
Ultrasound (US) of the fingers: anatomy and pathology
Introduction
Ultrasound (US) is one of the most widely used imaging techniques worldwide. Since its origins, following the discovery of ultrasound in 1974 by the Italian biologist Lazzaro Spallanzani while studying bat flight, through the development of sonar during World War II, and up to the adoption of US for medical imaging in the late 20th century as a viable method for diagnosis and treatment, ultrasound has undergone continuous evolution and development (1,2).
Starting in the 1990s, with technological advancements, the entire process became digital, allowing for image visualization on a monitor (2). Following this milestone, the equipment and probes significantly improved in image quality, reduced in cost, and became much easier to handle, making ultrasound the most utilized imaging method outside of radiology, such as in the field of locoregional anesthesia (3).
Currently, we have high-frequency probes that enable us to obtain more detailed information about small and superficial structures, such as the fingers.
The fingers of the hand are one of the most involved parts of the human body in human interaction with their environment, as well as in performing activities of daily living (4). Given their location and function, they are susceptible to various pathologies resulting from leisure and professional activities involving strength and repetitive movements, as well as traumas, which account for 28% of musculoskeletal system injuries (5,6). These pathologies will significantly impair function, making their diagnosis and treatment very important.
US, thanks to its availability, ability to provide detailed information, and capacity for dynamic studies, allows us to expedite the diagnosis of these pathologies. However, the success of the diagnosis largely depends on the experience of the operator. Therefore, the aim of this article is to familiarize the reader with the normal ultrasound anatomy of the fingers, offer some tips for performing US, and review the most common pathologies.
However, it is important to note that exposure to high-frequency US is not without risks (7). Although there are therapeutic methods based on the bioeffects they produce on the mechanical and thermal indices of tissues (8), within the frequency range used for diagnostic purposes, the literature has only described risks associated with exposure during first-trimester pregnancy ultrasound (9).
Sonographic technique
The images in this article are obtained from patients at our center and healthy volunteers using a high-end ultrasound machine and high-frequency linear probes (15–18 MHz), both with basic linear morphology and stick probes.
The patient is positioned seated facing the radiologist, with the hand placed on the examination table in a suitable position to obtain images of the area of interest in both transverse and longitudinal planes.
It is important to remember to always apply ample gel on superficial and small structures for optimal visualization.
Regarding the dynamic study, specific guidelines will be provided in the pathology exploration section.
Extensor region
Normal anatomy
The extensor mechanism of the fingers involves zones I to V of the Verdan zones (Figures 1,2) and has a complex anatomy. Its proper function depends on coordinated activity between the intrinsic muscles of the hand (interossei and lumbricals) and the extensor tendons.


The extensor tendon is formed by a central band that runs along the dorsal aspect of the phalanges and inserts distally at the base of the middle phalanx (MP) to extend the proximal interphalangeal (PIP) joint, but requires other components to stabilize the tendon and achieve extension of the distal interphalangeal (DIP) joint.
At the level of the metacarpophalangeal (MCP) joint, the extensor tendons are stabilized by the extensor hood, a fibrous triangular expansion located on the dorsal aspect of the proximal phalanx (PP) receiving fibers from the intrinsic muscles and merging with the extensor tendons. Its main component is the sagittal bands, fibrous bands starting from the volar plate and inserting into the extensor tendon.
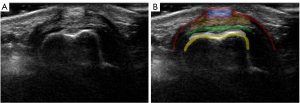
On US, the extensor hood appears as a thin echogenic fibrous structure (2 mm) covering the dorsal surface of the finger (10). In the longitudinal plane, only a linear echogenic band parallel to the finger is observed, while in the transverse plane, the typical “seagull” image can be seen (5), where the extensor tendon forms the body of the seagull and the sagittal bands are the wings, visualized as echogenic flattened extensions on both sides of the extensor tendon (Figure 3).
Distal to the sagittal bands, the extensor tendons continue divided into three parts: the central band described earlier and two lateral bands mostly formed by the intrinsic muscles of the hand, which also send fibers to contribute to the central band. Once the lateral bands receive the contribution from the intrinsic muscles, they are called conjoint tendons and converge distally to form the terminal tendon, which inserts at the base of the distal phalanx (DP).
The triangular ligament is located between the distal conjoint tendons and maintains these structures dorsal to the axis of rotation of the DIP (6,11).
On US, the central band can be observed in the longitudinal plane until its insertion at the base of the MP and the terminal tendon with its insertion at the DP appear as hyperechoic structures traversing the subcutaneous cellular tissue over the echogenic bone cortex, while the two lateral bands are barely visible (11) (Figure 4).

