
Recurrent mitral regurgitation after repair of Barlow’s disease in a single-center retrospective cohort study
Introduction
Barlow’s disease (BD) is one of the more frequent etiologies of degenerative mitral valve (MV) disease, which frequently results in substantial mitral regurgitation (MR) (1). BD caused by excessive myxomatous tissue development with or without calcification is characterized by severe annular dilatation, bileaflet prolapse, and the presence of thick, spongy leaflets (2). The pathology of BD is a challenge for surgeons performing MV repair (MVR), as is the achievement of a durable surgical result in this cohort of patients.
A previous study reported that the linearized recurrence rate of greater than 2+ after surgical repair in patients with degenerative valve disease was 3.7% per year (3). Additionally, the recurrence rate was higher in patients with BD, which was 6.0% per year (4). Similar conclusions have been reached by other authors (5). However, the risk of recurrent MR has not been widely reported because most studies have focused on survival and the risk of reoperation. Of note, the recurrence of regurgitation could only be partially explained by inadequate surgical techniques. Therefore, the aim of this study was to evaluate the outcome, persistence, and survival of MVR in BD and to identify factors influencing recurrent regurgitation. We present this article in accordance with the STROCSS reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1768/rc).
Methods
Study design
Consecutive patients who underwent MVR at a tertiary hospital (Guangdong Provincial People’s Hospital, Guangzhou, China) between 1 January 2010 and 1 June 2022 were retrospectively studied. The study was approved by the Institutional Review Board at Guangdong Provincial People’s Hospital (No. KY-Q-2021-271-02; 2022.1.29 approval) and conformed to the Declaration of Helsinki (as revised in 2013). The requirement for obtaining informed consent was exempted due to the retrospective nature of the study with minimal risk. The research was retrospectively registered.
Patient population
Between 1 January 2010 1 and June 2022, a total of 282 consecutive patients with BD underwent MVR at our clinic. However, eight patients with unsuccessful MVR procedures were excluded [one patient was found to have MR >2+ on saline testing and seven patients were found to have MR >2+ on transesophageal echocardiography (TEE), one of whom had systolic anterior motion (SAM); all the eight patients were referred for MV replacement surgery] (Figure 1), and 274 patients were studied. To analyze the results of MVR and to identify the risk factors affecting MR recurrence, we defined two groups: a total of 240 patients had MR grade <2+ (group A), whereas 34 patients experienced recurrent MR after MVR (group B; the patients who had MR ≥2+). Baseline clinical and echocardiographic characteristics (at the time of preoperative evaluation) of these patients were compared between the two groups (Table 1).
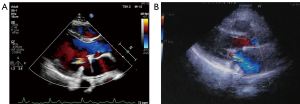
Table 1
| Variables | Total cohort (n=274) | Group A (n=240) | Group B (n=34) | P value |
|---|---|---|---|---|
| Age (years) | 46.00 [16–75] | 43.00 [16–75] | 51.50 [18–71] | 0.180 |
| Male | 186 (67.9) | 159 (66.3) | 27 (79.4) | 0.124 |
| BMI (kg/m2) | 22.13±3.54 | 22.07±3.46 | 22.53±4.15 | 0.475 |
| NYHA class (III/IV) | 58 (21.2) | 51 (21.3) | 7 (20.6) | 0.443 |
| Comorbid disease | ||||
| Hypertension | 47 (17.2) | 42 (17.5) | 5 (14.7) | 0.686 |
| Diabetes | 9 (3.3) | 8 (3.3) | 1 (2.9) | >0.999 |
| Coronary artery disease | 9 (3.3) | 7 (2.9) | 2 (5.9) | 0.364 |
| AF | 45 (16.4) | 37 (15.4) | 8 (23.5) | 0.232 |
| Stroke | 6 (2.2) | 5 (2.1) | 1 (2.9) | 0.552 |
| Chronic kidney disease | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| Endocarditis | 13 (4.7) | 9 (3.8) | 4 (11.8) | 0.063 |
| Preoperative MV assessment (echocardiogram) | ||||
| Preoperative MR grade (3+/4+) | 269 (98.2) | 237 (98.8) | 32 (94.1) | 0.817 |
| Preoperative TR grade (3+/4+) | 31 (11.3) | 28 (11.7) | 3 (8.8) | 0.654 |
| LAD (mm) | 45.01±9.08 | 44.08±8.48 | 51.62±10.49 | <0.001 |
| LVEDD (mm) | 57.06±7.13 | 56.56±6.46 | 60.59±10.19 | 0.031 |
| LVESD (mm) | 34.18±5.88 | 33.65±5.42 | 37.91±7.56 | 0.003 |
| LVESD ≥40 mm | 35±12.8 | 26±10.8 | 9±26.5 | 0.023 |
| RAD (mm) | 48.36±8.61 | 48.43±8.68 | 47.85±8.17 | 0.714 |
| RVD (mm) | 53.57±6.42 | 53.55±6.54 | 53.74±5.58 | 0.873 |
| LVEF (%) | 66.72±6.02 | 66.90±6.00 | 65.44±6.40 | 0.188 |
| Intraoperative MV assessment (surgery view) | ||||
| Prolapsing segments | 3.00 [0–8] | 3.00 [0–8] | 3.00 [1–8] | 0.862 |
| Anterior | 57 (20.8) | 47 (19.6) | 10 (29.4) | 0.186 |
| Posterior | 99 (36.1) | 87 (36.3) | 12 (35.3) | 0.914 |
| Anterior and posterior | 122 (44.5) | 109 (45.4) | 13 (38.2) | 0.430 |
| Perforation or fissure | 21 (7.7) | 17 (7.1) | 4 (11.8) | 0.309 |
| Rupture of the chordal | 125 (45.6) | 109 (45.4) | 16 (47.1) | 0.857 |
Data are presented as the median [range], mean ± SD, or n (%). Group A: defined as patients who had MR grade <2+; group B: defined as patients who had recurrent MR after MVR, that is, patients with MR grade ≥2+. BMI, body mass index; NYHA, New York Heart Association; AF, atrial fibrillation; MV, mitral valve; MR, mitral regurgitation; MVR, mitral valve repair; TR, tricuspid regurgitation; LAD, left atrium dimension; LVEDD, left ventricular end-diastolic dimension; LVESD, left ventricular end-systolic dimension; RAD, right atrium dimension; RVD, right ventricular dimension; LVEF, left ventricular ejection fraction; SD, standard deviation.
