
Penetrating lipoma of the right atrial wall: a case description and literature analysis
Introduction
Primary cardiac neoplasms are exceedingly rare, with an estimated post-mortem incidence of 0.001% to 0.03% (1). Approximately three-quarters of these lesions are benign, with cardiac myxomas being the most common. Other benign tumors include those of adipose tissue, such as lipomatous hypertrophy and lipoma, which collectively account for 6–10% of cases. Cardiac lipomas are well-circumscribed, encapsulated benign masses predominantly composed of mature adipocytes (2). They are typically found in the left ventricle and right atrium but can occur in various locations within the heart, with 25%, 50%, and 25% being pericardial, subendocardial, and intramyocardial, respectively (3). These tumors can present at any age and have no gender predisposition. Most cardiac lipomas are incidental findings that remain asymptomatic but can lead to embolization, syncope, and blood flow obstruction within the cardiac chambers or coronary arteries due to their mass effect. Here, we describe a novel case of a right atrial wall–penetrating lipoma, an occurrence not previously reported.
Case presentation
Chief complaints
A 47-year-old male patient was hospitalized due to frequent chest pain over the previous month, which worsened over the previous 3 days.
Patient background
The patient had a history of myocardial infarction 13 years prior and underwent coronary angiography, which revealed a significant narrowing (70%) of the left anterior descending artery and unknown stenosis of the remaining coronary arteries. No interventional therapy was performed, and the patient was prescribed Plavix, Lipitor, Simvastatin, and Aspirin. In 2016, the patient experienced gastrointestinal bleeding due to inadequate monitoring of blood coagulation indicators while on anticoagulants, leading to the discontinuation of these medications. A previous echocardiogram showed no space-occupying lesions in the heart. The patient had a history of hyperlipidemia but no hypertension or diabetes.
Personal and family history
The patient had a 20-year smoking history and denied a history of alcohol consumption and a family history of cardiovascular diseases.
Physical examinations
The patient had a body temperature of 36.3 ℃, a pulse rate of 72 beats per minute, a respiration rate of 15 breaths per minute, a blood pressure of 131/84 mmHg, a body mass index of 26.94 kg/m2, and a weight of 82.5 kg. Physical examination revealed regular arrhythmia, an enlarged cardiac silhouette extending to the left and inferiorly, and no abnormal valve sounds or heart murmurs. Bilateral lung sounds were clear, and no lower extremity swelling was observed.
Laboratory examinations
The laboratory results were as follows: hemoglobin level, 136 g/L; cardiac troponin T (cTNT) level, 13 pg/mL; creatine kinase-MB (CK-MB) level, 1.04 ng/mL; and B-type natriuretic peptide (BNP) level, 232 pg/mL.
Imaging examinations
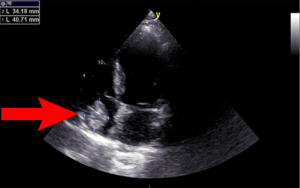
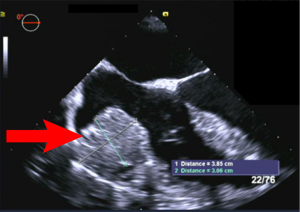
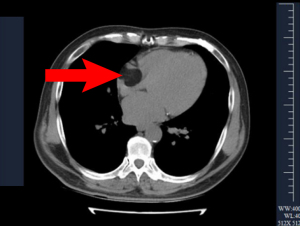
Electrocardiography showed a sinus rhythm with Q waves in leads II, III, augmented vector foot (aVF), and V3–V6, and ST-segment elevation in leads V1–V5. Moreover, it revealed a dilated left atrium (48 mm) and left ventricle (end-diastolic diameter, 67 mm) with severe diffuse hypokinesis and a 32.2-mm dyskinetic area in the apical left ventricle. A parenchymal echo of about 40.7 mm × 34.2 mm was observed in the right atrium (Figure 1). Transesophageal echocardiography revealed a large mass of about 38.5 mm × 30.6 mm in the right atrium (Figure 2). Coronary angiography showed significant stenosis of 50–60% at the end of the left main artery, 90% in the middle left anterior descending artery, 80–90% in the left circumflex artery opening, and 100% occlusion in the middle right coronary artery. A computed tomography (CT) scan revealed a nodule in the superior lobe of the right lung, left ventricular enlargement, and a fat density shadow in the right atrial nodal region with a CT value of –107 Hounsfield units (HU) (Figure 3).
