belt. Most cases of anterior dislocation of the sternoclavicular joint do not present with any clinical symptoms. However, some patients may develop chronic anterior instability and may continue to present symptoms. In these cases, surgical treatment is indicated (27). Sternoclavicular dislocations usually occur following traumatic events. Anterior dislocation often follows motor vehicle accidents, or occurs during sporting activities. Posterior dislocation is considered less common and it is classically secondary to indirect trauma. When a force is applied to the posterolateral shoulder, the lateral portion of the clavicle is displaced anteriorly. With a taut costoclavicular ligament acting as a fulcrum, the medial clavicle is then levered behind the sternum. Direct trauma to the anteromedial portion of the clavicle is a considerably less frequent condition (28).
Nevertheless, other authors contradict previously reported results; in a study of 41 patients with sternoclavicular joint pain related to trauma, MRI found 24 subluxations (59%), which antero-posterior axis was displaced anterior in three patients (7%) and posterior in 11 patients (27%), whereas supero-inferior axis was superior in 17 patients (41%) and inferior in two (5%). The authors explained this discrepancy based on their patient population, consisted of patients with more delayed and chronic symptoms (29). Dislocation of the sternoclavicular joint should always be considered in a trauma patient with pain, swelling, or deformity over the medial clavicle. Because of the potential for serious complications with a posterior dislocation, rapid diagnosis is essential. In practice, this will usually involve a chest radiograph, one of the specialized sternoclavicular views, followed by an immediate CT examination if possible (27). In fact, posterior sternoclavicular dislocations may be subtle or not visualized on conventional radiography. Therefore, when there is a clinical suspicion for this entity, CT with intravenous contrast material administration can be used to confirm the diagnosis and evaluate for possible associated vascular injury (1).
Thoracic wall muscle injuries
Thoracic wall muscle injuries in a traumatic context may be easily missed, since plain radiographs don’t usually reveal fractures or other bony abnormalities, and even more advanced imaging modalities such as CT may be insensitive to these lesions. Symptoms are generally non-specific and include acute pain, stiffness and swelling. A sensation of a muscle “pop” or “crunch” may raise suspicion of an underlying muscle injury. Physical examination can elicit limited range of motion, ecchymosis, asymmetric abnormal contour and a palpable mass.
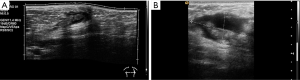
US findings of tendinous and muscular lesions injuries include disruption, absence and retraction of the tendon and muscle fibres, as well as haematoma. Immediately after injury, a haemorrhage is hypoechoic; however, it will become heterogeneously echogenic with clot formation and organization into a haematoma.
In comparison to US, MR imaging is less operator dependent, facilitates a more global assessment of the entire chest, and enables better differentiation of tendon tissue from tissues affected by trauma. It is the imaging method of choice when the diagnosis is not clear, and may avoid surgical delays particularly when surgery is indicated. Different MR imaging protocols may be suitable for imaging of thoracic wall muscles. T1-weighted sequences are good for evaluating the anatomy but lack sensitivity in the detection of fluid, with exception of some chronic hematomas due to very short T1 values (and corresponding brightness on T1-weighted images). Fluid-sensitive MR imaging sequences such as STIR, T2-weighted imaging with fat saturation, and proton-density—weighted imaging with fat saturation are essential for detecting increased fluid signal intensity induced by a traumatic process.
The pectoralis major is the most superficial of the anterior scapular muscles. It originates on the clavicle, sternum, rectus sheath, and on the costal cartilages of the first six ribs, inserting on the lateral lip on the bicipital groove. The frequency of injuries of the pectoralis major muscle has been increasing during the past two decades (30). This trend can be attributed in part to increasing cases of sports-related trauma and the growing popularity of weight-training regimens such as bench press weight-lifting exercises. Patients are generally young and active. The most common mechanism of injury is excessive tension on a maximally contracted muscle (31). Injuries of the pectoralis major can be categorized according to their location: muscle origin or belly, musculotendinous junction, intratendinous region, humeral insertion, or area of bone avulsion at the humeral attachment. Most of pectoralis major injuries occur at the humeral insertion (59%) and musculotendinous junction (24%) (32). Patients with injuries at the muscle origin or belly, including contusions and strains, usually are treated conservatively. Injuries involving bone avulsion at the humeral attachment may benefit from a primary fracture fixation (33).
