
Standing versus supine pelvic incidence in adult lumbar spondylolisthesis
Introduction
First described by Duval-Beaupère, pelvic incidence (PI) is a morphological spinopelvic parameter and is an angle that defines the position of the sacrum within the sagittal plane of the pelvis. It refers to the straight line between the midpoint of the S1 endplate and the midpoint of the center of the bilateral femoral head, as well as the angle between the vertical line of the S1 endplate. It is considered a constant value after maturity that is specific to each individual and does not change with position change (1). However, PI affects the individual’s overall spinal curvature, including lumbar lordosis (LL) and thoracic kyphosis (TK), and the ability to correct misalignment by pelvic retroversion. Therefore, the preoperative planning parameters for spinal deformity and lumbar degeneration surgery are commonly used to restore the ideal LL (2).
However, a fixed PI was questioned by Jean in 2014, who demonstrated a strong association between PI and age in individuals over 60 years (3). The findings of Jean were corroborated by Lee et al., Leven et al., and Godlewski et al. (4-6). In contrast, in a cadaveric study of 880 cases by Weinberg et al., age and height did not affect PI (7).
A randomized prospective study by Place et al. found that PI in 80% of participants changed according to the location of the pelvis (8). There is a growing body of evidence linking the movement of PI and sacroiliac (SI) joints (8-11). However, reports on whether PI changes with posture in patients with spondylolisthesis have not been conducted.
Therefore, the purpose of this study was to determine whether the spinopelvic sagittal alignment differs between the standing and supine position and whether PI varies with position to accurately assess sagittal alignment and aid in surgical planning. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-24-1954/rc).
Methods
Study population
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the ethics board of the Sichuan Provincial Orthopedic Hospital (No. KY2024-045-01). The requirement for individual consent was waived due to the retrospective nature of the analysis. A cross-sectional retrospective study was performed on patients with adult lumbar spondylolisthesis diagnosed and treated in Sichuan Province Orthopedic Hospital between January 2023 and January 2024 and who had complete imaging data. The inclusion criteria were a clear diagnosis of lumbar spondylolisthesis; an age of at least 18 years; and lumbar standing X-ray, supine X-ray, or scout computed tomography (CT) images that included the femoral head. Meanwhile, the exclusion criteria were an age younger than 18 years; previous pelvic, sacral, or lumbar internal fixation, lumbar fracture or malignancy; infection; previous hip replacement; and inadequate radiographic quality.
Data collection
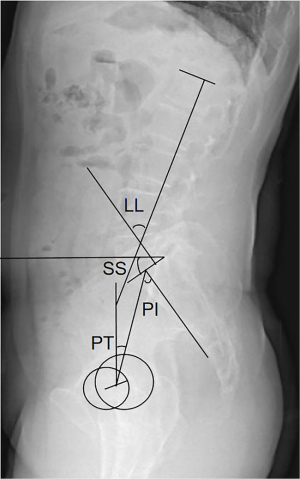
The demographic variables analyzed included patient age, sex, and body mass index (BMI). The above imaging data were measured by two attending physicians who had been engaged in spinal clinical work for more than 5 years and who were not aware of the study data but knew the measurement methods. The final value was considered to be the mean of the two measurements. The indices examined included PI, pelvic tilt (PT), sacral slope (SS), and LL (Figure 1).
Radiographic evaluation
Standing full-length lateral radiographs and supine lateral radiographs (or scout CT image) of the spine were acquired with clear anatomical markers in all cases. The protocol for X-ray image acquisition was that described by Horton et al. (12): under the guidance of professional technicians, the patient stood naturally, looked straight ahead, stood with both feet shoulder-width apart, straightened the knee joint, naturally flexed both elbow joints, bent both wrists, and clenched hands and placed them naturally in the supraclavicular fossa. CT of the lumbar spine was performed in the supine position, with the hip and knee extended. The imaging parameters were measured with the Picture Archiving and Communication System (PACS) of Sichuan Province Orthopedic Hospital.
