
Prenatal diagnosis of umbilical cord true knot using high-definition flow (HD-flow) render mode and spatio-temporal image correlation: a case series
Introduction
True knot of umbilical cord is a rare condition with a 4-fold high fetal mortality rate compared with that of normal fetuses. Women with this condition are associated with increased fetal heart rate and cesarean section rate (1). The risk factors of true knot for umbilical cord include long umbilical cords (>80 cm), polyhydramnios, gestational diabetes, male fetus, and amniocentesis (2,3). True knot of umbilical cord can be diagnosed with two-dimensional (2D) ultrasound and color Doppler ultrasound (1-3). However, it is difficult to distinguish false knots from true knots of the umbilical cord.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patients for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
In this study, ultrasound examinations were performed using the E10 system (GE Healthcare, Chicago, IL, USA) with an abdominal volume probe operating at 3.0–5.0 MHz. The high-definition flow (HD-flow) render mode combined with spatio-temporal image correlation (STIC) enabled detailed visualization of the umbilical cord’s vascular architecture, facilitating precise identification of true knots.
Case 1
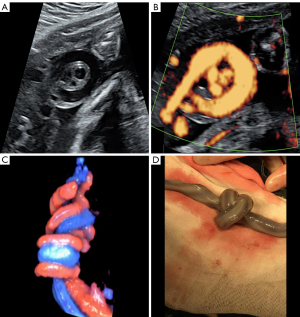
A 28-year-old pregnant woman, gravida 1, para 0, underwent routine ultrasound examination. Umbilical cord abnormality was detected during routine ultrasound at 32 weeks of gestational age. 2D ultrasound and energy Doppler blood flow showed a hanging noose sign (Figure 1A,1B). Three-dimensional (3D) ultrasound was employed to diagnose true knot of umbilical cord by using HD-flow render mode with STIC (Figure 1C). In addition, routine ultrasound examination and electronic fetal monitoring were performed once a week. The last ultrasound at 36+5 weeks’ gestational age showed an increased umbilical artery index. A cesarean section was performed upon the request of the pregnant woman. A healthy male neonate weighing 3,750 g was delivered. A true knot of umbilical cord was observed in the middle of the umbilical cord (Figure 1D).
Case 2
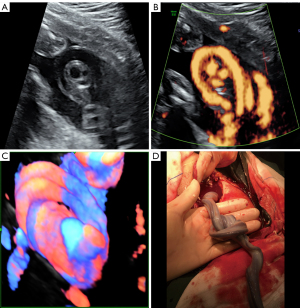
A 24-year-old maternity, gravida 1, para 0, underwent routine ultrasound examination at 27 weeks of gestation. 2D ultrasound and energy Doppler blood flow revealed a hanging noose sign (Figure 2A,2B). A further HD-flow render mode with STIC confirmed the existence of a true knot of the umbilical cord (Figure 2C). Routine ultrasound examination and electronic fetal monitoring were performed on a weekly basis thereafter. A cesarean section was performed at 39+1 weeks upon request by the pregnant woman. A healthy male infant weighing 2,700 g was successfully delivered. A true knot of the umbilical cord was seen in the middle of the umbilical cord (Figure 2D).
Case 3
A 31-year-old maternity, gravida 2, para 1, underwent routine ultrasound examination at 32 weeks of gestational age. 2D ultrasound and color blood flow scan were conducted, which revealed a true knot on the umbilical cord (Figure 3A,3B). No significant infarct was seen in the placenta on ultrasound images. Thus, a 3D ultrasound was performed to confirm the diagnosis (Figure 3C). Routine ultrasound examination and electronic fetal monitoring were conducted weekly. At 37+3 weeks, the woman requested a cesarean section due to preterm premature rupture of membranes. A healthy male neonate weighing 2,840 g was successfully delivered. A true knot of the umbilical cord was observed on the fetal side (Figure 3D). After the provision of written informed consent, a pathological examination of the placenta and umbilical cord was performed. Analysis of the umbilical cord image showed that the diameter of the umbilical vein was dilated both at the knot and distal of the knot (Figure 4A,4B), and the umbilical arteries were slightly occluded (Figure 4C,4D). Moreover, the placenta images exhibited villous dysplasia (Figure 4E), chorionic hyperemia (Figure 4F), choriocytoma (Figure 4G), and inflammatory cell infiltration in the fetal membrane (Figure 4H).
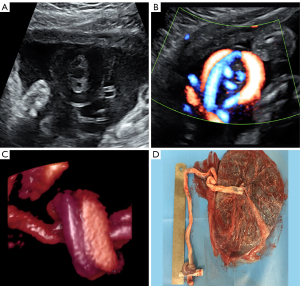
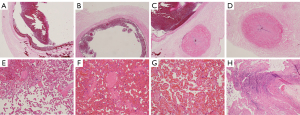
Table 1 shows the characteristics, and basic clinical information and high-risk factors of the three cases.