Finally, at the terminal and dorsal aspect of the fingers, we encounter the nail, formed by the nail unit (plate, bed, and matrix) and the periungual zone (folds):
- The nail plate is a bilaminar structure composed of the dorsal and ventral lamina, originating in the middle third of the phalanx. These bands are seen on ultrasound as two parallel hyperechoic lines separated by a hypoechoic virtual space called the interplate space. The thickness of the plates varies between 0.3 and 0.65 mm.
- The nail bed appears as a homogeneous hypoechoic band between the plate and the highly vascularized dorsal cortical bone of the DP on Doppler mode. Its average thickness is 1.5 mm and should be measured in the middle third of the phalanx.
- The nail matrix or root is located below the proximal fold. It is observed as a triangular structure with a proximal convex margin to the bed and hyperechoic compared to it. Its length varies between 1 and 5.3 mm.
- The periungual tissues are divided according to their location into proximal fold (eponychium), lateral folds (perionychium), or distal fold (hyponychium) (6,12).
Pathology
Injuries to the extensor tendons are more common than those of the flexors due to their superficial location. They usually occur due to trauma, whether open or closed, and to a lesser extent, spontaneous lesions secondary to inflammatory processes. Complete tendon ruptures typically do not result in significant retraction due to their complex insertion system (13).
We will address extensor tendon pathology from proximal to distal and based on their location in the Verdan zones.
Zone V: sagittal band rupture (boxer’s knuckle)
This occurs due to direct trauma (boxers) or repetitive microtrauma to the MCP joint, although it can also be seen in patients with inflammatory arthropathy without a previous traumatic history. The most affected finger is usually the 3rd, with the radial band involved, resulting in the tendon dislocating ulnarly.
On US, it is better observed in the transverse plane, and dynamic study is essential to demonstrate tendon dislocation during MCP joint flexion-extension. We will observe an increase in caliber and alteration of the echogenic structure of the affected sagittal band and the underlying joint capsule. The extensor tendon may appear normal or enlarged with loss of its fibrillar pattern if there is a fibrillar tear. Increased vascular flow may also be observed on Doppler mode secondary to inflammatory changes (5) (Figure 5).

It is important to remember that the 2nd and 5th fingers have two extensor tendons, so they can dislocate in different directions, one radially and the other ulnarly (11).
Zone III: central extensor band rupture (boutonniere deformity)
Rupture of the central band at its insertion at the base of the MP occurs after direct trauma, violent flexion, or volar dislocation of the PIP joint. In the subacute or chronic phase of the injury, since the lateral bands are intact, they shift volarly relative to the axis of the PIP joint, creating a loop through which the MP head moves, causing flexion of the PIP joint and forced extension of the DIP joint (13).
On US, it is better observed in the longitudinal plane, and dynamic study of isolated PIP joint flexion with DIP joint block is essential. We will observe thickening of the central extensor tendon band with heterogeneous echogenic structure, associated or not with bony avulsion at its distal insertion, possibly demonstrating discontinuity of its fibers in dynamic study (5) (Figure 6).

Zone I: terminal extensor band rupture (mallet finger)
Rupture of the terminal tendon at its distal insertion into the DP most commonly occurs after closed trauma with forced flexion of the DIP joint, associated or not with an avulsed bony fragment (Figure 7), resulting in mallet finger deformity due to inability to extend the DIP joint.

