
Huge trichobezoar resulting in gastrointestinal obstruction: a case description of Rapunzel syndrome
Introduction
Rapunzel syndrome is a rare entity characterized by a gastric trichobezoar that possesses a long tail extending into the small intestine. It primarily affects young women who have underlying psychiatric disorders, particularly those with a history of trichotillomania and trichophagia. We present a case involving a young woman who exhibited a trichobezoar causing gastrointestinal obstruction. The endoscopic fragmentation of the large and dense trichobezoar presents considerable difficulties, thereby necessitating surgical intervention for the removal of these masses.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institution and with the Declaration of Helsinki and its subsequent amendments. Written informed consent was obtained from the patient’s father for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Rapunzel syndrome is characterized as a rare form of gastric trichobezoar, distinguished by a long tail that extends into the small intestine, predominantly affecting young female children. We present a case involving a 15-year-old female patient with a three-year history of trichotillomania and trichophagia. This behavior was carried out behind the parents’ backs. The parents remained unaware of these behaviors until the patient experienced significant abdominal pain one week prior to presentation. Upon examination, the patient exhibited increased abdominal distension, anorexia, vomiting, diarrhea, and weight loss, with a body mass index (BMI) of 16.7 kg/m2, categorizing her as underweight. Clinical assessment revealed marked asthenia and dehydration, alongside a well-defined intra-abdominal mass located in the epigastric region. Laboratory results indicated mild leukocytosis and a slight elevation in platelet count, while all other values remained within normal limits.
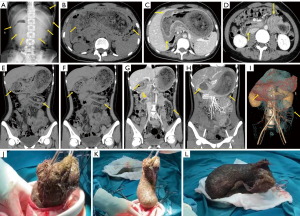
The abdominal radiograph shows the stomach filled with a huge soft tissue density of solid mass (yellow arrow, Figure 1A). An abdominal computed tomography (CT) scan with image reconstruction (Figure 1B-1I) was subsequently performed, revealing severe dilation of the proximal gastroduodenum and jejunum, as well as the presence of a heterogeneous, solid mass measuring 12.8 cm × 23.5 cm. Additionally, edema and thickening of the gastrointestinal wall were noted (yellow arrow, Figure 1B-1H), accompanied by peri-intestinal exudation. These findings raised suspicion of trichobezoar and intestinal obstruction. The patient was referred for surgical evaluation, leading to a median celiotomy and gastrotomy due to the progressive abdominal pain and the considerable size of the mass. A substantial trichobezoar was successfully excised from the stomach and proximal jejunum (Figure 1J-1L).
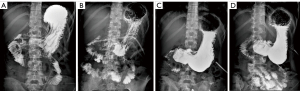
Twelve days post-surgery, the patient underwent an upper gastrointestinal (UGI) series to evaluate gastric motility, which indicated that the iohexol contrast was progressing too slowly into the bowel (Figure 2A,2B). Following this, the patient participated in a two-week acupuncture treatment program, and 26 days after the procedure, a follow-up UGI gastroenterography was conducted. Scintigraphic imaging (Figure 2C,2D) demonstrated no delayed gastric emptying. The patient was subsequently discharged from the hospital without complications. She received psychological counseling, and during annual follow-up visits three years post-surgery, it was observed that the patient had ceased the ingestion of hair, with her BMI returning to the normal range.
Discussion
A bezoar is defined as a mass of undigested material that accumulates within the gastrointestinal tract. It can be composed of various substances, including hair (trichobezoar), plant fibers (phytobezoar), concentrated milk formula (lactobezoar), mixed medications (pharmacobezoar), or stones (lithobezoar) (1). Trichotillomania, a psychiatric disorder, is characterized by the compulsive and repetitive act of pulling out one’s own hair. The subsequent ingestion of the pulled hair is referred to as trichophagia (2). It is imperative to closely monitor the mental health of adolescents, particularly in cases where individuals, such as the patient in this instance, experience significant stress due to demanding academic pressures over an extended period. Additionally, a lack of effective communication with parents and an unnecessary increase in study time may exacerbate the situation. This study seeks to enhance awareness of trichobezoars, with the intention of facilitating early diagnosis and intervention.
Trichobezoars typically present as asymptomatic abdominal masses initially; however, due to their indigestible nature and continuous growth, they can lead to symptoms such as abdominal pain, nausea, weight loss, and malnutrition. When a trichobezoar extends into the jejunum, ileum, or colon, it is referred to as Rapunzel syndrome. The term “Rapunzel syndrome” is derived from the Brothers Grimm fairy tale, which features a young princess who escapes from a tower with the aid of her long hair (3).
Rapunzel syndrome is an exceedingly rare condition predominantly observed in young females aged between 3 and 19 years. It is associated with psychiatric disorders and cognitive impairments (4). Severe complications arising from this condition may include intestinal obstruction, peritonitis, perforation, gastrointestinal bleeding, intussusception, pancreatitis, and cholangitis (5).
