
Magnetic resonance classification proposal for medial gastrocnemius muscle injuries
Introduction
Calf muscle injuries are frequent among both professional and amateur athletes and occupational groups (1,2). Recovery times are highly variable, lasting from a few months to years, depending on the site and severity of the injury (1,3-5). Therefore, an accurate diagnosis at the time of injury is a crucial step for the outcome of injured athletes.
Sonography and magnetic resonance imaging (MRI) are essential in the approach of muscular sports injuries that would otherwise be treated clinically. To this purpose, image-guided severity classifications of muscle injuries have been developed and become increasingly important in the overall assessment of lesions (6-8). However, general classifications of muscle injuries do not completely take into account the complexity of injuries of the medial head of the gastrocnemius especially because of its histological features and anatomic variability (9). The distal part of the distal gastrocnemius consists of a complex anatomy given the organization of the connective tissue (10,11). At this level, the anterior and posterior aponeurosis of the medial gastrocnemius, in conjunction with the soleus aponeurosis (SA), converge to form the “free gastrocnemius aponeurosis” (FGA), which ultimately integrates with the Achilles tendon (10,11).
Based on the understanding of these particular characteristics, Pedret et al. (12) proposed an ultrasound (US) classification to determine the type of injury according to its location and characteristics. Depending on their location, the lesions can be myoaponeurotic, aponeurotic or mixed, demonstrating different prognoses regarding the time to return to play or to work activities (12).
In the last decade, MRI has proven to be very useful in the diagnosis and evolution of muscle injuries given its high ability to discriminate connective tissue (13-15). Sergot et al. (16) proposed a classification that includes the muscle groups of the triceps surae with prognostic correlation according to the degree of connective tissue involvement, without considering the specific location of the injury based on the characteristics of each muscular belly.
Hence, considering the widespread acceptance and clinical utility of the recent US classification specifically targeting the distal portion of the medial gastrocnemius (12), we aimed to develop an MRI protocol facilitating the US translation of injury types to MRI modality. This clinical practice educational review endeavor seeks to enhance the understanding and application of precise diagnostic methodologies for calf muscle injuries, particularly focusing on their localization and characteristics within the mentioned anatomical context.
Normal anatomy and US-MRI correlation
The distal anatomy of the triceps surae exhibits numerous distinctive features that largely determine the occurrence of diverse injury patterns within the myoconnective complex. Understanding the distribution of normal myoconnective tissue is crucial for a comprehensive understanding of injuries (17-20). Both the medial and lateral heads of the gastrocnemius converge to form a singular broad aponeurosis, known as the anterior gastrocnemius aponeurosis (GA), located deeply across both muscle bellies. Generally, the GA has an area free of muscle fibers (FGA) just proximal to its junction with the SA. Distally, the FGA converge with the posterior SA to create the Achilles tendon (10,11).
The aponeuroses appear as echogenic linear structures surrounding these muscular bellies in US examination, whereas in MRI, they present markedly hypointense signals in T1 and fluid-sensitive sequences (13). Given the intermediate signal and echogenicity of the muscle fibers, the interface of the myoconnective junction is easily visualized with both techniques (12,13). However, the pattern of muscle fiber pennation, typically parallel in this location, is clearly visible through US but is not evaluable by MRI under normal conditions.
Finally, the biomechanical characteristics of the musculature at this level should be considered. Because of the presence of connective and fibroadipose tissue in the intermuscular space between the posterior aponeurosis of the soleus and the anterior aponeurosis of the gastrocnemius, there is synchronization in the movement of these muscle bellies during dorsal-flexion foot maneuver.