Intraoperative and pathological findings
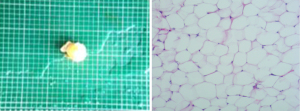
Intraoperative observation showed a lipoma attached to the lateral wall of the right atrium, penetrating the atrial wall (Figure 4). Pathological examination revealed atrial wall tissue with a size of 50 mm × 30 mm and a thickness of about 2 mm, with yellowish soft fat-like tissue on the cut surface. The gross specimens appeared as a complete capsule, confirming the encapsulated nature of the lipoma, although the tumor exhibited infiltrating properties into the atrial wall. Microscopically, the tumor was composed of uniform fat cells with some nuclear enlargement and cell proliferation. The immunohistochemical results were as follows: MDM2(–), CDK4(+), Ki-67(<5%), and S-100(+). These results confirmed the diagnosis of a lipoma with some proliferative activity (Figure 5).

Treatment and follow-up
The patient underwent coronary bypass surgery and lipomatectomy. One week postoperatively, no significant space-occupying lesions were detected in the heart on echocardiography, and the patient was in good condition with no adverse events.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Cardiac lipomas are rare benign tumors composed of encapsulated or nonencapsulated adipocytes that can develop in any region of the heart. Cardiac lipomas can be classified into three types based on their encapsulation and tissue characteristics: true encapsulated lipomas, which are well-defined and separated from the myocardium; lipomatous infiltration, in which the adipose tissue infiltrates the myocardium without clear encapsulation; and lipomatous hypertrophy of the interatrial septum (LHIS), characterized by nonencapsulated adipose tissue deposition in the interatrial septum (4). Unlike the more commonly reported cases, which are typically confined to specific cardiac chambers, the lipoma in our case uniquely penetrated the right atrial wall. Gross specimens demonstrated a complete capsule, yet the tumor exhibited infiltrating properties into the atrial wall. This distinct behavior suggests that the tumor cannot be easily categorized into the existing classifications. This finding has not been previously documented, making this case particularly noteworthy and highlighting the need for further research into the pathogenesis and classification of cardiac lipomas.
Literature review and comparison
A review of the literature suggests that cardiac lipomas are generally incidental findings and often asymptomatic. Over the past decade, we have found that the prevalence of cardiac lipomas is scarce, particularly cases involving penetration of the cardiac wall. Cardiac lipomas are typically benign tumors composed of adipocytes and can originate from the epicardium, myocardium, or endocardium. However, penetration of the cardiac wall by these tumors is exceptionally rare.
In our comprehensive review, we identified three cases of lipomas originating on the epicardial side and penetrating the basal ventricular myocardium, with one of these cases reported as multiple penetrating lipomas (5-7). Case 1 was a 15-year-old girl with multiple subepicardial lipomas infiltrating all four cardiac chambers, leading to sudden death. The extensive involvement, including lipomatous hypertrophy of the interatrial groove and multiorgan involvement, was unique. The sudden cardiac arrest was attributed to fatty infiltration causing ventricular fibrillation (5). Case 2 was a 31-year-old woman who experienced recurrent palpitations and ventricular tachycardias, which worsened during pregnancy. The cardiac tumor had infiltrated the right ventricle. The patient underwent successful tumor excision, including the restoration of the right ventricular wall and tricuspid valve, with no recurrence of symptoms during a 6-month follow-up (6). Case 3 was a 25-year-old male with palpitations and presyncope, in whom imaging revealed a large lipoma compressing the right ventricle and atrium. The mass was surgically excised, and histopathology confirmed a lipoma. The patient remained asymptomatic post-surgery with no further arrhythmic events (7). Four other cases were reported that involved tumors with intracavitary behavior: the first was a case of lipoma within the right ventricle involving the interatrial septum; the second case involved the tricuspid valve and septum; the third case included a biventricular tumor occupying the basal myocardium; and the fourth case was an atrial mass on the left side extending into the ventricles, involving the mitral valve (8-10). Additionally, one case report described a mass involving the superior vena cava (SVC) and the pulmonary vein on the right side (2). Li et al. reported multiple cardiac lipomas leading to sudden death, and Schrepfer et al. detailed a case of symptomatic right ventricular lipoma. However, neither of these cases involved wall penetration (5,6). Our case shares similarities with a case reported by Barbuto et al. (11), including the presence of an intracardiac mass and the use of imaging modalities for diagnosis. However, differences were noted in terms of clinical presentations, such as the absence of shortness of breath during exercise in our patient. Furthermore, the size and location of the mass differed from those reported by Barbuto et al (11). This highlights the variability in clinical manifestations and the importance of individualized diagnostic and treatment approaches. Our case, with a lipoma penetrating the right atrial wall, adds a new dimension to the understanding of cardiac lipomas. This unique presentation emphasizes the importance of recognizing the potential for cardiac lipomas to exhibit invasive behavior, which can significantly impact clinical management and outcomes.
