
Rare diagnosis of prenatal persistent vitelline artery with spatiotemporal image correlation and high-definition flow: a case description
Introduction
The human umbilical cord typically comprises two arteries and one vein. Single umbilical artery (SUA), a condition characterized by the absence of one umbilical artery, occurs in approximately 1% of pregnancies and is detectable through routine prenatal ultrasound examinations. Blackburn and Cooley proposed a classification system in which type II SUA is defined as a bilateral absence or interruption of the umbilical artery accompanied by a persistent vitelline artery (1). The persistent vitelline artery is considered a compensatory mechanism, providing vascular support and assuming the function of the absent umbilical artery. However, this anomaly is implicated in the pathogenesis of severe malformations such as sirenomelia, limb-body wall defect, and omphalocele-exstrophy-imperforate anus-spinal defect (OEIS) complex (2,3). Here, we present a case of type II SUA with a favorable neonatal outcome following prenatal diagnosis in a normally developing fetus.
Case presentation
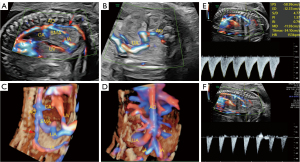
At 24 weeks of gestation, a 29-year-old pregnant woman was referred for further evaluation due to abnormal findings in routine ultrasound, revealing anomalous abdominal vasculature. Color Doppler imaging indicated the absence of umbilical arteries on both sides of the bladder. Sagittal views revealed an artery in the umbilical cord originating abnormally from the superior mesenteric artery, with a markedly thinner diameter of the abdominal aorta below the superior mesenteric artery (Figure 1A,1B, Video 1). Spatial relationships were vividly visualized with four-dimensional (4D) color Doppler with spatiotemporal image correlation (STIC) and high-definition flow (HD-flow) render mode (Voluson E10; GE Healthcare, Chicago, IL, USA) (Figure 1C,1D, Video 2). Abnormal vessels on pulse Doppler ultrasound images resembled normal umbilical arteries, but the abdominal aorta below the superior mesenteric artery showed a lack of diastolic blood flow signal (Figure 1E,1F). In a subsequent ultrasound examination during pregnancy, the length of both lower limbs, kidney size, and amniotic fluid volume of the fetus were all within the normal range, and the patient was followed up until the birth of the fetus.
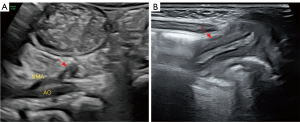
A male infant was delivered vaginally at 39+4 weeks of gestational age with a birth weight of 3,050 g. Ultrasound scanning of the abdomen on the second day of life confirmed an atretic vessel connecting the superior mesenteric artery to the navel, with no blood flow signals inside the vessel (Figure 2). During a 12-month follow-up, the infant remained asymptomatic.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient’s legal guardian for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Primitive umbilical vessels originate from the arterioles of the urinary bladder and the yolk sac, receding by the end of the third month. As the yolk sac atrophies, yolk circulation weakens and eventually ceases, while the umbilical artery, derived from the urachal artery, transports an increasing amount of blood to the placenta. The bilateral absence or interruption of the umbilical arteries with persistent yolk arteries is classified as type II SUA. This anomaly arises from the descending aorta high in the abdominal cavity, redirecting blood flow from developing caudal structures of the embryo to the placenta. The persistent vitelline artery, a large artery originating from the abdominal aorta or superior mesenteric artery, compensates for the absence of bilateral umbilical arteries by transporting nutrients to the caudal and distal parts of the embryo. The persistent vitelline artery possesses a distinct internal elastic lamina, which is usually absent in normal umbilical arteries (4). Termed vitelline artery steal, this phenomenon is implicated in the pathogenesis of distal-associated-organ and soft-tissue defects due to the diversion of a significant amount of blood from the abdominal aorta into the placenta (5).
After prenatal diagnosis, it is essential to conduct an enhanced fetal anatomy scan to thoroughly examine the caudal region due to its association with sirenomelia, caudal regression, and anal agenesis. Following birth, long-term follow-up is imperative for children with type II SUA. Attention should be focused on the formation of a persistent embryonic yolk tube following the closure of the vitelline artery. There may be a variety of clinical manifestations, including asymptomatic or atypical presentations, or associated acute intestinal obstruction, recurrent intestinal pain, or intraabdominal hemorrhage (6).