MVR patients who underwent concomitant tricuspid valve repair (TVR), maze/pulmonary vein isolation (PVI), left atrial appendage (LAA) closure, or atrial septal defect (ASD) repair were also included in this study. Patients ≤14 years of age, those with cardiomyopathy, cardiac tumors, previous cardiac surgery, concomitant aortic surgery, concomitant coronary artery bypass grafting (CABG), and redo surgery for a failed MVR were excluded (Figure 2).

Smokers were required to quit smoking for 1 month before surgery, diabetics were required to control their blood sugar, and all patients underwent coronary computed tomography (CT) or coronary angiography and fecal occult blood testing to reduce the risk of surgery.
MV characteristics
The degenerative MV was classified as BD based on echocardiographic and intraoperative visual findings (6).
Surgical techniques
All patients underwent intraoperative echocardiography before and after repair. Standard cannulation techniques using central or peripheral cannulation (depending on the surgical approach used) and intermittent cold blood cardioplegia to protect the heart were used in all cases. MVR was performed via a median sternotomy (MS) in 55.1% of patients and via a totally endoscopic minimally invasive (TEMI) approach in 44.9% of patients. Surgery performed by different surgeons in the same center; each cardiac surgeon had >15 years of experience and conducted >50 MVR procedures per year.
All of the patients were operated on using standard repair techniques. Due to the extensive mitral lesions in patients with BD, a combination of repair techniques is often required. Due to their complex pathology, these valves are technically more challenging. The aims of reconstructive surgery are to preserve or restore normal leaflet motion, create a large coaptation surface, and stabilize the entire annulus with a remodeling annuloplasty (7). It is well known that reconstruction can be achieved by resection of the prolapsing segments, commissuroplasty, implantation of neochordae, or annuloplasty. In this study, posterior leaflet (PL) prolapse was preferably corrected by resection if the prolapsing segment had extensive overgrowth. The prolapse of the anterior leaflet (AL) was corrected by transfer of the chordae or implantation of an artificial chordae. If there was no dilatation or only a slight dilatation of the annulus, the prolapse was preferably corrected by artificial chordae. In the majority of instances, mitral ring annuloplasty was performed to complete the repair, with the exception of extreme circumstances, such as where the AL was too large and SAM may be anticipated following ring annuloplasty, or when the annulus was not or just slightly dilated. For the selection of the ring size, the intertrigonal distance and the AL height were measured. The ring was chosen according to the surgeon’s discretion. The competence of the valve after the repair was assessed by the saline test and then by TEE after the atrium had been closed. If the residual MR was more than mild, a second pump run was performed for repair.
For each patient, the specific surgical repair techniques used at the end of surgery were identified and coded: leaflet intervention (none, resection, cleft closure), annulus intervention (none, sliding repair), neochordae implantation (yes or no), and annuloplasty ring placement (yes or no).
Table 2 shows the operative details. The most common repair techniques were artificial chordae implantation and mitral annuloplasty. Edge-to-edge repair was performed as the primary repair strategy in 3.3% of patients. Cleft closure/plication (17.9%) and resection (15.7%) were rarely used. The AL procedure was performed in 20.8%, the PL procedure in 36.1%, and the bileaflet procedure in 44.5%.
Table 2
| Variables | Total cohort (n=274) | Group A (n=240) | Group B (n=34) | P value |
|---|---|---|---|---|
| Approach | 0.116 | |||
| MS | 151 (55.1) | 128 (53.3) | 23 (67.6) | |
| TEMI | 123 (44.9) | 112 (46.7) | 11 (32.4) | |
| Concurrent procedure | ||||
| TVR | 71 (25.9) | 59 (24.6) | 12 (35.3) | 0.182 |
| Maze/PVI | 12 (4.4) | 11 (4.6) | 1 (2.9) | >0.999 |
| ASD repair | 3 (1.1) | 1 (0.4) | 1 (2.9) | 0.233 |
| LAA closure | 28 (10.2) | 24 (10.0) | 4 (11.8) | 0.762 |
| Repair techniques | ||||
| Resection and suture | 43 (15.7) | 36 (15.0) | 7 (20.6) | 0.402 |
| Sliding | 3 (1.1) | 2 (0.8) | 1 (2.9) | 0.329 |
| Neochordal replacement | 231 (84.3) | 202 (84.2) | 29 (85.3) | 0.866 |
| Number of cord tendons implanted | 3.16±2.79 | 3.31±2.37 | 3.53±2.48 | 0.613 |
| Mitral annuloplasty ring | 272 (99.3) | 238 (99.2) | 34 (100.0) | >0.999 |
| Mitral annuloplasty ring type | 0.748 | |||
| Physio | 246 (89.8) | 215 (89.6) | 31 (91.2) | |
| Physio II | 13 (4.7) | 12 (5.0) | 1 (2.9) | |
| Medtronic | 3 (1.1) | 3 (1.3) | 0 (0.0) | |
| Balance medical | 10 (3.6) | 8 (3.3) | 2 (5.9) | |
| Size of mitral annuloplasty (mm) | 32.41±4.64 | 32.41±4.80 | 32.48±3.27 | 0.976 |
| Big size of mitral annuloplasty | n=272 | n=239 | n=33 | 0.039 |
| Big size ≥34 | 111 (40.8) | 103 (43.1) | 8 (24.2) | |
| Small size <34 | 161 (59.2) | 136 (56.9) | 25 (73.5) | |
| Commissuroplasty | 49 (17.9) | 44 (18.3) | 5 (14.7) | 0.605 |
| Edge-to-edge | 9 (3.3) | 8 (3.3) | 1 (2.9) | >0.999 |
| Intraoperative MR area (cm2) | 0.37±0.59 | 0.34±0.59 | 0.56±0.58 | 0.045 |
| CPB time (min) | 147.43±40.20 | 148.92±41.22 | 136.26±30.25 | 0.035 |
