Esophageal bezoar after repeated fundoplications
Bezoars are conglomerates of indigestible material that is ingested, trapped in the gastrointestinal tract. Concerning the material that ingredients the bezoar they can be divided into four types: phytobezoars, trichobezoars, pharmacobezoars and lactobezoars (1). The main reason for formation of esophageal bezoar is malfunction of lower esophageal sphincter, motility disorders or structural abnormalities including lower esophageal stenosis (2). Various management strategies have been proposed including endoscopic fragmentation and extraction (3-6), pancreatic enzymes and Coca-Cola digestion (4-6), and in refractory case surgical removal (3,6).
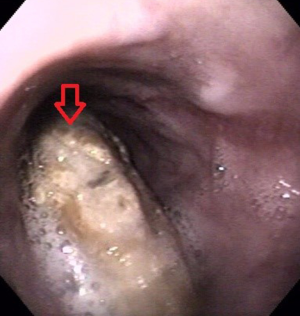
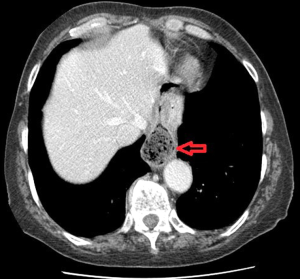
A 65-year-old female patient with type 3 hiatal hernia underwent open Nissen fundoplication. One year after the initial operation Nissen fundoplication was converted to Toupett due to twist of the fundoplication and complaints of disphagia. One year after Toupett fundoplication patient was referred to our clinic with complaints of disphagia and odynophagia. CT scan and esophagogastroscopy were performed. CT scan revealed dilated lower esophagus and particulate feculent like mass mingled with gas bubbles in the lumen of the esophagus (Figure 1). On endoscopy a greeny-brown soft mass was found in lower esophagus (Figure 2). The endoscope easily passed around the mass and entered the stomach founding no signs of structural abnormalities of the gastro-esophageal junction. The bezoar was endoscopically fragmentated using 4-prong grasping forceps, after unsuccessful attempt of extraction due to soft consistence of bezoar. After the endoscopy patient was given Coca-Cola in attempt to dissolve the particles of the bezoar left in the esophagus as proposed by Ladas et al. (5). Coca-Cola is believed to break the bezoar to fine particles which facilitate extraction or even full bezoar dissolution (1). Follow up endoscopy one month after the fragmentation of bezoar showed no evidence of foreign body in esophagus neither in the stomach. The patient was advised to drink enough amounts of water at home.
Fore gut bezoars, especially esophageal ones are extremely rare clinical entity. Very few case reports describe esophageal bezoars, and as far as we know this is the first described case of esophageal bezoar after hiatal hernia procedures. Most of the published cases present critically ill patients on enteral feeding via nasogastric tube (7). There are reports of bezoars formed after vagotomy and or pyloroplasty, but the bezoars were formed in the stomach (8). The main reason for formation of bezoars is presumed to be motility disorders—including achalasia, diffuse esophageal spasm, progressive systemic sclerosis, Guillain-Barre syndrome and myasthenia gravis (2). Dysfunction of lower esophageal sphincter seems to play important role in the formation of esophageal bezoar. Another pathogenic mechanism for esophageal bezoars formation is described by Pitiakoudis et al. as initial formation in the stomach, and then after continuous vomiting and fragmentation of bezoar, migration of part of the bezoar to the esophagus (8). In our case a possible mechanism for formation of bezoar is repeated surgical interventions in cardio-esophageal junction leading to dense adhesions in that region and altering peristalsis of lower esophagus. This hypothesis was presumed because of the lack of any structural abnormality that may cause stricture on esophagogastroscopy. A potential weakness of our study is the lack of esophageal manometry and barium contrast esophagography, which we decided to perform if recurrence occurs on follow up.
In conclusion a case of esophageal bezoar is described in patient with repeated cardioesophageal procedures for hiatal hernia. Esophageal bezoar should be excluded when patient with hiatal hernia surgeries present with disphagia and odynophagia. Endoscopic fragmentation and extraction are the first line treatments during diagnostic endoscopy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this article and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Iwamuro M, Okada H, Matsueda K, Inaba T, Kusumoto C, Imagawa A, Yamamoto K. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc 2015;7:336-45. [PubMed]
- Kim KH, Choi SC, Seo GS, Kim YS, Choi CS, Im CJ. Esophageal bezoar in a patient with achalasia: case report and literature review. Gut Liver 2010;4:106-9. [PubMed]
- Turner JS, Fyfe AR, Kaplan DK, Wardlaw AJ. Oesophageal obstruction during nasogastric feeding. Intensive Care Med 1991;17:302-3. [PubMed]
- Gupta R, Share M, Pineau BC. Dissolution of an esophageal bezoar with pancreatic enzyme extract. Gastrointest Endosc 2001;54:96-9. [PubMed]
- Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol 2002;14:801-3. [PubMed]
- Yaqub S, Shafique M, Kjæstad E, Thorsen Y, Lie ES, Dahl V, Bakka N, Røkke O. A safe treatment option for esophageal bezoars. Int J Surg Case Rep 2012;3:366-7. [PubMed]
- Marcus EL, Arnon R, Sheynkman A, Caine YG, Lysy J. Esophageal obstruction due to enteral feed bezoar: A case report and literature review. World J Gastrointest Endosc 2010;2:352-6. [PubMed]
- Pitiakoudis M, Tsaroucha A, Mimidis K, Constantinidis T, Anagnostoulis S, Stathopoulos G, Simopoulos C. Esophageal and small bowel obstruction by occupational bezoar: report of a case. BMC Gastroenterol 2003;3:13. [PubMed]