Parameter measurement: pelvic parameters were measured according to the method described by Legaye et al. (1). PI was measured as the angle between the straight line connecting the midpoint of the S1 upper endplate and the midpoint of the line connecting the center of the bilateral femoral head and the vertical line of the S1 upper endplate. SS was measured as the angle between the upper endplate of S1 and the horizontal line. PT was formed by the vertical line of the connection between the midpoint of the central line of the bilateral femoral head and the midpoint of the end plate on S1. The angle was considered positive when the midpoint of the upper endplate was located behind the axis of the femoral head, and it was considered negative when the midpoint of the upper endplate was located in the front of S1. LL included the angle between the tangent line of the upper endplate of L1 and S1. Lordosis and kyphosis were considered to be positive and the negative, respectively (13,14).
Statistical analysis
This study strictly followed the Quality Appraisal of Diagnostic Reliability (QAREL) checklist to evaluate the data reliability (15). All results were statistically analyzed with SPSS 26.0 statistical software (IBM Corp., Armonk, NY, USA). Descriptive statistical calculations were performed for all demographic variables and measurements. All measured values are expressed as the mean ± standard deviation. The data measured by the two researchers were divided into two groups. The two groups of data were tested via the intraclass correlation coefficient (ICC) with absolute consistency. The ICC values of 0.8 to 1.0 indicated that the data were reliable. The imaging parameters were examined with the paired t-test. All P values were bilateral, and P<0.05 was considered to be statistically significant. All measurement data were tested with post hoc power analysis and the Cohen d value (small effect, >0.2 but <0.5; medium effect, >0.5 but <0.8; and large effect, ≥0.8).
Results
A total of 161 patients eligible for lumbar spondylolisthesis were included in this study, of whom 110 were ultimately enrolled according to the inclusion and exclusion criteria. Among the initial patients, 37 were excluded due to prior pelvic or lumbar fracture history, 3 due to prior lumbar or femoral head internal fixation, and 11 due to poor imaging quality (bilateral femoral head invisible or S1 endplate invisible) (Figure 2). There were 75 females and 35 males, the mean age was 64.22±9.98 years (range, 24–85 years), and the BMI was 24.18±2.99 kg/m2. There were 6 cases of L3 slip, 74 cases of L4 slip, 30 cases of L5 slip, 73 cases of degenerative lumbar spondylolisthesis, and 37 cases of isthmic spondylolisthesis. Between the three standing PI groups, designated as low PI (<45°), normal PI (45°–60°), and high PI (>60°), there was no significant correlation between PI and gender, slip segment, or slip type (all P values >0.05) (Table 1).
Table 1
| PI value size | Gender | Slipped segment | Slip type | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=35) | Female (n=75) | L3 (n=6) | L4 (n=74) | L5 (n=30) | Degenerative (n=73) | Isthmic (n=37) | |||
| Low PI (n=11) | 6 (5.5) | 5 (4.5) | 1 (0.9) | 9 (8.2) | 1 (0.9) | 8 (7.3) | 3 (2.7) | ||
| Normal PI (n=54) | 14 (12.7) | 40 (36.4) | 4 (3.6) | 34 (30.9) | 16 (14.5) | 36 (32.7) | 18 (16.4) | ||
| High PI (n=45) | 15 (13.6) | 30 (27.3) | 1 (0.9) | 31 (28.2) | 13 (11.8) | 29 (26.4) | 16 (14.5) | ||
| χ2 | 3.531 | 3.505 | 0.276 | ||||||
| P | 0.171 | 0.477 | 0.871 | ||||||
Data are presented as n (%). Chi-squared test, P<0.05. Low PI, <45°; normal PI 45°–60°; high PI, >60°. PI, pelvic incidence.
The data measured by the two researchers were divided into two groups. ICCs values of the two groups of data for the standing position were as follows: PI, 0.942; PT, 0.981; SS, 0.942; and LL, 0.915 (all P values <0.001). For the supine position, the ICCs values were as follows: PI, 0.932; PT, 0.952; SS, 0.937; and LL, 0.943 (all P values <0.001). All ICC values were >0.9, indicating that the two sets of measurement results had excellent reliability (Table 2).
Table 2
| Measurement | Standing | Supine |
|---|---|---|
| PI | 0.942 | 0.932 |
| PT | 0.981 | 0.952 |
| SS | 0.942 | 0.937 |
| LL | 0.915 | 0.943 |
All P values <0.001. ICC, intraclass correlation coefficient; LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope.
