
Dual-channel minimally invasive percutaneous cerclage for femoral shaft and metaphysis fractures during the internal fixation with intramedullary nails: case reports and technical description
Introduction
When using closed reduction intramedullary nail fixation to treat femoral fractures, the placement of the main or locking nail may lead to increased displacement of the split fracture at the metaphysis, thereby affecting the quality of reduction and the effectiveness of internal fixation. The separation and displacement of the butterfly-shaped fracture block in the femoral shaft can prolong the healing time of the fracture and increase the risk of non healing, especially when the separation and displacement of the fracture block is greater than 10 mm (1-3). Small incision reduction and cerclage fixation are significantly affected by soft tissue thickness and are difficult to operate. There have been reports on minimally invasive cerclage of the femur (4-6), but the surgical incisions need to be large enough to accommodate relatively complex specialized tools. The dual channel percutaneous steel wire cerclage surgery introduced in this article does not require special surgical instruments, and the incision can be limited to within 1 cm. The operation is simple, minimally invasive, gentle, and not affected by soft tissue thickness.
Case presentation
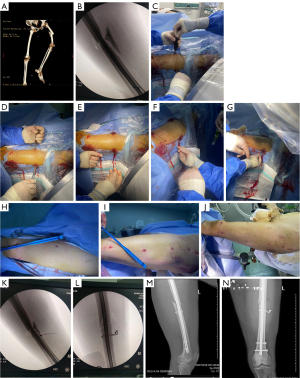
Case 1 (Figure 1): a female, 65-year-old patient. A crushed stone machine injury caused left femoral shaft fracture, combined with pelvic fractures and dislocation of the right hip joint (Figure 1A). After admission, emergency general anesthesia was administered before manual reduction of the right hip joint and percutaneous hollow screw internal fixation of the pubic bone fracture. On the 11th day after injury, closed reduction and antegrade intramedullary nail internal fixation of the femoral fracture were performed. After the intramedullary nail had been successfully implanted and locked during the operation, an X-ray showed significant separation and displacement of the butterfly-shaped fracture block at the fracture site (Figure 1B). Therefore, incisions of 5 and 9 mm were made on the anterior medial and posterior lateral sides of the thigh at the fracture site, respectively, and a hollow screwdriver was used as threading device (Figure 1C,1D). The traction line was inserted through the anteromedial incision with the hollow screwdriver. The ends of the thread were pulled out from the posterior lateral incision around the femur (Figure 1E), and after the thin wire was drawn in with the traction thread (Figure 1F), the thick wire was drawn into the loop-tying channel with the thin wire (Figure 1G). Then, the wire was tightened externally, and the end of the wire was buried deep in the soft tissue. The cerclage operation took 12 minutes and resulted in approximately 5 mL of blood loss. After the above operation, the incision site had a discreet appearance (Figure 1H-1J) and a good reduction effect (Figure 1K-1N).
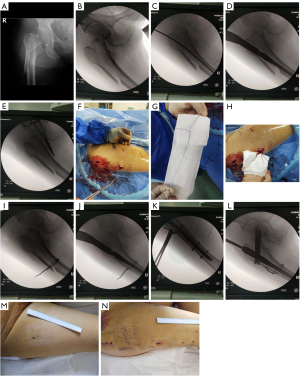
Case 2 (Figure 2): a female, 65-year-old patient. Due to the sequelae of cerebral infarction, the patient had lost coordinated movement of the limbs on one side and subsequently fallen, resulting in a subtrochanteric fracture of the femur with basal femoral neck fracture (Figure 2A). On the third day after injury, she underwent surgery and Intertan intramedullary nail (Dabo Medical Technology Co., LTD., Xiamen, China) fixation was performed. During the surgery, traction reduction was performed, and a slight displacement of the oblique fracture end was observed under fluoroscopy (Figure 2B). A guide needle was inserted, and the medullary cavity was expanded accordingly (Figure 2C). After inserting the main nail along the guide needle, the displacement of the fracture was found to worsen (Figure 2D). After placing the intramedullary nail to a normal depth, the proximal locking nail position was determined and a pre incision of 2.5 cm was made. Then, the intramedullary nail was withdrawn, and the binding site was positioned under fluoroscopy (Figure 2E). A 3 mm incision was made on the anteromedial thigh at the medial margin of the femur, through which an improved threading device (hollow tube: outer diameter 3 mm, inner diameter 1 mm) was punctured, using an elastic thread as the initial traction line. The traction line was led out from the locking nail incision at the proximal end of the intramedullary nail (Figure 2F), and after the traction line had been replaced by a thin steel wire (Figure 2G), the thin steel wire was converted into a thick steel wire (Figure 2H). The steel wire was tightened externally to reduce the fracture end (Figure 2I,2J), then the main intramedullary nail was inserted again and locked after the femoral medullary cavity had been re-surfaced with medullary cavity drills. After the surgery, the anatomical reduction of the fracture was observed through fluoroscopy (Figure 2K,2L), and a minimally invasive appearance was achieved (Figure 2M,2N). The cerclage operation took 10 minutes and resulted in approximately 5 mL of blood loss.