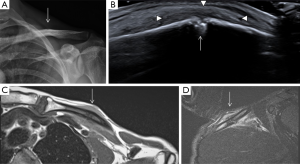
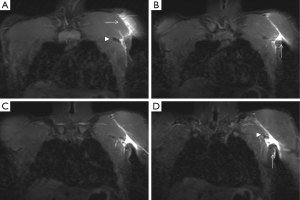
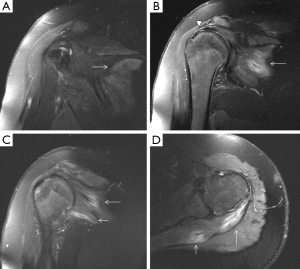
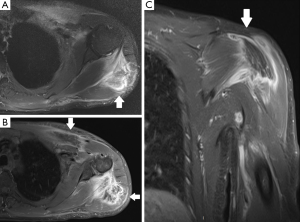
A normal pectoralis major tendon should have uniform low signal intensity on MR imaging. Like US (34), tears of the pectoralis major tendon seen on MR imaging exhibit different degrees of tendon abnormality, depending on the degree of injury. A grade I strain of the muscle belly will have feathery intramuscular fluid-sensitive signal intensity, which represents oedema and/or haemorrhage. Grade II injury will appear as a partial tear with an intramuscular hematoma, while grade III injury has a complete tear with possible retraction (Figures 11-13). As a matter of fact, a partial tear involving only the posterior sternal segments, the anterior clavicular head and tendon will be intact, with the long head of the biceps tendon in place. With complete tears involving both the sternal head and the clavicular head, however, there will be disruption of the entire tendon, with anterior displacement of the long head of the biceps tendon (35).
The serratus anterior originates in the lateral surfaces of the 1st to 9th ribs and inserts on the medial border of the scapula. This muscle is thought to be implicated in stress fractures in middle and lower ribs, but can also be injured itself due to acute trauma, with cases described in association with sport activities, such as rowing and baseball (36).
The latissimus dorsi is a large posterior and inferior thoracic muscle, extending from the spine to the axillary region. It inserts on the spinous processes of the last seven dorsal vertebrae, as well as on the spinous processes of lumbar and sacral vertebrae, and on the 10th to 12th ribs, ending as a flattened tendon in the bicipital groove of the humerus. Injury of the latissimus dorsi typically occurs in the setting of an acute traumatic event and most commonly involves an avulsion injury of the tendon. The mechanism involved is usually a forceful abduction and external rotation during resisted contraction (37).
The rotator cuff stabilizes the humeral head in the glenoid cavity and comprises the supraspinatus, infraspinatus, teres minor and the subscapularis muscles and tendons. They all originate in the scapula (the supraspinatus on the supraspinous fossa, the infraspinatus on the infraspinous process, the teres minor on the posterior surface of the scapula and the subscapularis on the subscapular fossa), and their tendons insert on the humerus (the first three on the greater tubercle of the humerus, and the subscapularis on the lesser tubercle). Tears of the rotator cuff are more common in older patients, generally associated with degenerative changes (the supraspinatus being the most commonly involved). However, acute traumatic tears can also occur in young and athletic individuals. Lesions usually affect the humeral insertion of the rotator cuff tendons, but can also more rarely affect their muscular origins in the scapula. Clinical examination and plain radiographs are almost never helpful in predicting rotator cuff muscle tears immediately after trauma, whereas MRI has proven its usefulness in the assessment of these lesions (Figure 14). Patients with injuries at the muscle origin or belly are treated conservatively (38).