Further analysis showed that the supine PI was significantly lower than the standing PI (58.22°±12.369° vs. 55.67°±11.694°; P<0.001), and the mean absolute value was 4.11°±3.370°. The supine PT was significantly lower than the standing PT (20.64°±9.079° vs. 14.03°±7.489°; P<0.001). The mean absolute value was 7.06°±4.940°. The supine SS was significantly higher than the standing SS (37.61°±10.157° vs. 41.65°±9.168°; P<0.001), the mean absolute value was 6.22°±4.640°, and the average difference value was –4.04°±6.640°. There was no significant difference between supine LL and standing LL (50.20°±12.791° vs. 50.44°±11.658°; P=0.734).
The parameters of the standing position and supine position both met normal distribution and homogeneity of variance, and there were significant differences in the PI, PT, and SS between the standing position and supine position (P<0.05). When the position was changed from standing position to supine position, PI and PT decreased significantly, while SS increased significantly (Table 3). The above changes were also present for different slipped sections and slip nature (Tables 4,5).
Table 3
| Measurement | PI (°) | PT (°) | SS (°) | LL (°) |
|---|---|---|---|---|
| Standing | 58.22±12.369 | 20.64±9.079 | 37.61±10.157 | 50.20±12.791 |
| Supine | 55.67±11.694 | 14.03±7.489 | 41.65±9.168 | 50.44±11.658 |
| t value | 7.718 | 12.516 | −6.381 | −0.340 |
| P value | <0.001 | <0.001 | <0.001 | 0.734 |
| Cohen d value | 0.212 | 0.794 | 0.418 | 0.020 |
Paired t-test, P<0.05. The Cohen d value is the result of post hoc power analysis: 0.2≤ small effect <0.5, 0.5≤ medium effect <0.8, large effect ≥0.8. LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope.
Table 4
| Measurement | Degenerative (n=73) | Isthmic (n=37) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PI (°) | PT (°) | SS (°) | LL (°) | PI (°) | PT (°) | SS (°) | LL (°) | ||
| Standing | 57.19±11.052 | 21.38±9.091 | 35.82±9.217 | 47.85±12.432 | 60.26±14.577 | 19.17±8.998 | 41.14±11.095 | 54.84±12.367 | |
| Supine | 54.41±10.365 | 14.27±7.210 | 40.15±8.449 | 48.97±11.061 | 58.17±13.768 | 13.56±8.093 | 44.61±9.907 | 53.33±12.402 | |
| t value | 5.257 | 10.048 | −5.208 | −1.244 | 2.544 | 8.011 | −3.723 | 1.399 | |
| P value | <0.001 | <0.001 | <0.001 | 0.217 | 0.015 | <0.001 | 0.001 | 0.170 | |
Paired t-test, P<0.05. LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope.
Table 5
| Measurement | L4 (n=74) | L5 (n=30) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PI (°) | PT (°) | SS (°) | LL (°) | PI (°) | PT (°) | SS (°) | LL (°) | ||
| Standing | 57.55±11.439 | 21.60±8.855 | 35.96±8.551 | 48.95±12.242 | 60.91±14.979 | 19.17±9.382 | 41.80±13.137 | 53.53±14.642 | |
| Supine | 55.12±11.206 | 14.42±7.622 | 40.69±8.524 | 50.18±11.263 | 58.14±13.379 | 13.21±7.530 | 44.94±10.656 | 52.53±13.120 | |
| t value | 4.343 | 11.058 | −6.024 | −1.398 | 3.210 | 5.933 | −2.710 | 0.782 | |
| P value | <0.001 | <0.001 | <0.001 | 0.166 | 0.003 | <0.001 | 0.011 | 0.440 | |
Paired t-test, P<0.05. LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope.
The change in PI between standing and supine positions was significant (Table 6). Among the patients, 28 (25.5%) had an increase of 6° or more, 32 (29.1%) an increase of 3° or more, and 50 (45.5%) an increase within ±3°.