MR indications
MRI allows identification of the affected histoarchitecture and the magnitude of a muscle injury (13). MRI is generally recommended for deep muscle injuries that are difficult to evaluate by US and are suspected that will require a prolonged recovery time (13,21,22). Despite the superficial nature of the medial gastrocnemius and the extended and variable recovery time periods of this muscle injuries, the ability of MRI findings to assess the time to return to play and the risk of reinjury (14) has contributed significantly to the growing popularity of this imaging technique in the professional sports world due to the specificity for studying the connective tissue. Likewise, MRI has allowed the identification of milestones in the healing process following a muscle injury (15), enabling the translation of those histological features described by Järvinen et al. (23-25). Nevertheless, determining the clinical necessity of a diagnostic MRI should be established case-by-case (21). The primary limitations of MRI include its cost, higher length of examination compared to US, and occasional feeling of claustrophobia reported by some patients. In terms of monitoring, US allows early detection of the onset of delayed hematomas and complications frequently reported as deep venous thrombosis.
MRI protocol
Utilizing a 3 Tesla MRI or an optimized 1.5 Tesla system enables specialists to precisely define muscle injuries, acquiring images in two planes, including static and dynamic acquisitions. The examination is specifically focused around the region marked with a skin vitamin marker, based on clinical findings. The patient is prepared by placing an MRI sand bag under the leg at the level of the distal portion of the Achilles tendon. The flex coil is positioned on the leg (in supine position) strongly attached to maintain the extremity fixed preventing translational motion but allowing foot dorsiflexion. It is recommended to use a multipurpose surface coil for MRI to achieve higher resolution images. Our recommended protocol consisting of 3 sequences: two fat-suppressed intermediate-weighted [echo time (TE) range, 40–65 ms] sequences (axial and sagittal planes), and a T1-weighted sequence in the axial plane. The intermediate-weighted fluid sensitive sequences provide excellent contrast and spatial resolution of the connective tissue (13). Tailoring protocols is advised to ensure thin sections (e.g., less than 3 mm), appropriately small field of view (FOV) (13), and multiplanar acquisitions (axial, and sagittal). Then, we perform a dynamic examination with true fast imaging with steady-state free precession (TRUFI) cine imaging, looking for the asynchronous motion of the gastrocnemius and soleus muscles during ankle dorsiflexion and plantarflexion maneuvers. Table 1 shows the recommended parameters.
Table 1
| Parameters | MRI characteristics | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Axial fat-suppressed TSE intermediate-weighted image | Axial TSE T1-weighted image | Sagittal fat-suppressed TSE intermediate-weighted image | Sagittal TRUFI-cine T2-weighted image* | ||||||||
| 1.5 T | 3 T | 1.5 T | 3 T | 1.5 T | 3 T | 1.5 T | 3 T | ||||
| Echo time (ms) | 37 | 34 | 9.6 | 9.8 | 39 | 32 | 1.79 | 3.74 | |||
| Slices (number) | 84 | 80 | 84 | 80 | 32 | 25 | 1 (20 acquisitions) | 1 (20 acquisitions) | |||
| Section thickness (mm) | 3 | 3 | 3 | 3 | 3 | 3 | 10 | 10 | |||
| Interslice distance (mm) | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 2.0 | 2.0 | |||
| Field-of-view (cm) | 20×20 | 20×20 | 20×20 | 20×20 | 18×18 | 18×18 | 20×20 | 20×20 | |||
| Repetition time (ms) | 3,850 | 8,770 | 758 | 1,900 | 3,520 | 3,000 | 4.3 | 7.47 | |||
| Flip angle (degrees) | 110 | 138 | 110 | 127 | 180 | 134 | 56 | 30 | |||
| Acquisition matrix | 256×320 | 256×320 | 302×336 | 256×320 | 285×320 | 269×384 | 290×320 | 290×320 | |||
| Bandwidth (Hertz/pixel) | 180 | 180 | 156 | 221 | 135 | 220 | 504 | 300 | |||
| Acceleration factor (R) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | |||
| Scan time (min:s) | 3:08 | 9:58 | 3:12 | 9:13 | 2:22 | 3:08 | 35 s | 58 s | |||
*, dynamic acquisition (foot dorsi-flexion); slices were acquired sequentially. MRI, magnetic resonance imaging; TSE, turbo spin-echo; TRUFI, true fast imaging with steady-state free precession; ms, milliseconds; mm, millimeters; cm, centimeters.