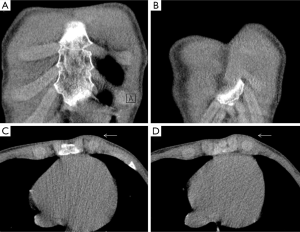
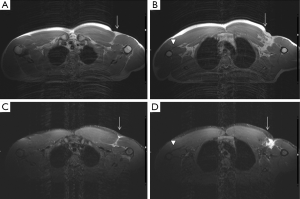
A rare clinical emergency so-called “deep tissue injury syndrome (DTI)” has been previously reported, characterized by a severe pressure ulcer necrotic tissue mass under intact skin (39). This unusual entity affects unconscious patients lying down in the same position after a long period of time, where thoracic wall muscles could be damaged. DTI can be identified using US (40), CT (41) and MRI (42). Soft-tissue swelling with myonecrosis is the hallmark of this pathology (Figures 15,16). It often requires surgical interventions and endangers the life of patients with motosensory impairments (43). Therefore, a delayed diagnosis must be avoided.
In conclusion, different types of traumatic events affecting the chest wall, such as rib and costal cartilage fractures, sternoclavicular dislocation and soft tissue lesions may be misdiagnosed with conventional X-ray. MDCT is considered the “gold-standard” for traumatic patients (especially polytraumatized patients), due to its fast acquisition covering the whole area of interest in axial plane (including other anatomic areas at the same time), reconstructing multiplanar (2D, 3D) volume-rendered images with a superb quality and angiographic CT capabilities for evaluating vascular injury (1,3) with changing management in up to 20% of chest trauma patients (4). However, radiologists must be aware of unnecessarily MDCT scans expose patients to potentially harmful ionizing radiation (5,6). In front of subtle rib fractures and muscle-tendinous tears, complementary techniques such as US and MRI may improve the diagnostic accuracy (19,20,32,35,38,42). All these imaging methods have an important role in quantifying the severity of chest wall trauma.
Acknowledgements
To our MDCT, US and MRI technicians Enrique Jorcano, David Flores, Carlos Reguera, Isaac Pomes, Jose Bonilla, Maria Ariño, Santiago Sotes, Marta Soto and Joan Ramon Sabate for their daily job and interest.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kaewlai R, Avery LL, Asrani AV, Novelline RA. Multidetector CT of blunt thoracic trauma. Radiographics 2008;28:1555-70. [Crossref] [PubMed]
- The American College of Surgeons Committee on Trauma Leadership. In: Clark DE, Fantus RJ, eds. National Trauma Data Bank (NTDB) Annual Report 2007. Chicago: American College of Surgeons, 2007:1-64.
- Exadaktylos AK, Sclabas G, Schmid SW, Schaller B, Zimmermann H. Do we really need routine computed tomographic scanning in the primary evaluation of blunt chest trauma in patients with "normal" chest radiograph? J Trauma 2001;51:1173-6. [Crossref] [PubMed]
- Omert L, Yeaney WW, Protetch J. Efficacy of thoracic computerized tomography in blunt chest trauma. Am Surg 2001;67:660-4. [PubMed]
- Rodriguez RM, Baumann BM, Raja AS, Langdorf MI, Anglin D, Bradley RN, Medak AJ, Mower WR, Hendey GW. Diagnostic yields, charges, and radiation dose of chest imaging in blunt trauma evaluations. Acad Emerg Med 2014;21:644-50. [Crossref] [PubMed]