Technical approach of percutaneous cerclage
Instrument preparation (Figure 3): threading device (hollow screwdriver or hollow tube), wire of different diameters, vascular forceps (Figure 3A), elastic traction line (Figure 3B).

Operation process (Figure 4): fluoroscopy is used to locate the binding site. An incision is made on the anteromedial thigh level at the medial margin of the femur, and another incision is made on the posterior lateral sides of the thigh at the fracture site, with lengths of about 3–5 and 9 mm, respectively. The elastic traction line is inserted into the threading device, and the threading device is used to puncture to the front side of the femur through the anteromedial incision, and then slid along the medial bone surface to the back. The tip of the vascular clamp is slid back along the bone surface after puncturing through posterior lateral incision, and the position of the fracture block is identified through touching by the tip of the vascular clamp (Figure 4A). Then, the fascia attached to the thick line of the femur is penetrated after the tip of the forceps encircles the fracture block. Both hands hold the threading device and vascular clamp respectively to make contact with each other in the medial posterior section of the femur, ensuring that the threading device is located within the clamping range of the tip of the vascular clamp (Figure 4B). At this time, the assistant pushes the elastic traction line inward to ensure that it does not retract. The operator retracts the threading device to the side of the vascular clamp, clamps the vascular clamp, and extracts the elastic traction line to the outside of the skin (Figure 4C). Then, the vascular clamp is inserted from the original soft tissue channel to the lateral side of the femur, and cuts along the bone surface to the anterior side of the femur. At the same time, the threading device tip is slid from the medial to the anterior side of the femur. When the vascular forceps come into contact with the threading device, the elastic traction line at the outlet of the threading device is clamped with the vascular forceps and removed to the outside of the skin (Figure 4D). Through the above operation, the two ends of the elastic traction line encircle the femur 360° and lead out from the posterior lateral incision. One end of the elastic traction line is connected to the thin steel wire (fold in half) (Figure 4E), and the elastic traction line is removed to achieve the conversion between the elastic traction line and the thin steel wire. Then, according to the needs of the fixation strength, the thin steel wire is converted to thick steel wire (Figure 4F), and the steel wire is finally tightened outside the skin for fracture reduction and fixation (Figure 4G). After completing the surgery, the external steel wire is cut, and the tail end twisted, with a clamp, then it is pushed deep away from the deep fascia (Figure 4H).

This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by Ethics Committee of Zibo Municipal Hospital, Shandong Province (No. 20240729), and all participants provided written informed consent.
Discussion
When intramedullary nail fixation is used for femoral fractures, the mismatch between the diameter of the medullary cavity and the intramedullary nail can affect the reduction effect, especially in cases of split or oblique fractures of the metaphysis, which can increase the difficulty of reduction. Research has found that the incidence of malunion after intramedullary nail fixation for epiphyseal fractures can reach up to 29% (7). The presence of free bone fragments in the femoral shaft increases the risk of nonunion of fractures, with a reported incidence rate of up to 12.5–34% in the literature (1,7). The human thigh muscles are rich in vasculature, and after a femoral fracture, there is blood accumulation and muscle edema in the soft tissue. Severe thigh swelling leads to a deeper fracture site, especially in obese patients. Therefore, when implementing intramedullary nail fixation, it is difficult to handle the misalignment of the fracture end or the displacement of the butterfly bone block. The cerclage technique has been shown to play an important role in improving the quality of fracture reduction and fixation strength, and shortening healing time in intramedullary nail fixation of subtrochanteric fractures of the femur (8-10). The cerclage technique utilizes the adaptive principle of fractures to make it easier to reduce, and the binding fixation of the fracture block on the side where the diameter of the medullary cavity and intramedullary nail do not match can not only reduce the fracture block, but also increase the stability of the fracture end relative to the intramedullary nail. The core of minimally invasive technology in this study lies in the placement of a traction line through two channels, followed by the conversion of the traction line and steel wires, making the threading process easier and closer to the bone surface. The conversion between thin and thick steel wires can meet the needs of different fixation strengths. The surgical incision is mainly used to meet the shuttle of the elastic traction line. The threading instrument is simple, and the operation is not affected by soft tissue thickness. Compared to a single incision with titanium cable or steel wire ligation, the operation is more minimally invasive and gentle. Therefore, in addition to being used for reduction and fixation of oblique fractures of the epiphyseal end, it is more advantageous to handle relatively small butterfly-shaped bone blocks.