Table 1
| Case number | UC length (cm) | Amniotic fluid (cm) | Gestational diabetes | Gender | Birth weight (g) | Amniocentesis |
|---|---|---|---|---|---|---|
| 1 | 72 | 4.9 | No | Male | 3,750 | No |
| 2 | 67 | 3.7 | No | Male | 2,700 | Yes |
| 3 | 59 | 6.0 | No | Male | 2,840 | No |
UC, umbilical cord.
Discussion
Modern ultrasound can reveal a true knot of the umbilical cord. Ramón et al. reported for the first time the diagnosis of umbilical cord true knot based on typical 2D images of the hanging noose sign of color blood flow (4). 3D-HD-flow and spectrum of the umbilical artery were conducted to confirm the diagnosis of umbilical cord true knot for the first time (3). The authors believed that the 3D-HD-Flow improved the diagnostic accuracy of umbilical cord true knot. Previously, Gurau et al. used 2D and 3D ultrasound examination for the first time to diagnose complex true knot of umbilical cord (5). Notably, 3D ultrasound, particularly when combined with HD-flow and STIC, improves diagnostic accuracy in differentiating true knots from false knots (6). However, maternal and fetal variables—such as maternal body habitus, fetal position, or excessive fetal movement—may occasionally limit visualization, as reported in studies where diagnostic confidence varied depending on technical conditions (7,8). In our cohort, optimal imaging conditions (e.g., adequate amniotic fluid volume, cooperative fetal positioning) allowed consistent identification of true knots. Our three true knots of the umbilical cord were detected during routine ultrasound examination, and a typical hanging noose sign was seen. One case showed an increased umbilical artery index in the last ultrasound examination. In the three cases, HD-flow with STIC 3D images of umbilical cord true knots were recorded.
Although prenatal diagnosis of umbilical cord true knots has been previously reported, our study underscores the value of integrating HD-flow render mode with STIC to enhance diagnostic precision and 3D visualization. This combined approach allows for better differentiation between true and false knots, a challenge noted in earlier studies (6).
In our clinical practice, routine ultrasound examinations include targeted evaluation of the umbilical cord when anomalies (e.g., abnormal Doppler findings, polyhydramnios, or fetal growth restriction) are suspected. Universal screening for true knots is not currently standard; however, our cases suggest that in high-risk pregnancies (e.g., long cord, male fetus, or prior amniocentesis), systematic protocols—such as 3D-HD-flow with STIC—could improve detection. Cost-effectiveness hinges on risk stratification, as weekly scans are resource-intensive. In our cohort, early identification enabled timely monitoring, potentially averting adverse outcomes. Further studies are needed to validate systematic screening guidelines.
Although previous reports have associated umbilical cord true knots with intrauterine distress (1), our cases exhibited no such complications, likely due to vigilant monitoring and the protective role of Wharton’s jelly. This underscores the importance of individualized surveillance rather than universal intervention. True knots of the umbilical cord can decrease the Apgar scores of neonates and increase the neonatal intensive care unit (NICU) admission rate (7). However, other studies have shown that umbilical cord true knots and postpartum outcomes are not unrelated (8). In the present cases, routine ultrasound examination and electronic fetal monitoring were performed weekly until abnormal spectrum of umbilical artery or abnormal fetal electronic monitoring. Therefore, we suggest that umbilical artery spectrum and electronic monitoring can be used dynamically to observe the intrauterine condition of umbilical cord true knots in fetuses. In the three cases, all fetuses showed good outcomes because the Wharton’s jelly protected the umbilical cord to ensure sufficient blood flow in the umbilical cord. Therefore, we recommend weekly ultrasound examinations only after a true knot is confirmed, focusing on placental perfusion and umbilical artery indices. This targeted approach balances resource utilization with the need to detect secondary complications (e.g., placental infarction), as observed in Case 3.
In our cases, the length of umbilical cord was less than 80 cm, the amniotic fluid was normal, and none of the three cases had diabetes. One case required amniocentesis and three cases were male fetuses. It is likely that in our cases, the amniocentesis and being a male infant may be a risk factor for umbilical cord true knots.
True umbilical cord knots are associated with several risk factors, including long umbilical cords (>80 cm), polyhydramnios, male fetuses, and maternal procedures such as amniocentesis (1-3). These factors may increase cord mobility or alter intrauterine dynamics, predisposing to knot formation. Notably, in our series, two cases involved male fetuses, and one had a history of amniocentesis, aligning with prior epidemiological observations (1).