- Rodriguez RM, Hendey GW, Mower WR. Selective chest imaging for blunt trauma patients: The national emergency X-ray utilization studies (NEXUS-chest algorithm). Am J Emerg Med 2017;35:164-170. [Crossref] [PubMed]
- Talbot BS, Gange CP Jr, Chaturvedi A, Klionsky N, Hobbs SK, Chaturvedi A. Traumatic Rib Injury: Patterns, Imaging Pitfalls, Complications, and Treatment. Radiographics 2017;37:628-651. [Crossref] [PubMed]
- Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardiothorac Surg 2003;23:374-8. [Crossref] [PubMed]
- Barrios C. Jr1, Pham J, Malinoski D, Dolich M, Lekawa M, Cinat M. Ability of a chest X-ray and an abdominal computed tomography scan to identify traumatic thoracic injury. Am J Surg 2010;200:741-4. [Crossref] [PubMed]
- Chung JH, Cox CW, Mohammed TL, Kirsch J, Brown K, Dyer DS, Ginsburg ME, Heitkamp DE, Kanne JP, Kazerooni EA, Ketai LH, Ravenel JG, Saleh AG, Shah RD, Steiner RM, Suh RD. ACR appropriateness criteria blunt chest trauma. J Am Coll Radiol 2014;11:345-51. [Crossref] [PubMed]
- Expert Panel on Thoracic Imaging. Henry TS, Kirsch J, Kanne JP, Chung JH, Donnelly EF, Ginsburg ME, Heitkamp DE, Kazerooni EA, Ketai LH, McComb BL, Parker JA, Ravenel JG, Restrepo CS, Saleh AG, Shah RD, Steiner RM, Suh RD, Mohammed TL; American College of Radiology. ACR Appropriateness Criteria® rib fractures. J Thorac Imaging 2014;29:364-6. [PubMed]
- Traub M, Stevenson M, McEvoy S, Briggs G, Lo SK, Leibman S, Joseph T. The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury 2007;38:43-7. [Crossref] [PubMed]
- Turk F, Kurt AB, Saglam S. Evaluation by ultrasound of traumatic rib fractures missed by radiography. Emerg Radiol 2010;17:473-7. [Crossref] [PubMed]
- Cho SH, Sung YM, Kim MS. Missed rib fractures on evaluation of initial chest CT for trauma patients: pattern analysis and diagnostic value of coronal multiplanar reconstruction images with multidetector row CT. Br J Radiol 2012;85:e845-50. [Crossref] [PubMed]
- Bruno VD, Batchelor TJ. Late aortic injury: a rare complication of a posterior rib fracture. Ann Thorac Surg 2009;87:301-3. [Crossref] [PubMed]
- De Maeseneer M, De Mey J, Lenchik L, Everaert H, Osteaux M.. Helical CT of Rib Lesions: A Pattern-Based Approach. AJR Am J Roentgenol 2004;182:173-9. [Crossref] [PubMed]
- Yang KM, Lynch M, O'Donnell C. "Buckle" rib fracture: an artifact following cardio-pulmonary resuscitation detected on postmortem CT. Leg Med (Tokyo) 2011;13:233-9. [Crossref] [PubMed]
- Athanassiadi K, Gerazounis M, Theakos N.. Management of 150 flail chest injuries: analysis of risk factors affecting outcome. Eur J Cardiothorac Surg 2004;26:373-6. [Crossref] [PubMed]
- Malghem J, Vande Berg B, Lecouvet F, Maldague B. Costal cartilage fractures as revealed on CT and sonography. AJR Am J Roentgenol 2001;176:429-32. [Crossref] [PubMed]
- Subhas N, Kline MJ, Moskal MJ, White LM, Recht MP. MRI evaluation of costal cartilage injuries. AJR Am J Roentgenol 2008;191:129-32. [Crossref] [PubMed]
- Livingston DH, Haurer CJ. Trauma to the chest wall and lung. In: Moore EE, Feliciano DV, Mattox KL. editors. Trauma. 5th ed. Philadelphia, PA: McGraw-Hill, 2004:507-37.