MRI interpretation
MRI fluid sensitive sequences allow the detection of edematous changes around the myoaponeurotic junctions, ensuring an accurate connective tissue assessment, as well as the delineating intramuscular or intermuscular fluid collections or hematomas (13,23,26,27). Areas of hyperintense signal on MRI may reveal disruption of the fibrillar pattern or discontinuities within the aponeuroses, indicating varying degrees of severity (13). Muscle overload is suggested when these areas of hyperintensity in fluid-sensitive sequences are not associate with loss of muscular architecture (13).
T1-weighted sequences are useful in the assessment of subacute hemorrhage or hematoma, in the detection of atrophy and fatty infiltration, and the identification of scar tissue in chronic injuries that may present as chemical shift artifacts in the T2-weighted or fluid-sensitive sequences (13,23).
Another benefit of MRI is its capacity for dynamic study allowing confirmation of the synchronicity of muscle movement, an aspect easily achieved with US as well (12). In dynamic examination using TRUFI cine imaging, it is essential to consider reference points from both the gastrocnemius and soleus muscles to observe synchronization.
Lastly, in cases of injuries assessed for the first time after 7 days of evolution, image interpretation should encompass the evaluation of scar tissue alterations relative to the injury’s temporal progression, along with assessing the presence or absence of an intermuscular hematoma (15). This is another potential value of the MRI classification here described.
Proposed MRI classification
Hereafter are delineated the MRI findings corresponding to the various types of injury severity according to the US classification proposed by Pedret et al. (12). Using MRI, we can also identify 4 types of injuries based on the recognition of images from fluid-sensitive sequences, such as: disruption of fibers in areas of muscular hyperintensity, discontinuities in the internal GA, presence and extension of discontinuities in the free aponeurosis, extension of hematomas, and the presence of muscular asynchrony during dynamic acquisition (Table 2).
Table 2
| Types | Location of damage | Imaging findings | |
|---|---|---|---|
| US signs | MRI signs | ||
| 1 | Muscular myoaponeurotic injury | Morphologic and echostructural alteration of muscle fascicles and the interposed fibro-adipose septa | Area of feathery edema is observed in the fibers anchored to the aponeurosis in fluid-sensitive sequences |
| 2A | Gastrocnemius aponeurotic injury (<50%) | Morphologic and echostructural alteration of the aponeurosis continuity, as well as evidence of morphologic and echostructural alteration of muscle fascicles. Small hypo-anechoic collection (hematoma). Synchronous motion of the gastrocnemius and soleus muscles | Increased signal area at the myoaponeurotic junction, along with irregularity in the fibrillar pattern of the anchorage and a clear discontinuity in the aponeurosis at that level. Small liquid-signal accumulation (hematoma). Synchronous motion of the gastrocnemius and soleus muscles |
| 2B | Gastrocnemius aponeurosis injury (>50%) | Morphologic and echostructural alteration of the aponeurosis continuity, as well as evidence of morphologic and echostructural alteration of muscle fascicles. Large hypo-anechoic accumulation (hematoma). Usually, asynchronous motion of the gastrocnemius and soleus muscles | Increased signal area at the myoaponeurotic junction, along with irregularity in the fibrillar pattern of the anchorage and a clear discontinuity in the aponeurosis at that level. Large liquid-signal accumulation (hematoma). Usually, asynchronous motion of the gastrocnemius and soleus muscles |
| 3 | FGA injury | Morphologic and echostructural alteration of the FGA. Synchronous motion of the gastrocnemius and soleus muscles | Exclusively a FGA discontinuity, and a small amount of fluid tends to accumulate superficially, although significant hematomas are not present. Synchronous motion of the gastrocnemius and soleus muscles |
| 4 | Mixed injury | Combination of US findings of 2B and 3 types | Combination of MRI findings of 2B and 3 types |
MRI, magnetic resonance imaging; US, ultrasound; FGA, free gastrocnemius aponeurosis.