Table 6
| ΔPI | Gender | Slipped segment | Slip type | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=35) | Female (n=75) | L3 (n=6) | L4 (n=74) | L5 (n=30) | Degenerative (n=73) | Isthmic (n=37) | |||
| ΔPI <3° (n=50) | 19 (17.3) | 31 (28.2) | 3 (2.7) | 34 (30.9) | 13 (11.8) | 29 (26.4) | 21 (19.1) | ||
| 6°> ΔPI ≥3° (n=32) | 8 (7.3) | 24 (21.8) | 2 (1.8) | 21 (19.1) | 9 (8.2) | 25 (22.7) | 7 (6.4) | ||
| ΔPI ≥6° (n=28) | 8 (7.3) | 20 (18.2) | 1 (0.9) | 19 (17.3) | 8 (7.3) | 19 (17.3) | 9 (8.2) | ||
| χ2 | 1.703 | 0.320 | 3.578 | ||||||
| P | 0.427 | 0.988 | 0.167 | ||||||
Data are presented as n (%). Chi-squared test, P<0.05. ΔPI, the absolute value of the result of subtracting the Standing PI from the Supine PI; LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope.
The mean absolute ΔPI between the standing and supine positions in this cohort was 4.11°±3.370°. Sixty patients (54.5%) had absolute ΔPI >3°, and 28 (25.5%) had changes of >6°. There was no significant correlation between ΔPI and gender, slipped segment, or slip type (P>0.05).
Discussion
In the research on spinopelvic sagittal alignment, PI has been consistently considered to be a fixed measurement value of anatomical parameters that do not change after bone maturity. Consequently, it has often been used as a fixed reference value for patients with spinal degenerative diseases, especially degenerative scoliosis, to evaluate the optimal alignment of the spinopelvic sagittal plane and thus achieve a satisfactory postoperative result. Achieving the appropriate ratio of LL is closely related to the patient’s PI (16,17), but this assumes that the PI is fixed. However, in recent years, some studies have questioned the fixed invariance of PI. A randomized prospective study by Place et al. found that 80% of participants could experience a change in PI when they changed the position of their pelvis (8). Moreover, in the cadaver study by Bao et al., SI movement caused changes in PI (18).
In this study, we found that in patients with lumbar spondylolisthesis, standing PI was significantly higher than supine PI (55.67°±11.694° vs. 58.22°±12.369°; P<0.001), with a mean absolute difference of 4.11°±3.370°. Among the included patients, 60 (54.5%) experienced ΔPI >3° while 28 (25.5%) had changes >6°, which is consistent with the literature (6). The mean age of the cohort was 64.22±9.98 years, which is consistent with that of Jean’s study (3). The possible reasons for standing PI were significantly higher than supine PI in patients with lumbar spondylolisthesis are as follows: First, it may be related to the activity of the SI joint. PI is the angle between the midpoint of the S1 endplate and the midpoint of the line connecting the center of the femoral head on both sides, as well as the angle between the vertical line of the S1endplate, which is an angle that defines the position of the sacrum in the sagittal plane of the pelvis. Theoretically, it has no correlation with the anteroposterior tilt of the pelvis, but the reference point for measurement involves the superior endplate of the sacrum and the center of the bilateral femoral head; the joint that can move between the two is typically the SI joint, thus affecting the PI value. It was previously believed that PI becomes fixed after bone development and maturity, as the extremely small range of motion of the SI joint was thought incapable of affecting PI. A normal SI joint has a range of motion of about 1°–3° (19,20), and a change in PI of 3° represents a 100% increase in the range of motion of the SI joint. However, with the increase in age, the degeneration or vacuum sign of the SI joint represents potential joint instability, and the stress of the SI joint under different positions changes, as does the activity of the SI joint (21); this eventually leads to significant differences in PI values under different positions. In the standing position, the SI joint is tightened due to the weight bearing, while in the recumbent position, the joint is relatively relaxed. The center of the acetabulum is slightly backward from the superior endplate of the sacrum, resulting in a decrease in the PI in the supine position compared with that in the standing position. Second, supine CT images may not be as standardized as formal supine CT images, and the X-ray emission bulb reference point and angle of the fluoroscope may small deviate slightly in different positions, resulting in a shift in the center of the endplate of the superior sacrum or the center of the femoral head. Third, although the ICCs of the PI indicated good agreement, measurement errors could have influenced the results.