- Knobloch K, Wagner S, Haasper C, Probst C, Krettek C, Vogt PM, Otte D, Richter M. Sternal fractures are frequent among polytraumatised patients following high deceleration velocities in a severe vehicle crash. Injury 2008;39:36-43. [Crossref] [PubMed]
- Akin K, Kosehan D, Topcu A, Koktener A. Anatomic evaluation of the xiphoid process with 64-row multidetector computed tomography. Skeletal Radiol 2011;40:447-52. [Crossref] [PubMed]
- Xie YZ, Wang BJ, Yun JS, Chung GH, Ma ZB, Li XJ, Kim IS, Chai OH, Han EH, Kim HT, Song CH. Morphology of the human xiphoid process: dissection and radiography of cadavers and MDCT of patients. Surg Radiol Anat 2014;36:209-17. [Crossref] [PubMed]
- Yang SM, Lo CM. A man with a fracture from minor trauma. World J Emerg Med 2014;5:306-9. [Crossref] [PubMed]
- Monica J, Vredenburgh Z, Korsh J, Gatt C.. Acute Shoulder Injuries in Adults. Am Fam Physician 2016;94:119-27. [PubMed]
- Bae DS, Kocher MS, Waters PM, Micheli LM, Griffey M, Dichtel L. Chronic recurrent anterior sternoclavicular joint instability: results of surgical management. J Pediatr Orthop 2006;26:71-4. [Crossref] [PubMed]
- Cope R.. Dislocations of the sternoclavicular joint. Skeletal Radiol 1993;22:233-8. [Crossref] [PubMed]
- Benitez CL, Mintz DN, Potter HG. MR imaging of the sternoclavicular joint following trauma. Clin Imaging 2004;28:59-63. [Crossref] [PubMed]
- ElMaraghy AW, Devereaux MW. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg 2012;21:412-22. [Crossref] [PubMed]
- Hasegawa K, Schofer JM. Rupture of the pectoralis major: a case report and review. J Emerg Med 2010;38:196-200. [Crossref] [PubMed]
- Lee YK, Skalski MR, White EA, Tomasian A, Phan DD, Patel DB, Matcuk GR Jr, Schein AJ. US. Radiographics 2017;37:176-189. [Crossref] [PubMed]
- Pavlik A, Csépai D, Berkes I. Surgical treatment of pectoralis major rupture in athletes. Knee Surg Sports Traumatol Arthrosc 1998;6:129-33. [Crossref] [PubMed]
- Lee SJ, Jacobson JA, Kim SM, Fessell D, Jiang Y, Girish G, Magerkurth O. Distal pectoralis major tears: sonographic characterization and potential diagnostic pitfalls. J Ultrasound Med 2013;32:2075-81. [Crossref] [PubMed]
- Weaver JS, Jacobson JA, Jamadar DA, Theisen SE, Ebrahim F, Kalume-Brigido M. Sonographic findings of pectoralis major tears with surgical, clinical, and magnetic resonance imaging correlation in 6 patients. J Ultrasound Med 2005;24:25-31. [Crossref] [PubMed]
- Otoshi K, Itoh Y, Tsujino A, Hasegawa M, Kikuchi S. Avulsion injury of the serratus anterior muscle in a high-school underhand pitcher: a case report. J Shoulder Elbow Surg 2007;16:e45-7. [Crossref] [PubMed]
- Friedman MV, Stensby JD, Hillen TJ, Demertzis JL, Keener JD. Traumatic Tear of the Latissimus Dorsi Myotendinous Junction: Case Report of a CrossFit-Related Injury. Sports Health 2015;7:548-52. [Crossref] [PubMed]
- Tomas X, Peidro L, Ortiz J, Pomes J, Cores E, Garcia AI, Bianchi L. Simultaneous muscle strain at the point of attachment to the scapula of the rotator cuff muscles: MRI findings. Clin Radiol 2004;59:621-4. [Crossref] [PubMed]
- Black J, Baharestani M, Cuddigan J, Dorner B, Edsberg L, Langemo D, Posthauer ME, Ratliff C, Taler G. National Pressure Ulcer Advisory Panel. National Pressure Ulcer Advisory Panel's updated pressure ulcer staging system. Dermatol Nurs 2007;19:343-9. [PubMed]
- Quintavalle PR, Lyder CH, Mertz PJ, Phillips-Jones C, Dyson M. Use of high-resolution, high-frequency diagnostic ultrasound to investigate the pathogenesis of pressure ulcer development. Adv Skin Wound Care 2006;19:498-505. [Crossref] [PubMed]
- Ohura T, Ohura N Jr, Oka H.. Incidence and Clinical Symptoms of Hourglass and Sandwich-shaped Tissue Necrosis in Stage IV Pressure Ulcer. Wounds 2007;19:310-9. [PubMed]
- Linder-Ganz E, Shabshin N, Gefen A. Patient-specific modeling of deep tissue injury biomechanics in an unconscious patient who developed myonecrosis after prolonged lying. J Tissue Viability 2009;18:62-71. [Crossref] [PubMed]
- Agam L, Gefen A. Pressure ulcers and deep tissue injury: a bioengineering perspective. J Wound Care 2007;16:336-42. [Crossref] [PubMed]