Type 1: muscular myoaponeurotic injury
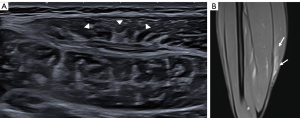
In this type of injury, an area of feathery edema is observed in the fibers anchored to the aponeurosis in fluid-sensitive sequences, without any discontinuities (Figure 1). However, the aponeurosis might appear slightly thickened with minimal loss of its normal signal on MRI. Similar to US, MRI displays gastrocnemius-soleus synchrony during dynamic maneuvers.
Type 2: gastrocnemius aponeurotic injury
In fluid-sensitive sequences, this type of injury presents an increased signal area at the myoaponeurotic junction, along with irregularities in the fibrillar pattern of the anchorage and a clear discontinuity in the aponeurosis at that level (Figures 2,3). Aponeurosis damage can be continuous, but more commonly by MRI, a ‘tandem’ pattern is observed as multiple focal discontinuities in the affected area. It is further classified into type 2A or 2B based on whether the transversal affected area of the aponeurosis is less than 50% or equal to or greater than 50%, respectively (12). Additionally, the presence of intermuscular hematomas is a characteristic feature (12). The asynchronous motion of the gastrocnemius and soleus muscles is mostly seen in subtype 2B.


Type 3: free GA injury
In this type of injury, there is exclusively an aponeurosis discontinuity and a small amount of fluid tends to accumulate superficially, although significant hematomas are not present (Figure 4). In these cases, MRI has a remarkable capability to determine the extent of connective tissue involvement, distinguishing a complete from a partial thickness tear. In cases with extensive involvement, a slight retraction of the muscular belly may be observed. However, MRI displays gastrocnemius-soleus synchrony during dynamic maneuvers. In these cases, the slight signal changes in the muscle fibers at the myoconnective junction of the calf should not be interpreted as structural damage but rather as an overload.

Type 4: mixed injury
This injury involves over 50% impairment of the GA at the upper myoconnective junction (like type 2B lesions), with a disruption of the free GA (as type 3 lesions) (12). Discontinuities in the connective tissue are visible in fluid-sensitive sequences, along with extensive intermuscular hematomas leaking onto the posterior muscle surface (Figure 5). The asynchronous motion of the gastrocnemius and soleus muscles is a characteristic finding.

Special considerations
Among the differences between US and MRI findings, it is important to highlight the high sensitivity of the MRI technique in detecting tissue signal alterations in fluid-sensitive sequences (13). This sensitivity is particularly useful in type 1 lesions, where signal alteration is more pronounced than structural changes. Notably, the sensitivity of MRI surpasses that of US. However, it is crucial to recognize that, in many cases, these signal alterations result from overload rather than tissue rupture. This underscores the importance of observing the edema pattern and its association with fibrillar pattern disruption or aponeurosis discontinuity.
In certain cases, muscle fiber edema due to overload may be observed in MRI studies without a clear clinical injury correlation. Similarly, when there is suspicion of muscle injury, pure type 3 lesions identified by US might exhibit signs of muscular overload at the myoconnective junction in MRI, without actual tissue damage at that level. This potential discrepancy may induce confusion. However, US is not free from these discrepancies in type 3 lesions; irregularities of the myoaponeurotic junction can be seen that do not correspond to a rupture but rather to retraction or overload secondary to the injury to the free aponeurosis. Nevertheless, in our experience, MRI has demonstrated a remarkable sensitivity in detecting small-sized discontinuities in injuries with few symptoms or low clinical suspicion, which were uncertain in US assessments.
On the other hand, the detection of free aponeurosis and the extent of involvement were more effectively assessed by MRI. This was facilitated by the quantification of thickness through axial acquisitions in fluid-sensitive sequences.
However, despite the valuable insights that dynamic MRI studies can offer, interpreting them might be challenging in instances where the technician lacks familiarity. Nevertheless, this maneuver has proven to be exceedingly easy to execute and interpret.
Recent studies on muscle tissue repair enable us to diagnose delayed muscle injuries (occurring more than 7 days after the initial trauma) by utilizing the milestones of the healing process (15). This empowers us to effectively manage injuries regardless of the timing of the patient’s initial presentation, as long as we correlate it clinically with their medical history.