| ACC time (min) | 98.24±32.68 | 99.48±33.40 | 89.50±25.81 | 0.048 |
| Total operation time (min) | 240.47±57.61 | 240.75±59.22 | 238.50±45.28 | 0.832 |
| ICU time (hours) | 49.26±78.26 | 48.97±80.94 | 51.29±56.71 | 0.871 |
| MVT (hours) | 18.15±40.07 | 17.27±37.54 | 24.35±55.03 | 0.335 |
| LOS (days) | 9.10±7.52 | 8.95±7.42 | 10.15±8.25 | 0.386 |
| Postoperative MV assessment (echocardiogram 1 week after surgery) | ||||
| MR grade (3+/4+) | 9 (3.3) | 2 (0.8) | 7 (20.6) | <0.001 |
| LAD (mm) | 36.02±7.04 | 35.56±6.85 | 39.21±7.60 | 0.005 |
| LVEDD (mm) | 47.43±7.08 | 46.79±6.43 | 52.65±9.77 | <0.001 |
| LVESD (mm) | 31.77±6.81 | 31.11±6.20 | 36.38±8.94 | <0.001 |
| LVEF (%) | 59.40±7.66 | 59.79±7.79 | 55.71±9.23 | 0.006 |
Data are presented as the mean ± SD or n (%). Group A: defined as patients who had MR grade <2+; group B: defined as patients who had recurrent MR after MVR, that is, patients with MR grade ≥2+. MS, median sternotomy; TEMI, total endoscopic minimally invasive; TVR, tricuspid valve repair; PVI, pulmonary vein isolation; ASD, atrial septal defect; LAA, left atrial appendage; MR, mitral regurgitation; MVR, mitral valve repair; CPB, cardiopulmonary bypass; ACC, aortic cross-clamp; ICU, intensive care unit; MVT, mechanical ventilation time; LOS, length of hospital stay; MV, mitral valve; LAD, left atrium dimension; LVEDD, left ventricular end-diastolic dimension; LVESD, left ventricular end-systolic dimension; LVEF, left ventricular ejection fraction; SD, standard deviation.
Nearly all of the patients (99.3%) received annuloplasties. The Carpentier-Edwards (CE) Physio ring (Physio) (Edwards Lifesciences Corp., Irvine, CA, USA) was used in 246 (89.8%) patients, whereas 13 (4.7%) patients received the CE Physio II ring.
Concomitant tricuspid surgery was performed in 71 patients (25.9%), LAA closure was performed in 28 patients (10.2%), and the A maze procedure or PVI was performed in 12 patients (4.4%). The mean time for cardiopulmonary bypass (CPB) was 147.43 minutes, and the mean time for aortic cross-clamp (ACC) was 98.24 minutes.
Follow-up
The follow-up was performed until March 2023. During a median follow-up time of 3.28 years, patients were followed up by means of clinic visits, phone calls, mailed or electronic questionnaires. Clinical and echocardiographic follow-up were performed by the referring cardiologist. Survival, reoperation, cerebrovascular events, bleeding complications, anticoagulation therapy, New York Heart Association (NYHA) functional class, and heart rhythm were recorded.
End points and echocardiographic measures
The primary outcome was recurrent MR which was determined on postoperative transthoracic echocardiography (TTE). The secondary outcomes were death and MV reoperation after surgery. Recurrence was measured by TTE and verified by the Echo Core laboratory. Recurrent MR was defined as MR grade ≥2+. The severity of MR was classified using Grades (grade 0, 1+, 2+, 3+, 4+) (8). To be classified as having no recurrent MR, patients with some missing echocardiographic data had to have MR <2+ on at least two recent echocardiograms. If the patient had recurrent MR, the TTE result was based on the information from the time that the MR ≥2+ first occurred; the recurrence time was the date that the MR ≥2+ was first identified, and the reoperation time was the date that the reoperation was performed. In addition, factors affecting MR recurrence were analyzed by dividing patients into a group undergoing MVR via MS and MVR via TEMI. Pre, intra, and postoperative echocardiographic data were collected.
Statistical analysis
Categorical variables are presented as frequencies with percentages and were compared between groups using Fisher’s exact test. Continuous variables are presented as the means with standard deviation (SD) and were compared between groups using analysis of variance. The Shapiro-Wilk test was utilized for the normality test. Cox proportional hazards methods were used to analyze the data on the recurrence of MR over time. The Kaplan-Meier method was used to analyze time-to-event data on survival, recurrent MR, and MV reoperation, and the log-rank and Wilcoxon test were used for group comparisons. Estimates are presented with 95% confidence intervals (CIs). Statistical significance was indicated by two-sided P values <0.05. Missing data were filled in using the mean value. As the rate of loss to follow-up in this study was less than 5%, data for loss to follow-up were corrected by processing using the last observation carried forward (LOCF) method. All statistical analyses were performed using R version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria) and SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
Results
Immediate surgical result of MVR
The most common preoperative comorbidities were hypertension (17.2%) and atrial fibrillation (AF) (16.4%), and 21.2% were in advanced NYHA functional class (III or IV). The immediate postoperative echocardiographic results were excellent: 270 patients (98.5%) had no or MR =1+. The in-hospital mortality rate was 0.4%, which was due to death from sepsis with multiple organ failure. The success of the operation was assessed by an echocardiographic examination of the function of the MV within the first postoperative week. MR was absent or trivial in 95.4% of all patients at 1 week postoperatively. No cases of endocarditis were documented.
