An evaluation of a superfast MRI sequence in the diagnosis of suspected acute appendicitis
Introduction
A lack of typical symptoms may delay appropriate therapy for in acute appendicitis, such as urgent surgical intervention, which contributes to a fatality rate ranging from 0.8-8% for these patients (1,2). The advent of imaging techniques was lauded as a mean of ending the uncertainty associated with this important diagnosis. Computed tomography (CT) has emerged as the dominant imaging modality for diagnosing suspected appendicitis because of higher sensitivity than ultrasound (US) (3-7). However CT fails in 12% of patients and results in considerable ionizing radiation exposure, especially in young individuals (8).
The magnetic resonance imaging (MRI) ultrafast sequences can shorten examination times and obtain improved images with fewer motion artifacts (1). If proven to be sufficiently accurate, MRI could be introduced in the diagnostic pathway of patients with suspected appendicitis, increasing diagnostic accuracy and improving clinical outcome, without the risk of radiation.
During the past decade, conventional MRI sequences (including T1W and T2W) have become widely available in abdominal imaging. However, to our knowledge this is the first study using ultrafast sequence of SENSE-BTFE with fat suppression. In this study, we hypothesized that ultrafast sequences of sensitivity encoding (SENSE) with balanced turbo field echo (BTFE) and spectral presaturation and inversion recovery (SPIR) could assist in the clinical diagnosis of acute appendicitis. We explored the specificity and sensitivity in the diagnosis by the sequence of SENSE-BTFE-SPIR. During the past decade, conventional MRI sequences (including T1W and T2W) have become widely available in abdominal imaging. However, to our knowledge this is the first study using the ultrafast sequence of SENSE-BTFE with fat suppression.
Materials and methods
Subjects
This study was approved by the ethics committee in our hospital and informed consents were obtained from the subjects. During a 2-year span from September 1, 2009 to September 31, 2011, 41 cases of suspected acute appendicitis were evaluated prospectively with an MRI examination and confirmed during subsequent surgery in our institution. These consecutive patients (23 female, 18 male; mean age, 41.5±11.3 years old) with clinically suspected appendicitis visited our institution and all underwent an abdominal US study (as is the policy in our hospital) for suspected appendicitis.
Clinical evaluation
The referring physicians had to fill in a form before requesting imaging, in which they scored the patient suspected of having appendicitis based on Alvarado scores system (9). Patient demographics, presenting signs and symptoms were documented.
MRI acquisition
All MR examinations were performed on a 1.5 T superconducting MR scanner (Achieva Nova Dual, Philips, Netherlands) with a radiant field strength of 30 mT/m, a gradient switching rate of 105 mT/ms, and a four-element phased array abdominal coil. At the time of examination, the patient was supine with the abdominal coil centered at the ileocecal level to ensure the quality of images. Oral or intravenous contrast material was not administered. Neither sedation nor anesthesia was used during the examination.
The MRI examination included breath-hold axial and coronal T2 weighted with Driven Equilibrium RF reset pulse (T2W-DRIVE) and SENSE-BTFE-SPIR. SPIR is a sequence with fat suppression to suppress the high fat signal surrounding the appendix. For visualization of appendix, slices were acquired from the inferior pole of the kidneys to the bottom of the pelvis in transverse plane. The parameters of SENSE-BTFE-SPIR and T2W-DRIVE sequence are shown in Table 1. The sensitivity encoding (SENSE) factor was set as 1.8. The three sequences took approximately 2 minutes and 42 seconds in total. Prior to the examination, the technician explained the MRI procedure to the patient and trained the patient in holding their breath for about 20 seconds, using a hyperventilation method with three deep breaths followed by a breath-hold during deep inspiration. All patients could perform three breath-holds in one sequence adequately, and no major breathing artifacts were seen. A multislice MRI technique was used for all patients with 4-mm-thick slices with acquisition times less than 60 s, so each slice of image didn’t interfere the others during each breathholding.
