
Imaging diagnosis and treatment of retrocaval ureter in children: clinical analysis of five cases
Introduction
The formation of the inferior vena cava is a complex process that begins in the sixth week, involving the development and selective regression of multiple venous systems (1). Initially, blood is drained by the anterior and posterior cardinal veins. Subsequently, the lower vena cava develops, taking over blood return from the lower body, and ultimately forms through multiple anastomoses and regressions (2). Retrocaval ureter is a rare congenital anomaly of the urinary system, commonly involving the right ureter passing behind the inferior vena cava, which leads to compressive urinary obstruction and consequent hydronephrosis (3). The incidence of this condition is approximately 0.13%, with a male-to-female ratio ranging from 3:1 to 4:1 (4). The formation of retrocaval ureter is closely related to abnormal vascular development during the embryonic period. Normally, the inferior vena cava develops from the anterior and posterior cardinal veins, with the ureter descending anteriorly to the psoas muscle and laterally to the inferior vena cava as it enters the bladder. However, if the posterior cardinal vein fails to regress and instead contributes to the formation of the inferior vena cava, the ureter passes behind the vena cava, wraps around it, and then descends anteriorly to enter the bladder, resulting in ureteral compression and urinary obstruction (5).
Clinically, the primary symptoms of retrocaval ureter include varying degrees of right flank pain, hematuria, recurrent urinary tract infections (UTIs), and hydronephrosis (6). In some mild cases, patients may remain asymptomatic and are only diagnosed in their third or fourth decade of life when hydronephrosis or significant renal dysfunction is present (7). Due to the often-subtle symptoms, this condition is frequently discovered incidentally during imaging studies. With advancements in medical imaging techniques, particularly three-dimensional computed tomography (CT) reconstruction and magnetic resonance urography (MRU), the diagnosis of retrocaval ureter has become more precise and clearer. The characteristic “fishhook sign” (reverse “C” or “J” shape) in imaging helps clinicians accurately identify this condition.
This article reviews the clinical data of five pediatric patients with retrocaval ureter treated at Anhui Provincial Children’s Hospital. The study summarizes the typical features and imaging manifestations of the condition and discusses the importance of early diagnosis and individualized treatment to provide reference for clinical practice.
Case presentation
This is a retrospective, single-center study aimed at analyzing the imaging manifestations of retrocaval ureter and the effectiveness of laparoscopic surgery. The subjects were five pediatric patients who underwent laparoscopic right-sided ureteral resection and reconstruction for retrocaval ureter at Anhui Provincial Children’s Hospital between January 2015 and September 2021. All procedures performed in this study were in accordance with the ethical standards of Anhui Provincial Children’s Hospital Ethics Committee (No. EYLL-2022-006) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients’ parents or legal guardians for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
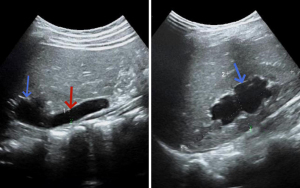
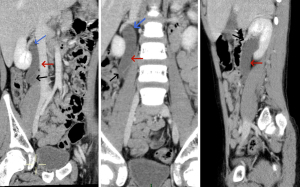
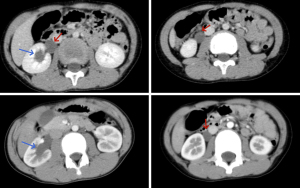
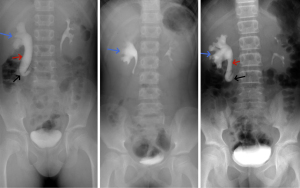
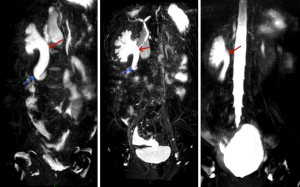
The ages of the patients ranged from 6 to 14 years, with a mean age of 10 years. Clinical symptoms included abdominal or flank pain, hematuria, and febrile UTIs, with all patients exhibiting varying degrees of hydronephrosis and upper ureteral dilation. Upon admission, all patients underwent ultrasound of the urinary system (Figure 1), CT scan (Figures 2,3), intravenous pyelogram (IVP) (Figure 4), or MRU (Figure 5). All patients received laparoscopic right-sided ureteral resection and reconstruction.
The patient underwent laparoscopic ureteral reconstruction under general anesthesia, using an extraperitoneal approach. The compressed or obstructed segment of the ureter was resected, and a ureterostomy was performed. The right renal pelvis was exposed by mobilizing the ascending colon, and the right ureter was identified using an ultrasonic scalpel, with the proximal ureter being transected. The reconstructed ureter was positioned anterior to the inferior vena cava and sutured to the anterior wall with 5-0 absorbable sutures. A double J stent was then placed, and the posterior wall of the ureter was sutured.