On US, it is better observed in the longitudinal plane with an increase in caliber and alteration of the echogenic structure of the terminal tendon, associated or not with bony avulsion. Dynamic study with passive flexion-extension of the DIP joint is essential to demonstrate complete ruptures.
Regarding the nail region, we will discuss its pathology without delving into the tumors and pseudotumors section.
Flexor region
Normal anatomy
The flexor complex consists of two tendons: the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP), which run through the volar region of the fingers within the digital canal from the metacarpal heads to their distal insertion.
Proximal to the proximal phalanx (PP), both tendons run one on top of the other, with the FDS being more volar in location. However, at the level of PP, the FDS divides into two tendons that lie on either side of the FDP, which then locates itself in the most volar position until its distal insertion at the base of the DP.
After the division into two tendon bands, the FDS reunites deeply with the FDP, forming a pulley, inserting into the proximal third of the MP. Upon insertion, both bands form a crossing of fibers known as the Camper’s chiasm (5,6).
Sometimes, it is challenging to visualize the tendons separately in the longitudinal and transverse planes on US, but with dynamic study and manipulation of artifacts due to anisotropy, we can individualize the tendons (Figure 8). For isolated study of the FDS, in the dynamic study, we will block the rest of the fingers in extension with our hand, and for the FDP, we will only block the PIP joint.

In the digital canal, the tendon sheaths have fibrous reinforcement called pulleys that fix them to the phalanges and maintain the tendons in their anatomical position.
In three-phalanx fingers, we have two types of pulleys: annular pulleys, thicker and more potent (from proximal to distal A1–A5), and cruciform pulleys with a lesser mechanical role (from proximal to distal C1–C3) (Figure 9). Pulleys A2 and A4 are the most important.

In the first finger, we have three constant pulleys: two annular pulleys (A1 and A2) and one oblique (C1), which is an expansion of the thumb adductor and the most important functionally. A variable fourth annular pulley (Av) distal to A1 has been described (5,6).
In US, the most accessible pulleys are A1 and A2, observed as a thin hypoechoic linear band overlying the flexor tendons, with a diameter not exceeding 0.62 mm (14) (Figure 10).

Pathology
Injuries to the flexor tendons are less frequent, and the mechanism of action is like that of the extensor tendons. The lesions can occur in both tendons or separately. It’s important to note that in complete ruptures, there will be retraction of the tendon ends, which depends on the degree of finger flexion at the time of injury (13). For this reason, the International Federation of Societies for Surgery of the Hand (IFSSH) establishes a topographic division of the flexor region of the hand and fingers (Figure 11), to improve the diagnosis and treatment of injuries.

We will address flexor tendon pathology from proximal to distal and based on their location in the IFSSH zones (Zones II and I).
Zones II and I
Tenosynovitis
It is the inflammation of the tendon sheath and can be inflammatory, mechanical, or infectious in nature.
On US, it appears as a hypoechoic halo around the flexor tendons, which acquires a lobulated morphology adapting to the arrangement of the pulleys. Often, the findings are overlapping in different etiologies, so they should be interpreted in the clinical context of the patient. Additional findings such as synovial proliferation, hyperechoic content in the tendon sheath, increased vascular flow on Doppler mode, presence of foreign bodies, and skin wounds help make an accurate diagnosis (Figure 12). Remember that the digital sheaths of the 1st, 2nd, and 5th fingers continue with the common sheath at the wrist during examination.

Pulley rupture (Climber’s finger)
Injuries to the pulleys, both due to overuse and complete ruptures, are common in climbing, where the athlete places their entire weight on their fingers during grip, exerting loads on the pulley system of up to 700 N (15). They have also been described in other sports.
They are more frequent in the 2nd and 4th fingers and in pulleys A2 and A4. These injuries can be isolated or combined. In the latter, when complete ruptures of pulleys A2, A3, and A4 are associated, we can clearly observe the bowstring deformity of the finger during physical examination.
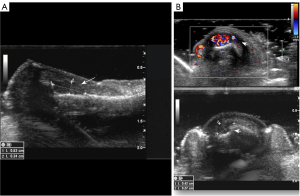
Dynamic US has shown a sensitivity of 98% and a specificity of 100% for detecting finger pulley injuries (15). The diagnostic image is the presence of a separation of more than 1 mm between the flexor tendon and the phalanx cortex, which becomes more apparent in the dynamic study with flexion against resistance, and the more pulleys that are injured, the more noticeable it is (5,15). Soft tissue swelling and increased vascular flow on Doppler mode in adjacent soft tissues may also be observed (Figure 13).