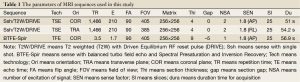
Full table
MRI interpretation
All MRI studies were reviewed by a gastrointestinal radiologist (B.Z.) with more than 10 years of experience, who was blinded to the clinical data. All acute appendicitis cases were confirmed on the basis of Nitta’s criteria (10): (I) diameter of the appendiceal cavity >6 mm; (II) appendiceal cavity effusion; (III) appendiceal wall thickening >2 mm; (IV) high signal changes in the effusion surrounding the appendiceal wall; (V) appendix surrounded by phlegmon or abscess formation; and (VI) appendix with extraluminal free air. The MRI criteria that excluded appendicitis were a normal appendix of 6 mm or less, or an appendix with a diameter of more than 6 mm without evidence of peri-appendiceal inflammatory changes.
Patient follow-up
All patients with high suspicion of having appendicitis were operated on within a few hours of the MRI studies. The pathological criteria for acute appendicitis were the presence of polymorphic granulocytes throughout the appendiceal wall, including the muscularis (11). Patients who did not undergo surgery were not included in this study.
Statistical analysis
True-positive cases were those with a positive imaging diagnosis at MRI for acute appendicitis and histopathological confirmation. True-negative results were those with negative imaging results for acute appendicitis, or with imaging results of an alternative diagnosis explaining the clinical condition, and did not develop appendicitis at follow-up. The sensitivity and specificity values for detecting acute appendicitis were calculated.
Results
Clinical results
Only 36 of these 41 patients had histopathologically proven appendicitis, and 5 of 41 had confirmed other diseases by surgery, including 1 with ileal diverticulum (irregular dilatation of the end of ileum seen by MRI), 2 with pelvic inflammation (hydrops in pelvic cavity seen by MRI), and 2 with acute gastroenteritis (inflammation in the end of ileum seen by MRI). Alvarado scores (9) for 36 confirmed patients were between 2 and 10, the average was 7.86±1.82. Eleven of 36 patients (30.5%) had Alvarado score ≤6. Twenty five of 36 patients (69.4%) had Alvarado score >6.
MRI findings
With reference to Nitta’s criteria, the MRI findings in the diagnosis included thicker walls, high intensity peri-appendiceal effusion and ascites, which are useful indicators of severe appendicitis. In our cases, only 3 of 36 cases had negative finding in MRI. And 33 of 36 showed MRI abnormalities. Among them, 25 (75.8%) cases demonstrated an appendiceal wall thickness of >2 mm; 23 (69.7%) cases had an appendix cavity diameter of >6 mm; 25 (75.8%) cases showed a high signal on the T2W image in the appendiceal wall and peri-appendiceal effusion (Table 2). Overall, the diameter of the appendiceal cavity measured by MRI was 0.805±0.205 cm; the thickness of the appendiceal wall was 0.318±0.106 cm. These met the diagnostic criteria for acute appendicitis.
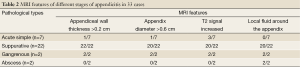
Full table
Sensitivity and specificity for detecting acute appendicitis
In this study, 41 cases of suspected acute appendicitis were evaluated with an MRI examination. Applying the above criteria, 33 of 41 cases (true-positive) were diagnosed with acute appendicitis by MRI, and 36 of 41 were confirmed by surgery. Five of 41 had confirmed other diseases by surgery, including 1 with ileal diverticulum, 2 with pelvic inflammation, and 2 with acute gastroenteritis. Thus, the sensitivity and specificity were 91.7% and 100%, respectively (Table 3).
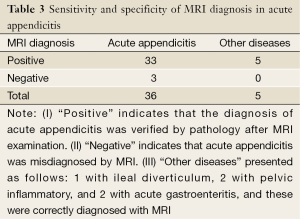
Full table
Preoperative localization in acute appendicitis by MRI
We determined the exact anatomic location of the appendix by MRI images. The MRI positioning, as shown in Figure 1, documented the appendix being located at one of the following areas: (I) retrocecal, (II) pelvic, (III) preileal, (IV) postileal, and (V) subcecal. The position suggested by MRI and the surgery finding were in 100% agreement.