We additionally found that the supine PT was significantly lower than the standing PT (20.64°±9.079° vs. 14.03°±7.489°; P<0.001), with a mean absolute difference of 7.06°±4.940°. Moreover, the supine SS was significantly higher than the standing SS (37.61°±10.157° vs. 41.65°±9.168°; P<0.001), with the mean absolute difference being 6.22°±4.640°. As PI = PT + SS (22), PT is inversely correlated with changes in SS. In order to maintain sagittal balance of the spine and pelvis when the human body is standing, the pelvis rotates to compensate, and then SS decreases and PT increases. Pelvic compensation is absent in the supine position, and supine PT is smaller than standing PT, while SS is larger.
The changes in PI, PT, and SS in different body positions were not significantly correlated with gender, slipped segment, or slip type (P>0.05). There was no significant correlation of the changes in PI in different body positions with the slipped segment or the cause of slippage. In this study cohort, the most common condition was L4 and L5 lumbar spondylolisthesis, with L3 lumbar spondylolisthesis present only 6 cases (5.4%). Therefore, it can be preliminarily concluded that the changes in PI under different body positions have no obvious correlation with the sequence of the slip segment of the lower lumbar spine. Standing PI was higher than supine PI. However, whether the difference in PI under different body positions is related to lumbar spondylolisthesis could not be concluded because cases without lumbar spondylolisthesis were not included for comparison. However, it has been reported in the literature that the PI value of patients with degenerative scoliosis is higher in the standing position than in the supine position (6). Two types of spondylolisthesis were included in the study cohort, isthmic spondylolisthesis and degenerative spondylolisthesis, and there was no significant correlation between them in terms of ΔPI. Meanwhile, the mean PI value in the spondylolisthesis group for the standing position and supine position was larger than in the degenerative spondylolisthesis group. However, the change in PI value in different postural positions was significantly correlated with the type of slippage.
This study involved several limitations that should be addressed. First, we employed a retrospective design. Moreover, when post hoc power analysis was conducted, the Cohen d value of PI was 0.212, which was a small effect interval, indicating insufficient sample size. We can only conclude that patients with lumbar spondylolisthesis are associated with the position change for PI, but the pathophysiological mechanism is unclear. Second, although the cases in this study were all from the same hospital, the retrospective design made it difficult to ensure that the same techniques were used to obtain X-rays. The majority of supine radiographs were from scout CT images, which may not be as standardized an imaging technique as more formal supine radiographs. Moreover, despite the ICC for PI being excellent, measurement error was unavoidable and could have influenced the results. Third, we acknowledge that imaging changes in PI do not determine clinical significance, and prospective studies should be considered. The position and angle of the X-ray bulb were fixed, and the participants’ perspective position markers were fixed to reduce errors caused by the transmission angle. Therefore, the sample size should be increased to reduce the differences caused by perspective changes, and further clarify the correlation between PI changes and body position.
Conclusions
Through an analysis of radiologic spinopelvic sagittal alignment parameters of adult patients with lumbar spondylolisthesis, we found that there was a significant difference in spinopelvic sagittal alignment between the standing position and supine position. PI and PT were significantly higher in the standing position than in the supine position, SS was significantly lower, and LL showed no significant difference. The variability in PI in different postures suggests that PI is not a fixed anatomical parameter and may change between supine and standing positions. Our findings may serve as a reference for changes in spinopelvic sagittal alignment in patients with lumbar spondylolisthesis.