Accurate diagnosis and prompt treatment are essential. The most effective diagnostic approaches for trichobezoars include UGI endoscopy and various imaging techniques, such as plain radiography, barium meal studies, ultrasound, and CT. A UGI X-ray is a safe and precise diagnostic tool that offers detailed imaging and real-time dynamic visualization of the entire gastrointestinal tract. CT is particularly favored for patients presenting to emergency departments with unexplained abdominal pain, as it demonstrates greater accuracy than barium meal studies and ultrasound in identifying concurrent gastric and intestinal bezoars, as well as in assessing the level and severity of gastrointestinal obstruction (6). Key CT findings typically include the presence of a heterogeneous bezoar, gastrointestinal tract dilation, edema and thickening of the gastrointestinal wall, and peri-intestinal exudation.
The primary treatment for trichobezoars involves the complete removal of the mass and the prevention of recurrence. Various surgical methods can be employed, including laparotomy, laparoscopy, and endoscopic removal. Endoscopic and laparoscopic techniques are generally preferred due to their associated benefits, which include reduced pain, shorter hospital stays, fewer adverse events, and lower rates of postoperative complications compared to laparotomy for smaller lesions (7). However, open gastrotomy remains the most effective approach for the removal of large trichobezoars and for evaluating potential satellite lesions in the small intestine (8). The selection of the surgical method for trichobezoar removal is influenced by factors such as the location and size of the mass, as well as the operator’s expertise, which plays a critical role in the success of the procedure.
Gastrointestinal motility disorders, which encompass conditions such as functional dyspepsia and gastroparesis, significantly hinder postoperative recovery in patients with trichobezoars (4). The most effective way to assess gastric motility is to measure the gastric emptying time using a barium swallow test and scintigraphy (9). The primary approach to managing gastric motility disorders includes dietary modifications, followed by pharmacological interventions, and, when necessary, surgical procedures. Acupuncture has emerged as a promising treatment modality for gastrointestinal disorders. Our case study demonstrates that acupuncture effectively enhances gastric motility and ameliorates delayed gastric emptying in patients with gastroparesis. Rabitti et al. have provided conclusive evidence that acupuncture treatment alleviates the symptoms associated with gastroparesis (10). Nonetheless, additional research is warranted to further substantiate the efficacy of this traditional therapeutic technique.
Rapunzel syndrome is an exceedingly rare condition in young women, frequently linked to psychiatric disorders. Diagnosis can be established through a history of trichophagia and appropriate imaging techniques. Postoperative acupuncture may offer benefits in improving gastric motility, while psychological counseling is essential for mitigating the risk of recurrence.
Acknowledgments
None.
Footnote
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-2024-2702/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and with the Declaration of Helsinki and its subsequent amendments. Written informed consent was obtained from the patient’s father for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gonuguntla V, Joshi DD. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res 2009;7:99-102. [Crossref] [PubMed]
- Balawender K, Pliszka A, Możdżeñ K, Kłos M, Ogorzałek A, Boroñ D, Grabarek BO. Trichopsychodermatology: trichotillomania and trichophagia leading to Rapunzel syndrome. Postepy Dermatol Alergol 2022;39:739-43. [Crossref] [PubMed]
- Vaughan ED Jr, Sawyers JL, Scott HW Jr. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery 1968;63:339-43. [PubMed]
- Kim SC, Kim SH, Kim SJ. A Case Report: Large Trichobezoar Causing Rapunzel Syndrome. Medicine (Baltimore) 2016;95:e3745. [Crossref] [PubMed]
- Delimpaltadaki DG, Gkionis IG, Flamourakis ME, Strehle AF, Bachlitzanakis EN, Giakoumakis MI, Christodoulakis MS, Spiridakis KG. A rare giant gastric trichobezoar in a young female patient: Case report and review of the literature. Clin Case Rep 2021;9:e05152. [Crossref] [PubMed]
- García-Ramírez BE, Nuño-Guzmán CM, Zaragoza-Carrillo RE, Salado-Rentería H, Gómez-Abarca A, Corona JL. Small-Bowel Obstruction Secondary to Ileal Trichobezoar in a Patient with Rapunzel Syndrome. Case Rep Gastroenterol 2018;12:559-65. [Crossref] [PubMed]
- Lisi D, D'Ovidio V, Lucidi C. A Giant Trichobezoar Diagnosed by Ultrasound, Confirmed by Upper Endoscopy, and Managed by Minimally Invasive Laparoscopic Surgery. Clin Gastroenterol Hepatol 2021;19:e125. [Crossref] [PubMed]
- Wang L, Chen Y, Chen S, Gao Z, Qian Y, Chen Q. Gastrointestinal trichobezoars in the pediatric population: a retrospective study. BMC Pediatr 2024;24:124. [Crossref] [PubMed]
- Keller J, Bassotti G, Clarke J, Dinning P, Fox M, Grover M, Hellström PM, Ke M, Layer P, Malagelada C, Parkman HP, Scott SM, Tack J, Simren M, Törnblom H, Camilleri MInternational Working Group for Disorders of Gastrointestinal Motility and Function. Expert consensus document: Advances in the diagnosis and classification of gastric and intestinal motility disorders. Nat Rev Gastroenterol Hepatol 2018;15:291-308. [Crossref] [PubMed]
- Rabitti S, Giovanardi CM, Colussi D. Acupuncture and Related Therapies for the Treatment of Gastrointestinal Diseases. J Clin Gastroenterol 2021;55:207-17. [Crossref] [PubMed]