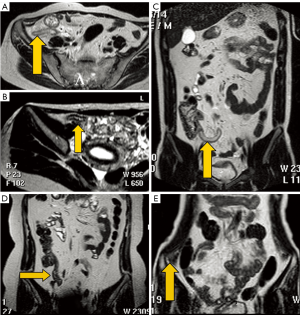 Figure 1. Positions of the appendix. The appendix was located at the following areas. A. post-ileal; B. pre-ileal; C. subcecal; D. pelvic; E. retrocecal
Figure 1. Positions of the appendix. The appendix was located at the following areas. A. post-ileal; B. pre-ileal; C. subcecal; D. pelvic; E. retrocecal Staging of appendicitis by MRI
Based on the results of this study, we are the first group of investigators who were able to characterize the various stages of appendicitis as (I) simple appendicitis, (II) suppurative appendicitis, (III) gangrenous appendicitis, or (IV) appendiceal abscess with MRI. In the post-operative diagnosis of 33 patients with positive MRI findings, 7 had acute simple appendicitis, 22 had suppurative appendicitis, 2 had gangrenous appendicitis, and 2 had an appendicular abscess. Table 2 shows the four important MRI features of these four stages. These stages are illustrated in Figures 2 and 3.
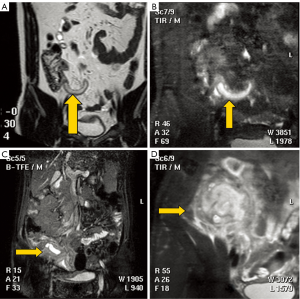 Figure 2. The staging of appendicitis. A. Acute simple appendicitis with a thick-walled appendix >0.3 cm in a 27-year-old man. Coronal MR images show a dilated appendix (arrow) lateral to the cecum, with a slightly thickened appendix wall. The appendix is of long T2 signal in T2W image without surrounding local effusion; B. Suppurative appendicitis with a cavity diameter >0.6 cm in a 47-year-old man. A SENSE-BTFE-SPIR image demonstrates that the appendiceal cavity is enlarged and T2 signal increased in the cavity with appendiceal wall thickening and surrounding local effusion; C. Gangrenous appendicitis in a 35-year-old woman; D. An appendicular abscess in a 55-year-old woman. Gangrenous appendicitis and appendicular abscess both show ileocecal-encapsulated high signals, and the appendix is unclear in these stages
Figure 2. The staging of appendicitis. A. Acute simple appendicitis with a thick-walled appendix >0.3 cm in a 27-year-old man. Coronal MR images show a dilated appendix (arrow) lateral to the cecum, with a slightly thickened appendix wall. The appendix is of long T2 signal in T2W image without surrounding local effusion; B. Suppurative appendicitis with a cavity diameter >0.6 cm in a 47-year-old man. A SENSE-BTFE-SPIR image demonstrates that the appendiceal cavity is enlarged and T2 signal increased in the cavity with appendiceal wall thickening and surrounding local effusion; C. Gangrenous appendicitis in a 35-year-old woman; D. An appendicular abscess in a 55-year-old woman. Gangrenous appendicitis and appendicular abscess both show ileocecal-encapsulated high signals, and the appendix is unclear in these stages 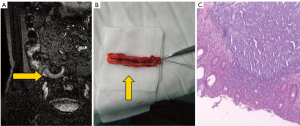 Figure 3. A case of suppurative appendicitis with a cavity diameter >0.6 cm in a 47-year-old man. (A) shows the SENSE-BTFE-SPIR image demonstrates that the appendiceal cavity is enlarged, and T2 signal increased in the cavity with appendiceal wall thickening and surrounding local effusion. (B) and (C) show the histopathological results for this confirmed suppurative appendicitis
Figure 3. A case of suppurative appendicitis with a cavity diameter >0.6 cm in a 47-year-old man. (A) shows the SENSE-BTFE-SPIR image demonstrates that the appendiceal cavity is enlarged, and T2 signal increased in the cavity with appendiceal wall thickening and surrounding local effusion. (B) and (C) show the histopathological results for this confirmed suppurative appendicitis Discussion
Modern MRI equipment possesses excellent contrast resolution, which enables the recognition of the inflammatory process more accurately than other imaging modalities without using ionizing radiation (2). Furthermore, and of great importance, the images can be post-manipulated into any of a variety of planes to assist in obtaining a 3-dimensional evaluation of the appendix and the processes surrounding it. Finally, MRI is much more effective than CT scans in delineating the edematous processes that may begin once the appendix undergoes initial inflammation and passes through the various stages prior to and including rupturing and abscess formation.