Conclusions
Both US and MRI are valuable techniques for the examination of distal injuries in the medial gastrocnemius. In this review, we have detailed and illustrated, through medical images, the correlation between US and MRI findings concerning various degrees of muscle involvement. In our clinical practice, we have successfully integrated the recently proposed US classification, complemented by the insights provided by MRI. It is essential to acknowledge the effectiveness of MRI in identifying patterns and the extent of connective tissue damage, particularly aponeurosis, while recognizing the US usefulness in visualizing gastrocnemius-soleus synchrony during foot dorsiflexion. The synergistic use of both modalities enhances our ability to comprehensively assess and manage distal injuries in the medial gastrocnemius.
Acknowledgments
The authors thank radiographers Isaac Pomés (ultrasound technician), and Juan Ramon Sabaté and Marta Soto (MRI technicians). The authors thank Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.
Funding: None.
Footnote
Provenance and Peer Review: With the arrangement by the Guest Editors and the editorial office, this article has been reviewed by external peers.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-298/coif). The special issue “Advances in Diagnostic Musculoskeletal Imaging and Image-guided Therapy” was commissioned by the editorial office without any funding or sponsorship. X.T. served as the unpaid Guest Editor of the issue. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article, the accompanying images and videos.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 2011;39:1226-32. [Crossref] [PubMed]
- Domeracki SJ, Landman Z, Blanc PD, Guntur S. Off the Courts: Occupational "Tennis Leg". Workplace Health Saf 2019;67:5-8. [Crossref] [PubMed]
- Werner BC, Belkin NS, Kennelly S, Weiss L, Barnes RP, Potter HG, Warren RF, Rodeo SA. Acute Gastrocnemius-Soleus Complex Injuries in National Football League Athletes. Orthop J Sports Med 2017;5:2325967116680344. [Crossref] [PubMed]
- Green B, Lin M, Schache AG, McClelland JA, Semciw AI, Rotstein A, Cook J, Pizzari T. Calf muscle strain injuries in elite Australian Football players: A descriptive epidemiological evaluation. Scand J Med Sci Sports 2020;30:174-84. [Crossref] [PubMed]
- Green B, McClelland JA, Semciw AI, Schache AG, McCall A, Pizzari T. The Assessment, Management and Prevention of Calf Muscle Strain Injuries: A Qualitative Study of the Practices and Perspectives of 20 Expert Sports Clinicians. Sports Med Open 2022;8:10. [Crossref] [PubMed]
- Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, Ekstrand J, English B, McNally S, Orchard J, van Dijk CN, Kerkhoffs GM, Schamasch P, Blottner D, Swaerd L, Goedhart E, Ueblacker P. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med 2013;47:342-50. [Crossref] [PubMed]
- Pollock N, James SL, Lee JC, Chakraverty R. British athletics muscle injury classification: a new grading system. Br J Sports Med 2014;48:1347-51. [Crossref] [PubMed]
- Valle X, Alentorn-Geli E, Tol JL, Hamilton B, Garrett WE Jr, Pruna R, Til L, Gutierrez JA, Alomar X, Balius R, Malliaropoulos N, Monllau JC, Whiteley R, Witvrouw E, Samuelsson K, Rodas G. Muscle Injuries in Sports: A New Evidence-Informed and Expert Consensus-Based Classification with Clinical Application. Sports Med 2017;47:1241-53. [Crossref] [PubMed]
- Chow RS, Medri MK, Martin DC, Leekam RN, Agur AM, McKee NH. Sonographic studies of human soleus and gastrocnemius muscle architecture: gender variability. Eur J Appl Physiol 2000;82:236-44. [Crossref] [PubMed]