Trigger finger
Trigger finger is a common hand disorder characterized by the trapping, snapping, or locking of the flexor tendon of the affected finger. The lifetime risk of developing trigger finger is 2% to 3% (16).
It is considered a stenosing tenosynovitis of pulley A1, generating a space conflict between the sheath and the tendon. This conflict causes friction and inflammation of the tendon and pulley until the triggering occurs with a painful click during passive extension (5,13). Its etiology is controversial and it usually affects the 1st, 3rd, and 4th fingers more frequently.
On US, we observe thickening of pulley A1 (>0.62 mm), associated or not with increased vascular flow on Doppler mode and with an increase in caliber of the adjacent tendon. We may also observe the presence of cysts and nodular thickening of the tendon sheath (Figure 14).

Zone I: distal flexor digitorum profundus (jersey finger)
Injuries to the FDP occur during active finger flexion and subsequent abrupt and passive hyperextension. It usually occurs in contact sports such as football or rugby, hence its name, as the finger gets caught in the opponent’s jersey. It may or may not be associated with an avulsed bony fragment and tendon retraction. The most affected fingers are the 3rd and 4th.
On US, partial ruptures show an increase in caliber and alteration of the echogenic structure of the tendon, while complete ruptures show irregularity of the cortex with or without avulsed fragment, tendon retraction with an empty tendon sheath, and marked posterior acoustic shadowing at the tendon stump (11) (Figure 15).

Joints
Normal anatomy
The MCP and PIP joints are hinge-type diarthroses with the capacity for flexion and extension, stabilized by the volar plate and collateral ligaments (CL).
There are two CLs: the proper CL and the accessory CL. The proper CL is taut in flexion, preventing radial and ulnar deviation at the joint. The accessory ligaments have a volar insertion where they merge with the volar plate and tense in extension.
The CLs of the PIP joints are accessible with US and are best studied in the longitudinal plane, appearing as a hypoechoic linear band crossing the joint. The examination of the MCP joint ligaments is limited to the transverse plane, except for the 1st finger, the radial collateral of the 2nd finger, and the ulnar collateral of the 5th finger.
In the 1st finger, the MCP joint is reinforced by the CLs, the volar plate/sesamoids complex, and the adductor aponeurosis that runs above the ulnar collateral ligament (UCL), which can be distinguished on ultrasound as a thin band covering the UCL (6,11).
The volar plate is a fibrocartilaginous structure with a lax proximal insertion on the head of the PP and a firm distal insertion on the base of the DP.
On US, it appears as a triangular, hyperechoic structure located between the joint and the flexor tendons (Figure 16).

Pathology
Rupture of the volar plate
These are more common in the PIP joint and occur due to a mechanism of hyperextension and/or dorsal dislocation of the joint, resulting in a flexion deformity. They may be associated with an avulsed bone fragment at their distal insertion.
On US, it appears as a loss of its triangular morphology and alteration of the echostructure. Performing a dynamic study with passive hyperextension of the PIP joint aids in diagnosing complete ruptures (Figure 17).

UCL of the 1st finger (skier’s thumb/ranger’s thumb and Stener lesion)
Injury to the UCL of the 1st finger occurs at its distal insertion due to hyperabduction with hyperextension of the MCP joint.
When the tendon remains in its anatomical position, conservative treatment may be suitable, termed skier’s thumb/ranger’s thumb. However, if the ligament displaces and the adductor aponeurosis becomes interposed between it and its distal insertion, it is considered a Stener lesion, requiring surgical treatment.
On US, we observe partial or complete non-displaced injuries with thickening of the UCL, alteration of its echostructure, and increased vascular flow on Doppler mode.
Displaced ruptures appear as a hypoechoic round mass proximal to the joint, corresponding to the displaced and retracted end of the UCL over the adductor aponeurosis, forming the “yo-yo sign” (5,11). Dynamic study with passive flexion of the MCP joint to move the adductor aponeurosis aids in diagnosis (Figure 18).