In our study, we used an ultrafast sequence, SENSE-BTFE-SPIR, in detecting appendicitis. BTFE is one of steady state free precession (SSFP) sequences (12). Very fast imaging in milliseconds can be achieved by BTFE sequences using a large flip angle and very short time of repetition (TR) (13). Furthermore, another technique, k-space and time (k-t) sensitivity encoding (SENSE) imaging (14), can be combined with BTFE to further reduce both maternal and fetal motion artifact as well as subject discomfort. High quality images in appendix MRI without resultant aliasing can be generated from this ultrafast sequence through a combination of SENSE and BTFE. In order to suppress the fat surrounding the appendix with enhancing the edematous signal, we tried to combine the BTFE with SPIR. Consequently, the sequences we used in this study can show the contrast between appendiceal wall, cavity and the surrounding tissue without motion artifact. This is, to our knowledge, the first clinical study to evaluate SENSE-BTFE-SPIR of MRI in patients with appendicitis.
In our MR protocol, we used sequences with SENSE-BTFE-SPIR and T2W-DRIVE obtained predominantly of T2-weighted fast sequences. Imaging of the bowel was shown to be superior with fast SE MRI because the short imaging time minimized artifacts due to peristalsis and the long T2 relaxation time of the luminal contents created high-resolution images of the mucosal surfaces. It is possible that SENSE-BTFE-SPIR sequences with addition of fat suppression may also be sensitive in the detection of inflammation.
Definitive visualization of the normal appendix is very important for reducing false-positive rate with unnecessary appendectomy. In our study, the appendiceal cavity measured an average diameter of 0.805+/-0.205 cm, with an average appendix thickness of 0.318+/-0.106 cm, which is similar to that reported by Nitta (10). The purpose of our study was to obtain further details regarding the diagnosis of acute appendicitis with MRI. Using this standard for the diagnosis of acute appendicitis, the sensitivity and specificity were 91.7% and 100%, respectively. MRI significantly improved the diagnosis of acute appendicitis and was determined to might be superior to abdominal CT scans and ultrasounds (15-17).
Based on our work, it is clear that MRI provides important information on the phases of appendiceal inflammation. In the post-operative diagnosis of 33 patients with positive MRI findings, 7 had acute simple appendicitis, 22 had suppurative appendicitis, 2 had gangrenous appendicitis, and 2 had an appendicular abscess. An MRI of the phases of appendiceal inflammatory processes also provides the following important information: (I) acute simple appendicitis mainly shows an increased T2 signal in the appendiceal wall and no surrounding local effusion; (II) suppurative appendicitis shows an expansion of the appendiceal cavity with an increased T2 signal in the cavity per se, along with appendiceal wall thickening, an increased signal in the appendiceal wall, and local effusion surrounding the appendix; (III) gangrenous appendicitis and (IV) appendicular abscess both show ileocecal-encapsulated high signals, with the appendix disappearing in these stages (10,15).
The limitations of this study include the sample size is still small, and also the study population is highly selected, and therefore the true sensitivity and specificity of the described technique in more general patients remain unknown.