All five patients underwent successful surgery, with operative times ranging from 130 to 243 minutes, with an average of 180.2 minutes. The average intraoperative blood loss was 3.6 mL. During the follow-up period of 6 months to 2 years, patients’ symptoms of flank pain and hematuria disappeared, and no UTIs recurred. Follow-up abdominal ultrasounds showed that hydronephrosis was alleviated compared to preoperative findings.
Discussion
Clinically, retrocaval ureter is classified into two types based on the location of the ureter’s crossover with the inferior vena cava: Type I (low loop) is more common, with obstruction at the L3–4 level, and marked upper ureteral dilation in a reverse “J” or “S” shape; Type II (high loop) is rarer, with the obstruction at the L1–2 level, with less dilation and minimal hydronephrosis (8). The diagnosis and treatment of retrocaval ureter present challenges due to its low incidence, hidden clinical manifestations, and reliance on imaging diagnostic techniques (7). All five patients in this study presented with varying degrees of right-sided hydronephrosis, and the use of IVP, CT three-dimensional reconstruction, and MRU played crucial roles in the diagnosis. These cases provide valuable clinical experience for further exploration of diagnostic and treatment strategies for retrocaval ureter.
Imaging is central to diagnosing retrocaval ureter. Abdominal ultrasound is the most commonly used screening tool for assessing the structure and function of the kidneys and ureters (9). Ultrasound can detect hydronephrosis or ureteral dilation, which are common findings in retrocaval ureter (10). Although ultrasound is limited in detailing the ureter’s course around the inferior vena cava, it serves as a preliminary screening tool for further imaging. Historically, the diagnosis of retrocaval ureter primarily relied on IVP and retrograde pyelography (RP) (11). When renal function is normal, IVP or RP can clearly show the dilated renal pelvis, calyces, and upper ureter, with the ureter often curving towards the midline, taking on a reverse. In cases of severe obstruction, hydronephrosis increases the pressure, making it difficult for contrast agents to pass through, leading to poor or absent ureteral imaging. CT scanning, particularly with three-dimensional reconstruction, is an essential tool for diagnosing retrocaval ureter (12). CT scans provide detailed anatomical information, showing the ureter wrapping partially around the inferior vena cava and the compressed segment of the ureter, while ruling out retroperitoneal tumors that may displace the ureter (13). The high-resolution images of CT scans make them invaluable in preoperative planning and surgical evaluation. MRU is a non-invasive, high-resolution imaging technique that provides detailed three-dimensional images of the ureter and inferior vena cava. Without the need for contrast agents, MRU can display the complete morphology of the kidney and ureter, the degree of renal damage, and hydronephrosis, making it an excellent non-invasive diagnostic tool for patients allergic to contrast agents or with impaired renal function (14).
In the past, retrocaval ureter was typically treated with open surgery, but this approach is associated with significant trauma, slow recovery, and more postoperative complications. With the advancement of minimally invasive techniques, laparoscopic surgery has become increasingly common in urology and is now the preferred treatment for retrocaval ureter (15). Compared with traditional open surgery, laparoscopic surgery offers several distinct advantages: (I) minimally invasive: laparoscopic surgery via small incisions reduces pain and hospital stay, especially for kids, minimizing risks of complications and infections. (II) Faster recovery: all patients resumed normal activities post-surgery without major complications, proving safety and effectiveness. (III) Minimal blood loss: precision of laparoscopic surgery minimizes blood loss. All patients lost less than 10 mL, showcasing its superiority in controlling bleeding. Moreover, the duration of surgery is largely dependent on the complexity of separating the ureter from the inferior vena cava, rather than patient age or body size. In this study, operative times ranged from 130 to 243 minutes, reflecting the varying complexity of each case, but all surgeries were successfully completed, with good postoperative recovery. Although laparoscopic surgery has shown significant efficacy in treating retrocaval ureter, postoperative complications still need to be considered. The most common complications include ureteral stricture, recurrent hydronephrosis, and urinary leakage. To prevent complications, care must be taken during surgery to ensure precise ureteral reconstruction, avoid injury, and ensure that the anastomosis is in front of the inferior vena cava. Postoperative ureteral stenting is essential to ensure urine drainage and anastomotic healing. In this study, all patients received ureteral stents, and follow-up results showed no significant complications, with marked improvement in hydronephrosis.
The goal of treating retrocaval ureter is to relieve ureteral obstruction, restore normal urine flow, and prevent further renal damage (16). In this study, postoperative follow-up showed that all five patients had varying degrees of improvement in hydronephrosis, with no recurrence of UTIs. Although the short-term outcomes are promising, long-term prognosis of retrocaval ureter requires further follow-up. Additionally, studying the mechanisms of ureteral malformation and factors that may influence the success of ureteral reconstruction during surgery could help optimize treatment strategies.