The most common postoperative complications were lung infection in 18 (6.6%), reoperation for bleeding in 11 (4.0%), arrhythmia in 4 (1.5%), gastrointestinal bleeding in 3 (1.1%), renal dysfunction in 3 (1.1%), and stroke in 3 (1.1%) patients (Table 3). The mean intensive care unit (ICU) stay was 49.26 hours. The mean length of hospital stay (LOS) was 9.10 days (Table 2).
Table 3
| Variables | Total cohort (n=274) | Group A (n=240) | Group B (n=34) | P value |
|---|---|---|---|---|
| Perioperative complications, n (%) | ||||
| Death | 1 (0.4) | 1 (0.4) | 0 (0.0) | >0.999 |
| Reoperation for bleeding | 11 (4.0) | 10 (4.2) | 1 (2.9) | >0.999 |
| Arrhythmia | 4 (1.5) | 4 (1.7) | 0 (0.0) | >0.999 |
| Gastrointestinal bleeding | 3 (1.1) | 2 (0.8) | 1 (2.9) | 0.329 |
| Renal dysfunction | 3 (1.1) | 3 (1.3) | 0 (0.0) | 0.182 |
| Stroke | 3 (1.1) | 2 (0.8) | 1 (2.9) | 0.329 |
| Lung infection | 18 (6.6) | 17 (7.1) | 1 (2.9) | 0.709 |
| Low cardiac output | 7 (2.6) | 6 (2.5) | 1 (2.9) | >0.999 |
| Long-term complications, n (%) | ||||
| Radiofrequency ablation | 7 (2.6) | 6 (2.5) | 1 (2.9) | >0.999 |
| Pacemaker implantation | 1 (0.4) | 1 (0.4) | 0 (0.0) | >0.999 |
| Stroke | 3 (1.1) | 1 (0.4) | 2 (5.9) | 0.041 |
| Recurrent MR | 34 (12.4) | |||
| MV reoperation | 4 (1.5) | |||
| Death | 3 (1.1) |
Group A: defined as patients who had MR grade <2+; group B: defined as patients who had recurrent MR after MVR, that is, patients with MR grade ≥2+. MR, mitral regurgitation; MVR, mitral valve repair; MV, mitral valve.
Survival and recurrent rate
During a median follow-up time of 3.28 years (range, 0–12.39 years). A total of eight patients were lost to clinical follow-up, mainly due to the fact that these eight patients did not return to our center after surgery and neither the patients nor their families could be contacted through contact telephone numbers and addresses. Over time, a total of three patients died, all of whom were in the A group. There was one case of death due to cardiogenic causes. There was no difference in survival between patients without MR recurrence and those who had MR recurrence (P=0.5) (Figure 3). Overall survival rates were 99.3%±0.5% at 1 year, 98.6%±0.8% at 5 years, and 98.6%±0.8% at 12 years. During the follow-up period, 34 patients had moderate or higher MR. Some 87.6% of valves were functional (MR <2+) at the end of follow-up on 1 March 2023 (up to 12 years). The cumulative incidence rate of MR ≥2+ at 12 years was 12.4%. According to the classical Kaplan-Meier approach, freedom from recurrent MR (regurgitation <2+) was 97.4%±1.0% at 1 month, 94.1%±1.4% at 1 year, 85.3%±2.6% at 5 years, and 72.0%±8.2% at 10 years (this analysis did not account for death as a competing outcome, death counted as a censor). When we considered competing risks due to mortality, the cumulative incidence of MR progression of 2+ or more grades was 2.6%, 5.9%, 14.5%, and 27.7% at 1 month, 1 year, 5 years, and 10 years, respectively. Of note is the slightly higher rate of recurrent MR after the first 6 months postoperatively, with a cumulative incidence of MR ≥2+ at 6 months of 5.5%. During the follow-up period, 4 patients (1.5%) underwent MV reoperation. The freedom from reoperation was 100% at 1 year, 98.9%±0.8% at 5 years, 89.1%±6.6% at 10 years, and 89.1%±6.6% at 12 years for all patients. Figure 3 illustrates the main findings of the study.

Clinical outcome and morbidity
A total of seven patients who underwent radiofrequency ablation had a recurrence of AF, and one other received a pacemaker implantation during the follow-up period. There were three cases of stroke (Table 3).
Predictive factors of recurrent MR after MVR
To analyze the results of MVR and to identify the risk factors affecting MR recurrence, we defined two groups: no MR recurrence (group A, n=240) and MR recurrence (group B, n=34). Patients with recurrent MR had a larger left atrium dimension (LAD) (P<0.001) and left ventricular end-diastolic dimension (LVEDD) (P=0.031) on preoperative echocardiography. In addition, a larger left ventricular end-systolic dimension (LVESD) (P=0.003) and a higher proportion of LVESD ≥40 mm (P=0.023) were found in patients with MR recurrence. In patients with MR recurrence, the number of prolapsing MV segments was not significantly higher than that in the group without MR recurrence. Furthermore, the proportions of posterior and anterior MV leaflets were not significantly larger in patients with MR recurrence than in patients without MR recurrence. In addition to these findings, 125 patients (45.6%) had ruptured chordae tendineae, 21 patients (7.7%) had one or more clefts, and 13 patients (4.7%) had endocarditis. There was no significant difference between the two groups (Table 1).
Of note, specific surgical repair techniques had no significant predictive value for recurrent regurgitation: the use of sliding annuloplasty (P=0.329), resection (P=0.402), annuloplasty ring (P>0.999), and chordal replacement (P=0.866) were generally not associated with outcome. Almost all patients received an annuloplasty ring (n=272, 99.3%). However, the distribution of annuloplasty ring size and type was not significantly different between the two groups (Table 2).
Multivariable time-dependent Cox proportional hazards analysis (Table 4) revealed that the subpopulation with regurgitation recurrence was mainly characterized by a higher grade of 1 week postoperative MR {hazard ratio (HR) = Exp[4.500 − 0.544 × ln(t + 20)]; P=0.008}. The intraoperative MR area [HR =1.723; 95% confidence interval (CI): 1.051–2.824; P=0.031] and postoperative LVEDD (HR =1.149; 95% CI: 1.016–1.300; P=0.027) showed a trend towards higher recurrence of regurgitation. Additionally, postoperative left ventricular ejection fraction (LVEF) also predicted regurgitation recurrence, with a protective effect (HR =0.931; 95% CI: 0.868–0.999; P=0.049).