The number of knots may further influence fetal outcomes. Although single knots (as observed in our cases) may remain asymptomatic due to compensatory mechanisms (e.g., Wharton’s jelly protection), multiple knots or tight knots can compromise blood flow, leading to fetal hypoxia or intrauterine demise. A meta-analysis by Räisänen et al. [2013] reported that neonates with multiple knots had significantly lower Apgar scores and higher NICU admission rates compared to those with single knots (7). Although our cases exhibited favorable outcomes, clinicians should remain vigilant in pregnancies involving multiple umbilical cord knots, as they may necessitate more intensive surveillance.
Studies have shown that a true knot of umbilical cord can lead to placental infarction (9). Pathological examination of the placenta and umbilical cord was performed in one case. Moreover, the umbilical vein was dilated and the umbilical arteries were slightly occluded, accompanied by pathological changes such as villous dysplasia in the placenta. Thus, routine ultrasound examination should be conducted to identify placental infarction or severe occlusion of the umbilical artery weekly when a true knot of umbilical cord is detected during pregnancy.
Conclusions
This case series highlights the diagnostic utility of combining HD-flow render mode with STIC in the prenatal identification of true umbilical cord knots. The integration of these advanced ultrasound techniques not only enhances spatial visualization but also improves differentiation between true and false knots, addressing a persistent challenge in prenatal imaging. Our findings demonstrate that vigilant monitoring—specifically weekly ultrasound examinations focusing on placental perfusion and umbilical artery indices following a confirmed diagnosis—can contribute to favorable fetal outcomes, as evidenced by the three cases presented.
Although universal screening for umbilical cord true knots remains impractical due to their low prevalence, our study underscores the value of targeted evaluations in high-risk pregnancies (e.g., long umbilical cords, male fetuses, or prior amniocentesis). The proposed risk-stratified protocol, incorporating 2D ultrasound, 3D-HD-flow/STIC confirmation, and longitudinal hemodynamic assessments, offers a balanced approach to resource utilization and clinical efficacy.
Notably, despite previous associations between true knots and intrauterine distress, none of our cases exhibited such complications, likely attributable to the protective role of Wharton’s jelly and proactive surveillance. Future research should validate these protocols in larger cohorts and explore cost-effectiveness in diverse clinical settings. This study reinforces the importance of individualized management and technological advancements in optimizing prenatal care for umbilical cord anomalies.
Acknowledgments
None.
Footnote
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-2421/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patients for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hershkovitz R, Silberstein T, Sheiner E, Shoham-Vardi I, Holcberg G, Katz M, Mazor M. Risk factors associated with true knots of the umbilical cord. Eur J Obstet Gynecol Reprod Biol 2001;98:36-9. [Crossref] [PubMed]
- Sørnes T. Umbilical cord knots. Acta Obstet Gynecol Scand 2000;79:157-9. [Crossref] [PubMed]
- Rodriguez N, Angarita AM, Casasbuenas A, Sarmiento A. Three-dimensional high-definition flow imaging in prenatal diagnosis of a true umbilical cord knot. Ultrasound Obstet Gynecol 2012;39:245-6. [Crossref] [PubMed]
- Ramón Y, Cajal CL, Martínez RO. Prenatal diagnosis of true knot of the umbilical cord. Ultrasound Obstet Gynecol 2004;23:99-100. [Crossref] [PubMed]
- Gurau D, Zaltz A, Yoo WK, Rahmani MR. All Tied Up and Nowhere to Go: Report of a Figure-eight Umbilical Cord Complex True Knot and Triple Nuchal Cord Detected on Antenatal Sonography. J Ultrasound Med 2016;35:1361-3. [Crossref] [PubMed]
- Merz E, Pashaj S. True or false umbilical cord knot? Differentiation via 3D/4D color Doppler ultrasound. Ultraschall Med 2018;39:127-8. [Crossref] [PubMed]
- Räisänen S, Georgiadis L, Harju M, Keski-Nisula L, Heinonen S. True umbilical cord knot and obstetric outcome. Int J Gynaecol Obstet 2013;122:18-21. [Crossref] [PubMed]
- Carter EB, Chu CS, Thompson Z, Tuuli MG, Macones GA, Cahill AG. True knot at the time of delivery: electronic fetal monitoring characteristics and neonatal outcomes. J Perinatol 2018;38:1620-4. [Crossref] [PubMed]
- Hasegawa J, Furuya N, Doi M, Sasaki T, Takagi M, Suzuki N. Sono-embryological assessments of a true knot that developed into a hypercoiled cord and circumvallate placenta. J Matern Fetal Neonatal Med 2021;34:4162-6. [Crossref] [PubMed]