- Blitz NM, Eliot DJ. Anatomical aspects of the gastrocnemius aponeurosis and its insertion: a cadaveric study. J Foot Ankle Surg 2007;46:101-8. [Crossref] [PubMed]
- Dalmau-Pastor M, Fargues-Polo B Jr, Casanova-Martínez D Jr, Vega J, Golanó P. Anatomy of the triceps surae: a pictorial essay. Foot Ankle Clin 2014;19:603-35. [Crossref] [PubMed]
- Pedret C, Balius R, Blasi M, Dávila F, Aramendi JF, Masci L, de la Fuente J. Ultrasound classification of medial gastrocnemious injuries. Scand J Med Sci Sports 2020;30:2456-65. [Crossref] [PubMed]
- Isern-Kebschull J, Mechó S, Pruna R, Kassarjian A, Valle X, Yanguas X, Alomar X, Martinez J, Pomés J, Rodas G. Sports-related lower limb muscle injuries: pattern recognition approach and MRI review. Insights Imaging 2020;11:108. [Crossref] [PubMed]
- Isern-Kebschull J, Pedret C, Mechó S, Pruna R, Alomar X, Yanguas X, Valle X, Kassarjian A, Martínez J, Tomas X, Rodas G. MRI findings prior to return to play as predictors of reinjury in professional athletes: a novel decision-making tool. Insights Imaging 2022;13:203. [Crossref] [PubMed]
- Isern-Kebschull J, Mechó S, Pedret C, Pruna R, Alomar X, Kassarjian A, Luna A, Martínez J, Tomas X, Rodas G. Muscle Healing in Sports Injuries: MRI Findings and Proposed Classification Based on a Single Institutional Experience and Clinical Observation. Radiographics 2024;44:e230147. [Crossref] [PubMed]
- Sergot L, Kho J, Collins H, Williams J, Murray R, Chakraverty J. MRI classification of calf injuries - a reliability study and correlation with return to play in professional rugby players. Skeletal Radiol 2023;52:61-6. [Crossref] [PubMed]
- Gillies AR, Lieber RL. Structure and function of the skeletal muscle extracellular matrix. Muscle Nerve 2011;44:318-31. [Crossref] [PubMed]
- Brukner P, Cook JL, Purdam CR. Does the intramuscular tendon act like a free tendon? Br J Sports Med 2018;52:1227-8. [Crossref] [PubMed]
- Balius R, Alomar X, Pedret C, Blasi M, Rodas G, Pruna R, Peña-Amaro J, Fernández-Jaén T. Role of the Extracellular Matrix in Muscle Injuries: Histoarchitectural Considerations for Muscle Injuries. Orthop J Sports Med 2018;6:2325967118795863. [Crossref] [PubMed]
- Balius R, Blasi M, Pedret C, Alomar X, Peña-Amaro J, Vega JA, Pruna R, Ardèvol J, Álvarez G, de la Fuente J, Fernández-Jaén T, Järvinen TAH, Rodas G. A Histoarchitectural Approach to Skeletal Muscle Injury: Searching for a Common Nomenclature. Orthop J Sports Med 2020;8:2325967120909090. [PubMed]
- Barça Innovation Hub. Muscle injury guide – preventing and treating muscle injuries in football. Available online: https://barcainnovationhub.com/es/muscle-injury-guide-preventing-and-treating-muscle-injuries-in-football/. Accessed January 14, 2022.
- Balius R, Rodas G, Pedret C, Capdevila L, Alomar X, Bong DA. Soleus muscle injury: sensitivity of ultrasound patterns. Skeletal Radiol 2014;43:805-12. [Crossref] [PubMed]
- Flores DV, Mejía Gómez C, Estrada-Castrillón M, Smitaman E, Pathria MN. MR Imaging of Muscle Trauma: Anatomy, Biomechanics, Pathophysiology, and Imaging Appearance. Radiographics 2018;38:124-48. [Crossref] [PubMed]
- Järvinen TA, Järvinen TL, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. Am J Sports Med 2005;33:745-64. [Crossref] [PubMed]
- Järvinen TA, Järvinen M, Kalimo H. Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J 2013;3:337-45. [Crossref] [PubMed]
- Kalimo H, Rantanen J, Järvinen M. Muscle injuries in sports. Baillieres Clin Orthop 1997;2:1-24.
- Lee JC, Mitchell AW, Healy JC. Imaging of muscle injury in the elite athlete. Br J Radiol 2012;85:1173-85. [Crossref] [PubMed]