Table 4
| Variables | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Preoperative LAD | 1.071 (1.041–1.101) | <0.001 | – | – | |
| Preoperative LVEDD | 1.061 (1.024–1.099) | 0.031 | – | – | |
| Preoperative LVESD | 0.003 | ||||
| Preoperative LVESD ≥40 mm | 2.842 (1.325–6.097) | 0.023 | – | – | |
| Postoperative LVEF | 0.911 (0.831–0.098) | 0.046 | 0.931 (0.868–0.999) | 0.049 | |
| Postoperative LAD | 1.073 (1.028–1.120) | 0.001 | – | – | |
| Postoperative LVEDD | 1.089 (1.053–1.126) | <0.001 | 1.149 (1.016–1.300) | 0.027 | |
| Postoperative LVESD | 1.093 (1.052–1.135) | <0.001 | – | – | |
| Intraoperative MR area | 1.383 (0.968–1.976) | 0.047 | 1.723 (1.051–2.824) | 0.031 | |
| Degree of postoperative MR | 4.810 (2.712–8.530) | <0.001 | Exp[4.500 − 0.544 × ln(t + 20)] | 0.008 | |
MR, mitral regurgitation; HR, hazard ratio; CI, confidence interval; LAD, left atrium dimension; LVEDD, left ventricular end-diastolic dimension; LVESD, left ventricular end-systolic dimension; LVEF, left ventricular ejection fraction.
When the patient population was divided into those who underwent MVR via MS and those who underwent MVR via TEMI, the risk factors became more focused (Table 5). In the MS approach, the grade of postoperative MR was predictive of the recurrence of regurgitation (P=0.023) as well as the LVEF of the postoperative period (P=0.046). In patients treated via the TEMI approach, the concomitance of ASD repair (P=0.049) was the main predictor of regurgitation.
Table 5
| Variables | MS | TEMI | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Postoperative LVEF | 0.911 (0.831–0.999) | 0.046 | – | – | |
| Degree of postoperative MR | Exp[321.40 − 0.515 × ln(t + 20)] | 0.023 | – | – | |
| Concurrent ASD repair | – | – | 13.780 (1.014–187.336) | 0.049 | |
MR, mitral regurgitation; MS, median sternotomy; TEMI, total endoscopic minimally invasive; HR, hazard ratio; CI, confidence interval; LVEF, left ventricular ejection fraction; ASD, atrial septal defect.
Discussion
There is still an ongoing debate about the durability of MVR for patients with BD. Valve repair in BD is particularly challenging due to its complex pathology. Multisegmental involvement with excess leaflet tissue results in a lack of a reference point, complicating valve analysis and repair planning. Our study demonstrated that in a single institution, real-world population with BD, a high rate of successful reconstruction with low morbidities and mortalities, excellent long-term survival, and low reoperation rates could be achieved. Our high successful repair rate of 95.7% in a cohort with complex valve pathology compared favorably with other studies that report repair rates of 90–100% depending on the valve pathology (9-11). Repair rate in prior studies was reported as 99% and 100% by Faerber et al. (12) and Tomšic et al. (13), respectively. Faerber et al. analyzed the post-operative results of symmetrical and asymmetrical lesions according to repair technique in 103 patients with BD (12). In our study, we enrolled all BD patients who underwent MVR, without bias towards the surgical technique to be more in line with clinical reality, and analyzed the associated risk factors affecting postoperative survival, reoperation, and recurrent regurgitation. We found an excellent clinical outcome with a low reoperation rate (89.1% freedom) at 10 years. Nevertheless, the rate of freedom from failed repair (regurgitation <2+) was 72.0% at 10 years. Meanwhile, the present article confirmed previous findings that the recurrence of MR based on echocardiographic studies was more frequent than the reoperation rate indicates. Reoperation rate was therefore shown not to be the best parameter to estimate the efficacy and durability of MVR.
MV pathology
As mentioned earlier, our immediate postoperative echocardiographic results were excellent: 98.5% of the patients had no or MR =1+. However, despite such a highly successful repair, recurrence of MV incompetence still occurred at a constant rate during the following years. The causes of the recurrence of regurgitation after MVR can be classified as either procedure-related or valve-related. There is a reported difference in outcome within the MV patient population, depending on valve pathology: the literature shows excellent long-term outcomes for PL patients and less good outcomes for AL and bileaflet. In a larger study, they showed that patients with an isolated AL prolapse had an increased early risk of reoperation (14). However, in our study, we did not find any differences between the prolapsed segments; therefore, we are convinced that either AL or PL prolapse were not significantly associated with the recurrence of regurgitation, as already shown by Passos et al. (15) and De Bonis et al. (16).
Surgical repair techniques
A wide variety of surgical repair techniques have been described in the 40 years since MVR for MR was successfully performed (17). Many different MVR techniques were used in the present study. It is known from previous literature that the implantation of artificial chordae (18) and the use of ring annuloplasty (19) reduced the risk of recurrent MR in the late hazard phase. Pfannmueller et al. reported more MR at discharge in the resection group than in the chordae group (20). The artificial chordae technique is associated with excellent results and may therefore be more durable (9). Kasegawa et al. showed that the number of artificial chordal replacements was associated with a reduced risk of recurrent moderate MR (21). Of note, in the present study, the neochordae group did not have such superior outcomes. There were no significant differences between the resection group and the neochordae group, and the number of chordae implanted was not associated with the reduced recurrence of MR. This study suggests that neochordae and resection techniques are equally safe and effective.