The distinctiveness of our case is highlighted by the lipoma penetrating the right atrial wall, a phenomenon that has not been previously documented. This highlights the necessity for comprehensive diagnostic evaluations and the potential need for innovative surgical approaches. The findings from this case contribute to the broader understanding of cardiac lipomas and underscore the importance of continued research and vigilance in clinical practice to accurately diagnose and effectively manage such rare presentations (12).
Mechanistic insights
The exact pathogenesis of cardiac lipomas remains unclear (13). In our case, the tumor’s ability to infiltrate the atrial wall suggests a potential for local invasiveness that is atypical for benign lipomas. Immunohistochemical analysis revealed a low proliferation index (Ki-67 <5%) and positive CDK4 expression, indicating some degree of cellular activity which might contribute to its invasive behavior. Further molecular studies are warranted to elucidate the underlying mechanisms driving this atypical growth pattern.
Diagnostic challenges
Initial cardiac neoplasms are exceedingly rare, with a postmortem incidence estimated between 0.001% and 0.03% (1). Among these, three-quarters are benign, predominantly manifesting as cardiac myxomas. Other benign lesions, such as lipomatous hypertrophy and lipoma, constitute 6–10% of the total cases. Cardiac lipomas, typically encapsulated benign masses composed of mature adipocytes, are most frequently found in the left ventricle and right atrium, although they can occur in various regions of the heart, with 25% being pericardial, 50% subendocardial, and 25% intramyocardial (2,3,13). The pathogenesis of cardiac lipomas remains unclear, although they generally grow slowly and remain asymptomatic. Clinical symptoms, when present, depend on the size and location of the tumor. Large lipomas can cause severe blood flow obstruction, valve dysfunction, or compression of the heart and adjacent vessels.
In our case, the lipoma uniquely penetrated the right atrial wall, a presentation not previously documented. Despite its substantial size (approximately 30 mm in diameter), the tumor did not compress the superior or inferior vena cava or obstruct the tricuspid valve, resulting in the absence of systemic symptoms such as edema or syncope. Moreover, although invasive lipomas involving the cardiac conduction system can lead to arrhythmias, our patient did not experience such complications despite the tumor’s infiltration.