Acknowledgments
The authors would like to thank Qinglong Li and Min Cao for their contribution to the collection of primary data for the study, specifically, the demographic, clinical, and radiographic data, as well as preparing data for statistical analysis.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-24-1954/rc
Funding: This study was supported by
Conflicts of Interest: All authors completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-1954/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the ethics board of the Sichuan Provincial Orthopedic Hospital (No. KY2024-045-01). The requirement for individual consent was waived due to the retrospective nature of the analysis.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99-103. [Crossref] [PubMed]
- Hu Z, Qian Z, Li W, Li J, Tang Z, Ling C, Xu Y, Liu Z, Zhu Z, Qiu Y. Preoperative supine pelvic incidence predicts standing pelvic incidence following S2AI fixation in patients with adult spinal deformity: a prospective study. Eur Spine J 2024;33:1816-20. [Crossref] [PubMed]
- Jean L. Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J 2014;23:1394-9. Erratum in: Eur Spine J 2014;23:1583. [Crossref] [PubMed]
- Lee JH, Na KH, Kim JH, Jeong HY, Chang DG. Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J 2016;25:3707-14. [Crossref] [PubMed]
- Leven DM, Merrill RK, Kim JS, Meaike JJ, Suchman K, Kim JH, et al. Fundamental Differences and Changes in Pelvic Parameters Depending on Age, Gender and Race. The Spine J 2016;16:s277. [Crossref]
- Godlewski MW, Haselhuhn JJ, Polly DW Jr. Standing versus supine pelvic incidence in adult spinal deformity patients. Eur Spine J 2024;33:3851-6. [Crossref] [PubMed]
- Weinberg DS, Morris WZ, Gebhart JJ, Liu RW. Pelvic incidence: an anatomic investigation of 880 cadaveric specimens. Eur Spine J 2016;25:3589-95. [Crossref] [PubMed]
- Place HM, Hayes AM, Huebner SB, Hayden AM, Israel H, Brechbuhler JL. Pelvic incidence: a fixed value or can you change it? Spine J 2017;17:1565-9. [Crossref] [PubMed]
- Ishida W, Elder BD, Holmes C, Lo SL, Goodwin CR, Kosztowski TA, Bydon A, Gokaslan ZL, Wolinsky JP, Sciubba DM, Witham TF. Comparison Between S2-Alar-Iliac Screw Fixation and Iliac Screw Fixation in Adult Deformity Surgery: Reoperation Rates and Spinopelvic Parameters. Global Spine J 2017;7:672-80. [Crossref] [PubMed]
- Schroeder N, Noschenko A, Burger E, Patel V, Cain C, Ou-Yang D, Kleck C. Pelvic Incidence Changes Between Flexion and Extension. Spine Deform 2018;6:753-61. [Crossref] [PubMed]
- Mikula AL, Fogelson JL, Oushy S, Pinter ZW, Peters PA, Abode-Iyamah K, Sebastian AS, Freedman B, Currier BL, Polly DW, Elder BD. Change in pelvic incidence between the supine and standing positions in patients with bilateral sacroiliac joint vacuum signs. J Neurosurg Spine 2021;34:617-22. [Crossref] [PubMed]
- Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36" radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976) 2005;30:427-33. [Crossref] [PubMed]
- Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828-33. [Crossref] [PubMed]
- Li W, Sun Z, Chen Z. Imaging study of normal sagittal parameters of the spine-pelvis. Chinese Journal of Orthopedics 2013;33:447-53.
- Lucas N, Macaskill P, Irwig L, Moran R, Rickards L, Turner R, Bogduk N. The reliability of a quality appraisal tool for studies of diagnostic reliability (QAREL). BMC Med Res Methodol 2013;13:111. [Crossref] [PubMed]
- Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay AEuropean Spine Study Group (ESSG). Global Alignment and Proportion (GAP) Score: Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J Bone Joint Surg Am 2017;99:1661-72. [Crossref] [PubMed]
- Ma H, Hu Z, Shi B, Liu Z, Zhu Z, Chu WCW, Lam TP, Cheng JCY, Qiu Y. Global Alignment and Proportion (GAP) score in asymptomatic individuals: is it universal? Spine J 2022;22:1566-75. [Crossref] [PubMed]
- Bao H, Zhang Y, Shu S, Zhang T, Gu Q, Jing W, Liu Z, Sun X, Qiu Y, Zhu Z. Position-related Change of Pelvic Incidence Depends on the Nonfused Sacroiliac Joint in Patients with Degenerative Spinal Diseases. Spine (Phila Pa 1976) 2021;46:796-802. [Crossref] [PubMed]
- Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila Pa 1976) 2009;34:E162-9. [Crossref] [PubMed]
- Wilke HJ, Fischer K, Jeanneret B, Claes L, Magerl F. In vivo measurement of 3-dimensional movement of the iliosacral joint. Z Orthop Ihre Grenzgeb 1997;135:550-6. [Crossref] [PubMed]
- Sturesson B, Uden A, Vleeming A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine (Phila Pa 1976) 2000;25:364-8. [Crossref] [PubMed]
- Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J 2011;20:564-71. [Crossref] [PubMed]