During intramedullary nail fixation for femoral shaft and metaphysis fractures, nailing is used to align and enable early mobilization and weight bearing. Combined percutaneous binding techniques can increase fracture stability at minimal cost, reduce the risk of fracture nonunion due to fracture instability, and shorten fracture shaping time. The drawback of this study is the lack of a large number of clinical case-control studies.
Conclusions
Dual channel percutaneous steel wire cerclage is a simple, minimally invasive, and practical surgical technique that can be used for minimally invasive reduction and fixation of oblique femoral metaphysis fractures and butterfly-shaped femoral shaft fracture blocks during the internal fixation with intramedullary nails.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-724/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by Ethics Committee of Zibo Municipal Hospital, Shandong Province (No. 20240729), and all participants provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lee JR, Kim HJ, Lee KB. Effects of third fragment size and displacement on non-union of femoral shaft fractures after locking for intramedullary nailing. Orthop Traumatol Surg Res 2016;102:175-81. [Crossref] [PubMed]
- Lin SJ, Chen CL, Peng KT, Hsu WH. Effect of fragmentary displacement and morphology in the treatment of comminuted femoral shaft fractures with an intramedullary nail. Injury 2014;45:752-6. [Crossref] [PubMed]
- Vicenti G, Carrozzo M, Caiaffa V, Abate A, Solarino G, Bizzoca D, Maddalena R, Colasuonno G, Nappi V, Rifino F, Moretti B. The impact of the third fragment features on the healing of femoral shaft fractures managed with intramedullary nailing: a radiological study. Int Orthop 2019;43:193-200. [Crossref] [PubMed]
- Trikha V, Das S, Agrawal P. M A, Kumar Dhaka S. Role of percutaneous cerclage wire in the management of subtrochanteric fractures treated with intramedullary nails. Chin J Traumatol 2018;21:42-9. [Crossref] [PubMed]
- Shin WC, Moon NH, Jang JH, Jeong JY, Suh KT. Technical note and surgical outcomes of percutaneous cable fixation in subtrochanteric fracture: A review of 51 consecutive cases over 4 years in two institutions. Injury 2019;50:409-14. [Crossref] [PubMed]
- Kang SJ, Bao FL, Huang DS, Jiang T, Hu YM, Li JM, Liu T. Percutaneous Cerclage Wiring Combined with Cephalomedullary Nailing for Irreducible Subtrochanteric Fractures. Orthop Surg 2021;13:1899-911. [Crossref] [PubMed]
- Santolini E, West RM, Giannoudis PV. Leeds-Genoa Non-Union Index: a clinical tool for asessing the need for early intervention after long bone fracture fixation. Int Orthop 2020;44:161-72. [Crossref] [PubMed]
- Hantouly AT, Salameh M, Toubasi AA, Salman LA, Alzobi O, Ahmed AF, Ahmed G. The role of cerclage wiring in the management of subtrochanteric and reverse oblique intertrochanteric fractures: a meta-analysis of comparative studies. Eur J Orthop Surg Traumatol 2023;33:739-49. [Crossref] [PubMed]
- Panteli M, Vun JSH, West RM, Howard AJ, Pountos I, Giannoudis PV. Management of subtrochanteric femur fractures: is open reduction associated with poor outcomes? Eur J Trauma Emerg Surg 2022;48:1759-68. [Crossref] [PubMed]
- Kim CH, Yoon YC, Kang KT. The effect of cerclage wiring with intramedullary nail surgery in proximal femoral fracture: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 2022;48:4761-74. [Crossref] [PubMed]