Diagnosing cardiac lipomas, particularly those with atypical presentations, poses significant challenges. Differential diagnosis is essential for evaluating cardiac masses, particularly in distinguishing between LHIS and cardiac lipomas. LHIS is characterized by the benign accumulation of adipose tissue within the interatrial septum and is often associated with obesity. One study indicated a significant correlation between increased visceral adiposity and the presence of LHIS (14). However, there was no clear evidence regarding whether the penetrating lipoma of the right atrial wall in this case is related to adiposity. Advances in imaging modalities, particularly in CT and magnetic resonance imaging (MRI) technologies, have enhanced our ability to detect and characterize these conditions, improving diagnostic accuracy and patient outcomes. Transthoracic echocardiography offers a simple and noninvasive method for detecting cardiac masses with high specificity and sensitivity. However, additional imaging techniques such as CT and cardiac MRI are often required to provide detailed information on the tumor’s size, location, and characteristics. Cardiac MRI is a crucial tool in the evaluation of cardiac tumors, including lipomas. It provides superior soft tissue contrast, allowing for detailed assessment of the tumor’s size, location, and relationship with surrounding structures. MRI can also characterize the tissue composition of the mass, distinguishing between fatty, fibrous, and other tissue types, which is critical for planning surgical interventions. Moreover, MRI can assess the functional impact of the tumor on cardiac chambers and valves. These attributes make cardiac MRI an invaluable modality for comprehensive preoperative planning and postoperative follow-up in patients with cardiac tumors (15). Although cardiac MRI can provide detailed tissue characterization and assess myocardial involvement, it was not performed due to resource limitations and the clinical urgency for intervention. The combined findings from echocardiography and CT were sufficient for surgical planning. Differential diagnoses include atrial septal lipomatous hypertrophy, a nonencapsulated adipocyte mass often mistaken for cardiac tumors (16). Left heart catheterization is essential for assessing coronary anatomy, particularly in patients requiring surgery, as it helps determine whether the tumor affects myocardial vascular supply (16). In this case, preoperative left heart catheterization confirmed that there was no vascular supply to the tumor. Furthermore, transesophageal echocardiography provided additional insights, enabling a more precise surgical plan and highlighting the importance of comprehensive imaging in managing cardiac lipomas effectively. Pulsed wave (PW) tissue Doppler imaging (TDI) was not used in this case; however, it can be particularly useful in the evaluation of intracardiac masses. PW-TDI allows for the assessment of the mobility and echogenic characteristics of cardiac structures, which can help differentiate between benign and potentially embolic masses. A study by Sonaglioni et al. demonstrated that PW-TDI could predict the embolic risk of left ventricular thrombi by assessing mass peak antegrade velocity (17). In cases where malignancy or high embolic potential is suspected, PW-TDI can provide valuable prognostic information. This case underscores the importance of comprehensive imaging and careful differential diagnosis in identifying atypical presentations of cardiac lipomas. The findings contribute to the broader understanding of cardiac lipomas and emphasize the need for vigilance in clinical practice. Future research should focus on elucidating the pathogenesis of these tumors and developing guidelines for their management, which could significantly enhance diagnostic accuracy and therapeutic outcomes in similar cases (12).
Treatment strategy
Research indicates that a small percentage of deaths related to cardiovascular issues may be attributed to sudden death resulting from initial lesions or tumors in the heart, particularly among individuals aged 0–34 year. Although these occurrences are rare, they nonetheless contribute to mortality rates within this demographic (18). Given the size and infiltration of lipoma in our case, surgical resection was deemed necessary to prevent potential complications such as obstruction and arrhythmias. The decision-making process involved comprehensive preoperative imaging and intraoperative findings, which confirmed the tumor’s extensive involvement. The successful resection of the tumor, along with part of the right atrial wall, underscores the importance of thorough surgical planning and execution.
Prognosis and follow-up
Postoperative follow-up is critical for monitoring recurrence and assessing the long-term outcomes of patients. In this case, the patient showed no signs of recurrence or adverse events during the follow-up period. This favorable outcome aligns with other reports suggesting that complete surgical resection of cardiac lipomas generally results in excellent long-term prognosis (12).
Future research directions
This case highlights the need for further research into the molecular and genetic factors contributing to the invasive behavior of certain cardiac lipomas. Additionally, advancements in imaging techniques could improve the early detection and characterization of these tumors. Prospective studies focusing on the long-term outcomes of patients with atypical cardiac lipomas could provide valuable insights into the optimal management strategies for these rare entities.
Conclusions
This report documents a rare case of a right atrial lipoma with wall penetration, expanding the clinical spectrum of cardiac lipomas. The successful surgical management and favorable prognosis underscore the importance of accurate diagnosis, careful surgical planning, and diligent postoperative follow-up. Further research is needed to fully understand the pathogenesis and optimal treatment of such atypical cardiac tumors.