In the case reported here, ultrasonography at 24 weeks of gestation revealed an umbilical artery originating from the beginning of the abdominal aorta. Coronal views showed a markedly thinner internal diameter of the distal segment of the abdominal aorta branching off from the anomalous vessel. However, there was no evidence of serious blood supply deficiency below the level of the anomalous vessel or to the distal organs. Several cases of type II SUA with favorable outcomes have been reported, where a thinner aorta below the vitelline artery was observed despite the presence of a steal phenomenon (7). In these cases, a thinner aorta below the vitelline artery was observed despite the steal phenomenon. In our case, throughout the entire pregnancy, the fetal renal artery, femoral artery, and amniotic fluid volume remained within normal ranges, possibly due to the shunt volume being insufficiently large to cause serious structural issues.
Compared to two-dimensional ultrasound, 4D color Doppler with STIC and HD-flow mode can comprehensively and clearly display the origin, course, and relationship between the vitelline artery and descending aorta. This is advantageous for clinicians and patients in gaining a better understanding of the disease’s severity, greatly aiding in prenatal management guidance. However, this technique is often hindered by the fetal position and the high fat content of the pregnant woman, which can result in incomplete imaging for some patients.
Early detection by fetal ultrasound has several clinical implications: (I) application of 4D color Doppler with STIC HD-flow mode facilitates the display of spatial relationships between the abdominal aorta and SUA. (II) Fetal karyotype analysis and genetic testing is recommended in cases of associated malformations. (III) Diagnosis of SUA syndrome should prompt an exhaustive fetal morphology scan, and fetal lower-limb development and amniotic fluid volume should be monitored dynamically throughout the fetal period. (IV) Long-term follow-up is essential, particularly when a ligament formed by the persistent vitelline artery after atresia leads to intestinal torsion and malrotation.
Conclusions
This report presents an extremely rare case of type II SUA accompanied by a persistent vitelline artery, resulting in a favorable neonatal outcome. Postnatally, long-term follow-up is imperative for the management of children with type II SUA.
A thorough understanding of the embryological and ultrasound characteristics of the vitelline artery can assist in the early and accurate diagnosis of this condition. Prenatal diagnosis plays a pivotal role in enabling early clinical and imaging assessments. In this instance, prenatal ultrasound via 4D color Doppler with STIC HD-flow mode facilitated the visualization of the spatial relationship between the persistent vitelline artery and the abdominal aorta. Some cases may present with various complications, asymptomatic or atypical, or have associated acute intestinal obstruction, recurrent intestinal pain, or intra-abdominal hemorrhage. Postnatally, long-term follow-up is imperative for the management of children with type II SUA.
Acknowledgments
None.
Footnote
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-159/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient’s legal guardian for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Blackburn W, Cooley W. Human malformations and related anomalies. New York: Oxford University Press; 1993.
- Gámez F, De León-Luis J, Bravo C, Pintado P, Ruiz Y, Palomo S, Pérez R, Ortiz-Quintana L. Prenatal diagnosis of Type II single umbilical artery (persistent vitelline artery) in a normal fetus. Ultrasound Obstet Gynecol 2013;41:593-4.
- Lecoquierre F, Brehin AC, Coutant S, Coursimault J, Bazin A, Finck W, et al. Exome sequencing identifies the first genetic determinants of sirenomelia in humans. Hum Mutat 2020;41:926-33.
- Bravo C, De León-Luis J, Gámez F, Ruiz Y, Pintado P, Pérez R, Ortiz-Quintana L. Fetal MRI as a complementary technique after prenatal diagnosis of persistent vitelline artery in an otherwise normal fetus. J Magn Reson Imaging 2013;38:951-4.
- Stevenson RE. Common pathogenesis for sirenomelia, OEIS complex, limb-body wall defect, and other malformations of caudal structures. Am J Med Genet A 2021;185:1379-87.
- Gamzu R, Zalel Y, Jacobson JM, Screiber L, Achiron R. Type II single umbilical artery (persistent vitelline artery) in an otherwise normal fetus. Prenat Diagn 2002;22:1040-3.
- Murphy-Kaulbeck L, Dodds L, Joseph KS, Van den Hof M. Single umbilical artery risk factors and pregnancy outcomes. Obstet Gynecol 2010;116:843-50.