Recently, several groups have reported excellent clinical results with simple ring-only repair in patients with BD (12). Lawrie et al. found that leaflet repair was not needed in 17% of patients with BD (22). In previous studies, Hiemstra et al. and van Wijngaarden et al. reported that annular abnormalities of the MV were already present prior to the development of significant MR (23,24). Ben Zekry et al. reported excellent mid-term clinical results of ring-only repair in patients with BD, with no recurrence of MR during a mean follow-up period of 38±36 months (25). In addition, Adams et al. mentioned that the use of large annuloplasty rings has recently been advocated with regard to the risk of SAM (26). The present study showed that the size and type of annuloplasty rings had no relevance to the risk of recurrence of regurgitation and did not involve any patients with SAM. Although Physio II is considered an improvement over Physio, it has an improved shape, a double saddle, and a cuff to reduce tension on the sutures. However, better annular dynamics seen in Physio II annuloplasty do not translate into superior freedom from recurrent MR. The type of annuloplasty device does not influence the long-term results that have previously been reported (27,28). Therefore, in terms of procedural or surgical factors, our study found no factors associated with recurrence of MR. Meanwhile, the use of annuloplasty rings (99.3%) and the implantation of artificial chordae (84.3%) in most patients may explain the good clinical outcomes in our results. Our study has shown that the technique of artificial chordae with a ring annuloplasty can give excellent results (29,30).
Despite the fact that patients with BD underwent more complex repairs with significantly longer operative, CPB, and ACC times, this study demonstrated very acceptable 10-year freedom from reoperation (89.1%) and 10-year survival (98.6%) rates. According to our data, the long-term survival rate of 98.6% is comparable to or better than that of other studies, which ranged from 66% to 85% (14,31). Furthermore, our in-hospital mortality (0.4%), stroke (1.1%), and rethoracotomy (4.0%) rates are low and comparable to other studies (20,32). The mean LOS was 9.10 days, and there were no significant differences between the groups. However, our LOS is shorter than that in other studies (32).
MS versus TEMI
In the present study, the difference in surgical approach was not associated with recurrent MR ≥2+. The TEMI technique can be proposed in cases of complex MV disease. Recent studies have shown that the safety and efficacy outcomes of the TEMI approach are equivalent to those of conventional MS surgery (33). Sakaguchi et al. and De Bonis et al. demonstrated that MVR in patients with BD also provides excellent results via a minimally invasive approach (34,35). TEMI MV surgery can also provide patients with a cosmetically pleasing incision, faster recovery, and a faster return to normal activities (36). Meanwhile, we found that the grade of postoperative MR and LVEF were predictive of the recurrence of regurgitation in the MS approach. In patients treated via the TEMI approach, the concomitance of ASD repair is the main predictor of regurgitation; however, all (three patients) who underwent TEMI were in group B. Follow-up research is needed to clarify whether it is of real significance.
Recurrence and risk factors
MVR is not indicated in all patients with BD, and performing MVR in unsuitable patients would increase the risk of mortality and postoperative recurrence. Durability is the main concern regarding MVR in patients with BD. Previous studies have shown a higher recurrence rate after MVR (4). In our cohort, 87.6% of valves were functional (MR <2+) at the end of follow-up on 1 March 2023 (up to 12 years). This is similar to or better than in other studies that have reported up to 89% in long-term follow-up (9,14). In the multivariate Cox analysis, our study showed that independent predictors of MR recurrence included immediate postoperative MR area, postoperative LVEF, LVEDD, and postoperative MR grade (all P<0.05), and postoperative LVEF was protective (HR =0.931; 95% CI: 0.868–0.999). The present study found that elevated postoperative LVEDD (HR =1.149; 95% CI: 1.016–1.300) and decreased postoperative LVEF showed a trend towards higher recurrence of regurgitation. Previous studies have noted that left ventricular (LV) systolic dysfunction is the ultimate adverse outcome of chronic MR and is the leading cause of postoperative mortality in MVR (37,38). Nappi et al. identified a preoperative LVEDD >62 mm as an independent predictor of poor outcome (39). In addition, LVEF <40% increased the risk of recurrent moderate or severe MR, as shown by David et al. (14) This may be because long-term chronic MR leads to irreversible remodeling of the LV and because LV dysfunction may persist into the postoperative period, thus affecting postoperative recovery. Patients with severe MR, even if asymptomatic, should therefore be recommended for surgical repair as soon as possible. Furthermore, Morisaki et al. showed that the independent risk factors for moderate to severe recurrent regurgitation in a previous study of 362 patients who underwent successful MVR were residual regurgitation ≥ mild (29). This finding suggests that MVR may be the optimal choice for patients with BD after careful selection, particularly in the early stages of BD with predominant MR. Careful assessment of LV function and residual MR by experienced surgeons may be crucial for durable MVR in patients with BD. However, considering the differences in patient characteristics, this result might be statistically overestimated. Further studies should be performed in the future to investigate these factors.
Study limitations
This study did have some inherent limitations. It was a retrospective observational study, single-center, and uncontrolled, which allows for potential bias. Moreover, for both groups of patients, most of the cases were censored. Such a high level of censored data makes the available results highly biased, which affects the credibility of the results. This is one of the main limitations of the study. Further large randomized controlled trials with long-term follow-up are needed to determine the feasibility of MVR in patients with BD.
Conclusions
According to our study, MVR for patients with BD presented a beneficial survival effect. However, MVR was associated with a certain risk of MR recurrence, especially in those with high postoperative LVEDD, residual MR >1+, and decreased postoperative LVEF. We recommend MVR for patients with BD, especially for those with early-stage disease.
Acknowledgments
The paper was originally presented at the AATS Annual Meeting. We would like to thank Professor Yingjie Wang of the University of Oxford for grammar proofreading.