Acknowledgments
We would like to thank the staff of the Department of Cardiac Function at People’s Hospital of Liaoning Province for providing valuable clinical and ultrasonic support.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-1128/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Reynen K. Cardiac myxomas. N Engl J Med 1995;333:1610-7. [Crossref] [PubMed]
- Shah OA, Badran A, Kaarne M, Velissaris T. Right atrial and SVC infiltrating mass-the entity of infiltrating lipoma. J Cardiothorac Surg 2019;14:210. [Crossref] [PubMed]
- da Silveira WL, Nery MW, Soares EC, Leite AF, Nazzetta H, Batista MA, de Oliveira CP, de Oliveira VG. Lipoma of the right atrium. Arq Bras Cardiol 2001;77:361-8. [Crossref] [PubMed]
- Li FP, Wang XF, Xiao J, Xiao YB. Myocardial lipomatous infiltration of the left ventricular wall. J Card Surg 2010;25:513-5. [Crossref] [PubMed]
- Li J, Ho SY, Becker AE, Jones H. Multiple cardiac lipomas and sudden death: a case report and literature review. Cardiovasc Pathol 1998;7:51-5. [Crossref] [PubMed]
- Schrepfer S, Deuse T, Detter C, Treede H, Koops A, Boehm DH, Willems S, Lacour-Gayet F, Reichenspurner H. Successful resection of a symptomatic right ventricular lipoma. Ann Thorac Surg 2003;76:1305-7. [Crossref] [PubMed]
- Shenthar J, Sharma R, Rai MK, Simha P. Infiltrating cardiac lipoma presenting as ventricular tachycardia in a young adult. Indian Heart J 2015;67:359-61. [Crossref] [PubMed]
- Fang L, He L, Chen Y, Xie M, Wang J. Infiltrating Lipoma of the Right Ventricle Involving the Interventricular Septum and Tricuspid Valve: Report of a Rare Case and Literature Review. Medicine (Baltimore) 2016;95:e2561. [Crossref] [PubMed]
- Vaughan CJ, Weremowicz S, Goldstein MM, Casey M, Hart M, Hahn RT, Devereux RB, Girardi L, Schoen FJ, Fletcher JA, Morton CC, Basson CT. A t(2;19)(p13;p13.2) in a giant invasive cardiac lipoma from a patient with multiple lipomatosis. Genes Chromosomes Cancer 2000;28:133-7. [Crossref] [PubMed]
- Anderson DR, Gray MR. Mitral incompetence associated with lipoma infiltrating the mitral valve. Br Heart J 1988;60:169-71. [Crossref] [PubMed]
- Barbuto L, Ponsiglione A, Del Vecchio W, Altiero M, Rossi G, De Rosa D, Pisani A, Imbriaco M. Humongous right atrial lipoma: a correlative CT and MR case report. Quant Imaging Med Surg 2015;5:774-7. [Crossref] [PubMed]
- Wang H, Hu J, Sun X, Wang P, Du Z. An asymptomatic right atrial intramyocardial lipoma: a management dilemma. World J Surg Oncol 2015;13:20. [Crossref] [PubMed]
- Sankar NM, Thiruchelvam T, Thirunavukkaarasu K, Pang K, Hanna WM. Symptomatic lipoma in the right atrial free wall. A case report. Tex Heart Inst J 1998;25:152-4.
- Mallio CA, Di Gennaro G, Greco F, Pescosolido A, Bernetti C, Piccolo CL, Buffa V, Quattrocchi CC, Beomonte Zobel B. Visceral adiposity in patients with lipomatous hypertrophy of the interatrial septum. Heart Vessels 2024;39:160-6. [Crossref] [PubMed]
- Li X, Chen Y, Liu J, Xu L, Li Y, Liu D, Sun Z, Wen Z. Cardiac magnetic resonance imaging of primary cardiac tumors. Quant Imaging Med Surg 2020;10:294-313. [Crossref] [PubMed]
- Wu S, Teng P, Zhou Y, Ni Y. A rare case report of giant epicardial lipoma compressing the right atrium with septal enhancement. J Cardiothorac Surg 2015;10:150. [Crossref] [PubMed]
- Sonaglioni A, Nicolosi GL, Lombardo M, Anzà C, Ambrosio G. Prognostic Relevance of Left Ventricular Thrombus Motility: Assessment by Pulsed Wave Tissue Doppler Imaging. Angiology 2021;72:355-63. [Crossref] [PubMed]
- De Filippo M, Corradi D, Nicolini F, Rastelli A, Ugo F, Araoz PA, Sverzellati N, Gherli T, Zompatori M. Hemangioma of the right atrium: imaging and pathology. Cardiovasc Pathol 2010;19:121-4. [Crossref] [PubMed]