In conclusion, MRI can effectively document the various stages of appendicitis, along with the pathological changes in the surrounding tissue that accompany its complications. MRI greatly improves the pre-operative diagnosis, especially when the typical clinical manifestations of appendicitis do not present in all patients. Furthermore, MRI can make a differential diagnosis between simple appendicitis and appendiceal abscess, thus enhancing clinical treatment programs, reducing diagnostic ambiguity, eliminating unnecessary appendectomies, and reducing complications due to delayed surgery, resulting in perforation. This study suggests that SENSE-BTFE-SPIR in cases of suspected acute appendicitis might be a complementary sequence in appendix MRI (3,18).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Inci E, Hocaoglu E, Aydin S, et al. Efficiency of unenhanced MRI in the diagnosis of acute appendicitis: comparison with Alvarado scoring system and histopathological results. Eur J Radiol 2011;80:253-8. [PubMed ]
- Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg 2008;32:1843-9. [PubMed ]
- Inci E, Hocaoglu E, Aydin S, et al. Efficiency of unenhanced MRI in the diagnosis of acute appendicitis: comparison with Alvarado scoring system and histopathological results. Eur J Radiol 2011;80:253-8. [PubMed ]
- Israel GM, Malguria N, McCarthy S, et al. MRI vs. ultrasound for suspected appendicitis during pregnancy. J Magn Reson Imaging 2008;28:428-33. [PubMed ]
- Khanal BR, Ansari MA, Pradhan S. Accuracy of ultrasonography in the diagnosis of acute appendicitis. Kathmandu Univ Med J (KUMJ) 2008;6:70-4. [PubMed ]
- Birchard KR, Brown MA, Hyslop WB, et al. MRI of acute abdominal and pelvic pain in pregnant patients. AJR Am J Roentgenol 2005;184:452-8. [PubMed ]
- Oto A, Ernst RD, Shah R, et al. Right-lower-quadrant pain and suspected appendicitis in pregnant women: evaluation with MR imaging--initial experience. Radiology 2005;234:445-51. [PubMed ]
- Leeuwenburgh MM, Laméris W, van Randen A, et al. Optimizing imaging in suspected appendicitis (OPTIMAP-study): a multicenter diagnostic accuracy study of MRI in patients with suspected acute appendicitis. Study Protocol. BMC Emerg Med 2010;10:19. [PubMed ]
- Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 1986;15:557-64. [PubMed ]
- Nitta N, Takahashi M, Furukawa A, et al. MR imaging of the normal appendix and acute appendicitis. J Magn Reson Imaging 2005;21:156-65. [PubMed ]
- Rosai J. Chapter 11: Appendix. In: Ackerman’s Surgical Pathology. St Louis: Mosby, 711-6.
- Kim S, Huh YM, Song HT, et al. Chronic tibiofibular syndesmosis injury of ankle: evaluation with contrast-enhanced fat-suppressed 3D fast spoiled gradient-recalled acquisition in the steady state MR imaging. Radiology 2007;242:225-35. [PubMed ]
- Aydın H, Altın E, Dilli A, et al. Evaluation of jugular foramen nerves by using b-FFE, T2-weighted DRIVE, T2-weighted FSE and post-contrast T1-weighted MRI sequences. Diagn Interv Radiol 2011;17:3-9. [PubMed ]
- Muthurangu V, Lurz P, Critchely JD, et al. Real-time assessment of right and left ventricular volumes and function in patients with congenital heart disease by using high spatiotemporal resolution radial k-t SENSE. Radiology 2008;248:782-91. [PubMed ]
- Wan MJ, Krahn M, Ungar WJ, et al. Acute appendicitis in young children: cost-effectiveness of US versus CT in diagnosis--a Markov decision analytic model. Radiology 2009;250:378-86. [PubMed ]
- Watters JM. The appendicitis inflammatory response score: a tool for the diagnosis of appendicitis that outperforms the Alvarado score. World J Surg 2008;32:1850. [PubMed ]
- Cengiz M, Yildiz F, Selek U, et al. Comment on “computed tomography versus magnetic resonance imaging-based contouring in cervical cancer brachtherapy: results of a prospective trial and preliminary guidelines for standardized contours” by Viswanathan et Al. (Int j radiat oncol biol phys 2007;68:491-498, 2007). Int J Radiat Oncol Biol Phys 2007;69:963; author rply 963-4.
- Chooi WK, Brown JA, Zetler P, et al. Imaging of acute appendicitis and its impact on negative appendectomy and perforation rates: the St. Paul's experience. Can Assoc Radiol J 2007;58:220-4. [PubMed ]