Conclusions
Retrocaval ureter is a rare congenital anomaly of the urinary system, with imaging, particularly CT three-dimensional reconstruction and MRU, playing an essential role in its diagnosis. Laparoscopic ureteral resection and reconstruction, as a minimally invasive treatment, has the advantages of small incisions, quick recovery, and few complications. In this study, all five patients achieved good short-term outcomes after surgery, with long-term follow-up showing significant improvement in hydronephrosis. However, long-term follow-up is crucial for evaluating renal function recovery and preventing potential complications. Future research should continue to focus on the pathogenesis of retrocaval ureter and optimization of treatment strategies to improve long-term surgical success rates.
Acknowledgments
None.
Footnote
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-2081/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of Anhui Provincial Children’s Hospital Ethics Committee (No. EYLL-2022-006) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients’ parents or legal guardians for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lesma A, Bocciardi A, Rigatti P. Circumcaval Ureter: Embryology. Eur Urol Suppl 2006;5:444-8. [Crossref]
- Mao C, Cao Y, Zhang T. Laparoscopic Ureteral Reconstruction in Children with Retrocaval Ureter: A Modern Single Center Retrospective Study. J Endourol 2024;38:991-6. [Crossref] [PubMed]
- Peycelon M, Rembeyo G, Tanase A, Muller CO, Blanc T, Alhazmi H, Paye-Jaouen A, El Ghoneimi A. Laparoscopic retroperitoneal approach for retrocaval ureter in children. World J Urol 2020;38:2055-62. [Crossref] [PubMed]
- Hostiuc S, Rusu MC, Negoi I, Grigoriu M, Hostiuc M. Retrocaval ureter: a meta-analysis of prevalence. Surg Radiol Anat 2019;41:1377-82. [Crossref] [PubMed]
- Bass JE, Redwine MD, Kramer LA, Huynh PT, Harris JH Jr. Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics 2000;20:639-52. [Crossref] [PubMed]
- Ahmed M, Alhassan A, Sadiq MA, Lawal AT, Bello A, Maitama HY. Variable presentation of retrocaval ureter: Report of four cases and review of literature. Niger Postgrad Med J 2017;24:126-9. [Crossref] [PubMed]
- Yağız B, Yağmur İ, Hancıoğlu S, Demirel BD, Karagözlü Akgül A, Kaynak Şahap S. I Thought I Saw a Retrocaval Ureter; Don't Bite the Fish-Hook Sign So Easily. J Laparoendosc Adv Surg Tech A 2024;34:656-63. [Crossref] [PubMed]
- Escolino M, Masieri L, Valla JS, Lopez PJ, Tokar B, Mushtaq I, Esposito C. Laparoscopic and robotic-assisted repair of retrocaval ureter in children: a multi-institutional comparative study with open repair. World J Urol 2019;37:1941-7. [Crossref] [PubMed]
- Wang M, Zhang J, Zhang B, Ma Q. Value of detected hydronephrosis and hydroureter on ultrasound for detecting a ureteral stone: a retrospective study. Urolithiasis 2023;51:67. [Crossref] [PubMed]
- Hasdemir A, Atay M, Balkan E, İsleyen ME, Unal İ. A rare cause of hydronephrosis: Left retrocaval ureter without situs inversus or inferior vena cava duplication with CT and US imaging findings. J Clin Ultrasound 2024;52:1463-6. [Crossref] [PubMed]
- Liu E, Sun X, Guo H, Li F, Liu S, Wang K, Hou Y. Retroperitoneoscopic ureteroplasty for retrocaval ureter: report of nine cases and literature review. Scand J Urol 2016;50:319-22. [Crossref] [PubMed]
- Chen S, Xu B, Liu J, Ren Q, Hu X, Yang Y, Zhang X, Chen M. Retroperitoneal laparoscopic reconstruction for retrocaval ureter: experience and literature review. J Endourol 2012;26:1147-52. [Crossref] [PubMed]
- Wang X, Zhang Y, Li Z, Li X, Chen S, Han G, Xia M, Yang K, Zhou L, Zhang K, Li X. Robot-assisted laparoscopic ureteroplasty for retrocaval ureter with three-dimensional images navigation: technique and outcomes. BJU Int 2024;133:622-7. [Crossref] [PubMed]
- Acharya SK, Jindal B, Yadav DK, Singha S, Bagga D. Retrocaval ureter: a rare cause of hydronephrosis in children. J Pediatr Surg 2009;44:846-8. [Crossref] [PubMed]
- Seo IY, Oh TH, Jeon SH. Transperitoneal laparoscopic ureteroureterostomy with excision of the compressed ureter for retrocaval ureter and review of literature. Investig Clin Urol 2019;60:108-13. [Crossref] [PubMed]
- Mao L, Xu K, Ding M, Pan J, Guo Z. Comparison of the efficacy and safety of retroperitoneal laparoscopic and open surgery for the correction of retrocaval ureter. Ther Clin Risk Manag 2017;13:697-701. [Crossref] [PubMed]