Tumors and pseudotumors
Ganglions
They represent the most common lesion in the hand and fingers. Ganglions are hard nodular lesions due to their mucoid content and are most frequently located in the volar region of the tendons and joints of the fingers. They are more common in young adults and three times more common in women (17).
On US, ganglions appear as anechoic nodular or polycyclic masses with posterior acoustic enhancement and no vascular flow on Doppler mode. They may present thin septa and echoes within. It is important to try to demonstrate their neck/communication with the joint or tendon sheath (18) (Figure 19).

Palmar fibromatosis (Dupuytren’s disease)
This is the most common type of fibromatosis, occurring in approximately 1–2% of the general population and may be bilateral in 42–60% of cases (11). It is common in the elderly and is localized at the base of the 4th and 5th fingers. On physical examination, it appears as subcutaneous nodules on the palmar surface, progressing slowly to fibrous cords and causing traction on the skin and flexor tendons, resulting in finger flexion contractures (13).
On US, palmar fibromatosis appears as hypoechoic nodular thickening of the palmar aponeurosis located between the skin and flexor tendons (Figure 20). They usually do not show significant vascularity on Doppler mode. Dynamic study reveals adhesions between the palmar fibromatosis and the flexor tendon during finger movements (11).

Foreign bodies
Foreign bodies are very common in the hands and fingers, presenting on physical examination as nodular masses/lesions, as they are often associated with granulomas due to foreign body reaction.
On US, foreign bodies appear hyperechoic with different shapes and reverberation artifacts to varying degrees depending on the material they are composed of. They often associate with a hypoechoic perilesional rounded formation with increased vascular flow on Doppler mode, related to granuloma due to foreign body reaction (5) (Figure 21).

Giant cell tumor
This is the most common true neoplasm in the hand and represents the extra-articular extension of pigmented villonodular synovitis. It affects patients between 30 and 50 years old, slightly more common in women.
Giant cell tumors are slow-growing solid masses on the volar aspect of the fingers, causing eccentric displacement of adjacent structures and associated bone erosions in 10–50% of cases (11,13).
On US, they appear as solid, oval, or polycyclic lesions, well-defined, hypoechoic, located in close relationship with the tendon, with varying degrees of vascularity on Doppler mode (Figure 22).