Funding: This study was supported by t
Footnote
Reporting Checklist: The authors have completed the STROCSS reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-1768/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1768/coif). H.H. reports that this study was supported by the National Natural Science Foundation of China (No. 82270373), the Department of Science and Technology of Guangdong Province (No. 2020B1111170011), the Guangdong Basic and Applied Basic Research Foundation (No. 2019B1515120071), and the High-Level Hospital Construction Project of Guangdong Provincial People’s Hospital (No. 2023P-GX08). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Institutional Review Board at Guangdong Provincial People’s Hospital (No. KY-Q-2021-271-02; 2022.1.29 approval) and conformed to the Declaration of Helsinki (as revised in 2013). The requirement for obtaining informed consent was exempted due to the retrospective nature of the study with minimal risk.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Soulat-Dufour L, Addetia K. Degenerative mitral regurgitation. Curr Opin Cardiol 2020;35:454-63. [Crossref] [PubMed]
- Chemtob RA, Mick S, Gillinov M, Hodges K, Wierup P. Repair of bileaflet prolapse in Barlow syndrome: The 4-chord technique. J Card Surg 2019;34:605-9. [Crossref] [PubMed]
- Flameng W, Herijgers P, Bogaerts K. Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation 2003;107:1609-13. [Crossref] [PubMed]
- Flameng W, Meuris B, Herijgers P, Herregods MC. Durability of mitral valve repair in Barlow disease versus fibroelastic deficiency. J Thorac Cardiovasc Surg 2008;135:274-82. [Crossref] [PubMed]
- Jouan J, Berrebi A, Chauvaud S, Menasché P, Carpentier A, Fabiani JN. Mitral valve reconstruction in Barlow disease: long-term echographic results and implications for surgical management. J Thorac Cardiovasc Surg 2012;143:S17-20. [Crossref] [PubMed]
- Fornes P, Heudes D, Fuzellier JF, Tixier D, Bruneval P, Carpentier A. Correlation between clinical and histologic patterns of degenerative mitral valve insufficiency: a histomorphometric study of 130 excised segments. Cardiovasc Pathol 1999;8:81-92. [Crossref] [PubMed]
- Savage EB, Ferguson TB Jr, DiSesa VJ. Use of mitral valve repair: analysis of contemporary United States experience reported to the Society of Thoracic Surgeons National Cardiac Database. Ann Thorac Surg 2003;75:820-5. [Crossref] [PubMed]
- Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJAmerican Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003;16:777-802. [Crossref] [PubMed]
- Mazine A, Friedrich JO, Nedadur R, Verma S, Ouzounian M, Jüni P, Puskas JD, Yanagawa B. Systematic review and meta-analysis of chordal replacement versus leaflet resection for posterior mitral leaflet prolapse. J Thorac Cardiovasc Surg 2018;155:120-128.e10. [Crossref] [PubMed]
- Seeburger J, Borger MA, Doll N, Walther T, Passage J, Falk V, Mohr FW. Comparison of outcomes of minimally invasive mitral valve surgery for posterior, anterior and bileaflet prolapse. Eur J Cardiothorac Surg 2009;36:532-8.
- Zhang L, Cui H, Shen H, Li D, Li L, Shen H, Jiang S. Mid-term clinical outcomes of totally endoscopic repair for mitral regurgitation in Barlow's disease. J Cardiothorac Surg 2024;19:233. [Crossref] [PubMed]
- Faerber G, Tkebuchava S, Diab M, Schulze C, Bauer M, Doenst T. Minimally-invasive mitral valve repair of symmetric and asymmetric Barlow’s disease. Clin Res Cardiol 2021;110:1881-9. [Crossref] [PubMed]
- Tomšic A, Hiemstra YL, van der Pas SL, Putter H, Versteegh MIM, van Brakel TJ, Ajmone Marsan N, Klautz RJM, Palmen M. Early and long-term outcomes of mitral valve repair for Barlow's disease: a single-centre 16-year experience. Interact Cardiovasc Thorac Surg 2018;26:783-9. [Crossref] [PubMed]
- David TE, David CM, Lafreniere-Roula M, Manlhiot C. Long-term outcomes of chordal replacement with expanded polytetrafluoroethylene sutures to repair mitral leaflet prolapse. J Thorac Cardiovasc Surg 2020;160:385-394.e1. [Crossref] [PubMed]
- Passos L, Aymard T, Biaggi P, Morjan M, Emmert MY, Gruenenfelder J, Reser D. Midterm outcomes of minimally invasive mitral valve surgery in a heterogeneous valve pathology cohort: respect or resect? J Thorac Dis 2023;15:3013-24. [Crossref] [PubMed]
- De Bonis M, Lorusso R, Lapenna E, Kassem S, De Cicco G, Torracca L, Maisano F, La Canna G, Alfieri O. Similar long-term results of mitral valve repair for anterior compared with posterior leaflet prolapse. J Thorac Cardiovasc Surg 2006;131:364-70. [Crossref] [PubMed]
- Agnino A, Graniero A, Roscitano C, Villari N, Marvelli A, Verhoye JP, Anselmi A. Continued follow-up of the free margin running suture technique for mitral repair. Eur J Cardiothorac Surg 2020;58:847-54. [Crossref] [PubMed]
- Phillips MR, Daly RC, Schaff HV, Dearani JA, Mullany CJ, Orszulak TA. Repair of anterior leaflet mitral valve prolapse: chordal replacement versus chordal shortening. Ann Thorac Surg 2000;69:25-9. [Crossref] [PubMed]
- Hirji SA, Del Val FR, Yazdchi F, Lee J, Ejiofor J, Kolkailah AA, Chowdhury R, McGurk S, Kaneko T. Mitral valve repair using edge-to-edge technique in various situations: real-world experiences. Eur J Cardiothorac Surg 2019;56:1110-6. [Crossref] [PubMed]