Glomus tumor
It is a hamartoma of the glomus body, which is a special type of arteriovenous anastomosis located in the dermis for thermoregulation. Up to 75% of glomus tumors are in the hand, with up to 65% occurring in the fingertips, predominantly in the subungual space (17), resulting in deformity and discoloration of the overlying nail. Clinically, they present with unbearable pain and sensitivity to temperature (11).
On US, they appear as a small well-defined hypoechoic nodule under the nail bed associated with bone erosion of the adjacent DP and marked vascular flow on Doppler mode (Figure 23).
Conclusions
Since the discovery of US in 1974 and its subsequent adoption as a diagnostic and therapeutic method, ultrasound has undergone significant evolution and development, making it the most widely used imaging method both within and outside of radiology, such as in the field of locoregional anesthesia.
Due to this evolution, it should be considered the technique of choice for diagnosing pathologies in small and superficial structures, such as the fingers. However, it is important to remember that it is an operator-dependent technique, and a thorough understanding of the anatomy and examination technique is necessary for accurate diagnoses.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: With the arrangement by the Guest Editors and the editorial office, this article has been reviewed by external peers.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-591/coif). The special issue “Advances in Diagnostic Musculoskeletal Imaging and Image-guided Therapy” was commissioned by the editorial office without any funding or sponsorship. J.M.V. served as the unpaid Guest Editor of the issue. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kaproth-Joslin KA, Nicola R, Dogra VS. The History of US: From Bats and Boats to the Bedside and Beyond. RadioGraphics 2015;35:960-70. [Crossref] [PubMed]
- Iriarte I, Pedret C. Aspectos generales de la ecografía. En: Ecografía musculoesque-lética Exploración anatómica y patológica. 1o. España: Panamericana, 2020:450.
- Fioccola A, Skerritt CJ. Ultrasound-guided flexor sheath block as a valid alternative to blind techniques for finger pain treatment: the horseshoe sign. Reg Anesth Pain Med 2023;48:375-7. [Crossref] [PubMed]
- Bitar Benítez EM, Gaviria Posada S, León Fernández ND, Gallego Gónima S. Epi-demiología del trauma de miembro superior atendido en seis instituciones de salud de la ciudad de Medellín, Colombia, en 2016. Cir Plástica Ibero-Latinoam. septiembre de 2021;47:323-32.
- Bueno Horcajadas Á, Del cura Rodriguez JL. Ecografía musculoesquelética esencial. Panamericana, 2011:297.
- Landeras R, Gallardo E. Anatomía normal y ecografía de la mano y los dedos. En: Ecografía musculoesquelética Exploración anatómica y patológica. 1o. España: Panamericana, 2020:450.
- Gómez-Cano Hernández, Manuel. Ministerio de trabajo y economía social. NTP 205: Ultrasonidos: exposición laboral. Available online: https://www.mites.gob.es/es/extras/buscador/resultados.htm?q=esposici%C3%B3n+ultrasonidos&buscar.x=0&buscar.y=0&hl=es
- Kim YS, Rhim H, Choi MJ, Lim HK, Choi D. High-intensity focused ultrasound therapy: an overview for radiologists. Korean J Radiol 2008;9:291-302. [Crossref] [PubMed]
- Arenas Ramírez J, Puerto Navarro B, Puente Águeda JM, Sainz Bueno JA, Álvaro Navidad M. Guía de la exploración ecográfica del I trimestre. Prog Ginecol Obstet 2022;65:240-90.
- Lee JC, Healy JC. Normal sonographic anatomy of the wrist and hand. Radiographics 2005;25:1577-90. [Crossref] [PubMed]
- Lee SA, Kim BH, Kim SJ, Kim JN, Park SY, Choi K. Current status of ultrasonography of the finger. Ultrasonography 2016;35:110-23. [Crossref] [PubMed]
- Aluja Jaramillo F, Quiasúa Mejía DC, Martínez Ordúz HM, González Ardila C. Nail unit ultrasound: a complete guide of the nail diseases. J Ultrasound 2017;20:181-92. [Crossref] [PubMed]
- Gallardo E, Laneras R. Patología de la manos y los dedos. En: Ecografía musculo-esquelética Exploración anatómica y patológica. 1o. España: Panamericana, 2020:450.
- Flores DV, Murray T, Jacobson JA. Diagnostic and Interventional US of the Wrist and Hand: Quadrant-based Approach. Radiographics 2023;43:e230046. [Crossref] [PubMed]
- Klauser A, Frauscher F, Bodner G, Halpern EJ, Schocke MF, Springer P, Gabl M, Judmaier W, zur Nedden D. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology 2002;222:755-61. [Crossref] [PubMed]
- Mifune Y, Inui A, Sakata R, Harada Y, Takase F, Kurosaka M, Kokubu T. High-resolution ultrasound in the diagnosis of trigger finger and evaluation of response to steroid injection. Skeletal Radiol 2016;45:1661-7. [Crossref] [PubMed]
- Nepal P, Songmen S, Alam SI, Gandhi D, Ghimire N, Ojili V. Common Soft Tissue Tumors Involving the Hand with Histopathological Correlation. J Clin Imaging Sci 2019;9:15. [Crossref] [PubMed]
- Horcajadas AB, Lafuente JL, de la Cruz Burgos R, Muñiz SH, Roca SA, Ortega SG, Franjo PD, Cruz EO. Ultrasound and MR findings in tumor and tumor-like lesions of the fingers. Eur Radiol 2003;13:672-85. [Crossref] [PubMed]