- Pfannmueller B, Misfeld M, Verevkin A, Garbade J, Holzhey DM, Davierwala P, Seeburger J, Noack T, Borger MA. Loop neochord versus leaflet resection techniques for minimally invasive mitral valve repair: long-term results. Eur J Cardiothorac Surg 2021;59:180-6. [Crossref] [PubMed]
- Kasegawa H, Shimizu A, Fukui T, Takanashi S, Shimokawa T. Mitral valve repair for extreme billowing and prolapsing valve. JTCVS Open 2022;10:169-75. [Crossref] [PubMed]
- Lawrie GM, Earle EA, Earle NR. Nonresectional repair of the barlow mitral valve: importance of dynamic annular evaluation. Ann Thorac Surg 2009;88:1191-6. [Crossref] [PubMed]
- Hiemstra YL, Tomsic A, Gripari P, van Wijngaarden AL, van der Pas SL, Palmen M, Klautz RJM, Pepi M, Bax JJ, Delgado V, Marsan NA. Evolution from mitral annular dysfunction to severe mitral regurgitation in Barlow's disease. Interact Cardiovasc Thorac Surg 2021;32:506-14. [Crossref] [PubMed]
- van Wijngaarden SE, Kamperidis V, Regeer MV, Palmen M, Schalij MJ, Klautz RJ, Bax JJ, Ajmone Marsan N, Delgado V. Three-dimensional assessment of mitral valve annulus dynamics and impact on quantification of mitral regurgitation. Eur Heart J Cardiovasc Imaging 2018;19:176-84. [Crossref] [PubMed]
- Ben Zekry S, Spiegelstein D, Sternik L, Lev I, Kogan A, Kuperstein R, Raanani E. Simple repair approach for mitral regurgitation in Barlow disease. J Thorac Cardiovasc Surg 2015;150:1071-7.e1. [Crossref] [PubMed]
- Adams DH, Anyanwu AC, Rahmanian PB, Abascal V, Salzberg SP, Filsoufi F. Large annuloplasty rings facilitate mitral valve repair in Barlow's disease. Ann Thorac Surg 2006;82:2096-100; discussion 2101. [Crossref] [PubMed]
- Sidiki AI, Akulova AA, Hussein MH, Al-Ariki MK, Donsov VV, Iluhin MA, Limeshkin AA, Ananko VA. Physio and Physio II rings: beyond the annular physiology. J Cardiovasc Surg (Torino) 2022;63:529-35. [Crossref] [PubMed]
- Del Forno B, Carino D, Bisogno A, Rizzello A, Lapenna E, Ascione G, Gramegna F, Iaci G, Agricola E, Monaco F, Alfieri O, Castiglioni A, Maisano F, De Bonis M. Mitral Repair With Complete Rings or Posterior Bands in Barlow Disease: Long-term Results. Ann Thorac Surg 2023;115:421-7. [Crossref] [PubMed]
- Morisaki A, Takahashi Y, Fujii H, Sakon Y, Murakami T, Shibata T. Outcomes of loop technique with ring annuloplasty: a > 10-year experience. Gen Thorac Cardiovasc Surg 2022;70:793-803. [Crossref] [PubMed]
- Lawrie G, Zoghbi W, Little S, Shah D, Earle N, Earle E. One Hundred Percent Reparability of Mitral Prolapse: Results of a Dynamic Nonresectional Technique. Ann Thorac Surg 2021;112:1921-8. [Crossref] [PubMed]
- Ma J, Liu J, Wei P, Yao X, Zhang Y, Fang L, Chen Z, Liu Y, Tan T, Wu H, Huang H, Xie B, Chen J, Zhuang J, Guo H. Quadrangular resection versus chordal replacement for degenerative posterior mitral leaflet prolapse. Ann Transl Med 2021;9:60. [Crossref] [PubMed]
- Dreyfus GD, Dulguerov F, Marcacci C, Haley SR, Gkouma A, Dommerc C, Albert A. "Respect when you can, resect when you should": A realistic approach to posterior leaflet mitral valve repair. J Thorac Cardiovasc Surg 2018;156:1856-1866.e3. [Crossref] [PubMed]
- Moscarelli M, Fattouch K, Gaudino M, Nasso G, Paparella D, Punjabi P, Athanasiou T, Benedetto U, Angelini GD, Santarpino G, Speziale G. Minimal Access Versus Sternotomy for Complex Mitral Valve Repair: A Meta-Analysis. Ann Thorac Surg 2020;109:737-44. [Crossref] [PubMed]
- Sakaguchi T, Totsugawa T, Hayashida A, Ryomoto M, Sekiya N, Tamura K, Hiraoka A, Yoshitaka H. Stepwise mitral valve repair for Barlow's disease via a minimally invasive approach. J Card Surg 2020;35:1471-6. [Crossref] [PubMed]
- De Bonis M, Lapenna E, Del Forno B, Di Sanzo S, Giacomini A, Schiavi D, Vicentini L, Latib A, Pozzoli A, Pappalardo F, La Canna G, Alfieri O. Minimally invasive or conventional edge-to-edge repair for severe mitral regurgitation due to bileaflet prolapse in Barlow's disease: does the surgical approach have an impact on the long-term results? Eur J Cardiothorac Surg 2017;52:131-6. [Crossref] [PubMed]
- Melnitchouk SI, Seeburger J, Kaeding AF, Misfeld M, Mohr FW, Borger MA. Barlow's mitral valve disease: results of conventional and minimally invasive repair approaches. Ann Cardiothorac Surg 2013;2:768-73. [Crossref] [PubMed]
- Pu M, Gao Z, Zhang X, Liao D, Pu DK, Brennan T, Davidson WR Jr. Impact of mitral regurgitation on left ventricular anatomic and molecular remodeling and systolic function: implication for outcome. Am J Physiol Heart Circ Physiol 2009;296:H1727-32. [Crossref] [PubMed]
- Gerber W, Sanetra K, Drzewiecka-Gerber A, Jankowska-Sanetra J, Bochenek A, Zembala M, Cisowski M. Echocardiographic evaluation of the results of minimally invasive repair of asymptomatic mitral regurgitation. Kardiol Pol 2019;77:56-8. [Crossref] [PubMed]
- Nappi F, Nenna A, Spadaccio C, Lusini M, Chello M, Fraldi M, Acar C. Predictive factors of long-term results following valve repair in ischemic mitral valve prolapse. Int J Cardiol 2016;204:218-28. [Crossref] [PubMed]


