
Giant gluteal lipoma presenting as sciatic hernia: a case description
Introduction
When the peritoneal sac and its contents protrude through the larger or lesser sciatic foramen, this is referred to as sciatic hernia (SH) which was first described by Papen in 1750 (1). As one of the rarest types of hernia, SH frequently poses a diagnostic challenge to physicians. The three categories of SH include type 1 (supra piriform), type 2 (sub piriform), and type 3 (subspinous), with type 3 being the least frequent (2). Lipomas are benign tumors composed of mature fat cells and are most commonly mesenchymal (3). Typically, lipomas remain in the subcutaneous tissue and do not cause symptoms. However, they can also appear in deeper areas and exert pressure on the surrounding tissues, including nerves (4). Lipomas can reach a considerable size before symptoms appear. Herein, we report a case of a deep-seated gluteal lipoma protruding into the intrapelvic region with symptoms of pelvic compression.
Case presentation
A 61-year-old female was admitted to the hospital due to complaints of a mass that had developed 1 year prior in the right buttock. The mass was described as approximately the size of a goose egg when the patient first noticed it, but no treatment was prescribed due to the lack of discomfort. The mass increased progressively, and she subsequently developed numbness in the right lower limb over the 3 months prior to the hospital visit. The patient also noted a change in defecation habits, with a recent development of constipation. The patient had no significant past medical history of surgery, medication, trauma, cancer, hip accidents, or unexplained weight loss. Physical examination revealed a body mass index (BMI) of 26.6 kg/m2, a tender abdomen, and no masses or signs of peritonitis. However, pain was present that increased with the straightening of her right leg. A large mass was noted on the right buttock during the physical exam, measuring approximately 15 cm × 15 cm in size. She also reported pain radiating down the back of her thigh exacerbated by dorsiflexion which was likely due to compression of the sciatic nerve. Digital rectal examination revealed a mass, tough in quality, poor in motion, and tender. Hematological and biochemical workups, including assessments of complete blood counts, renal function, liver function, and coagulation profiles were within the normal ranges.
A computed tomography (CT) scan of the pelvis and ultrasound-guided fine needle aspiration of the gluteal area were performed to determine the type of gluteal tumor. The pelvic CT scan revealed a dumbbell-shaped mass inside the pelvis and behind the gluteus maximus that was connecting through the greater ischiatic foramina (Figure 1A-1C). The mass was large, with an intact envelope, and there was no enhancement observed after contrast administration. The mass was homogeneously isointense with fat and approximately 184 mm × 16 mm in size. The bladder and uterus were forced to the left due to the pelvic organs being dislodged by the mass’s size and location. Superficial ultrasound revealed that the right gluteus muscle was significantly thicker than was the contralateral muscle and had an uneven echo. Magnetic resonance imaging (MRI) revealed space-occupying lesions in the right buttock and pelvic cavity, approximately 112 mm × 184 mm × 125 mm in size, with clear boundaries and smooth edges, resulting in the displacement of the pelvic bowel and uterus due to pressure (Figure 2A-2C). The mass was considered likely to be a lipoma based on imaging findings, as it was isointense with fat throughout. No additional radiological evidence of damage was observed other than its substantial size and deep position. The coronal view on the magnetic resonance neuroimaging short tau inversion recovery (STIR) sequence showed that the tumor was in close proximity to and compressed the right sciatic nerve, resulting in edematous thickening and a high signal in the right sciatic nerve (Figure 3). After informed consent was obtained, an ultrasound-guided aspiration biopsy of the right buttock mass revealed a minor quantity of fiber, blood vessels, and fat tissue, without signs of malignancy. A tentative diagnosis of a lipoma was made based on the findings, and the patient provided consent for the lump to be surgically removed.



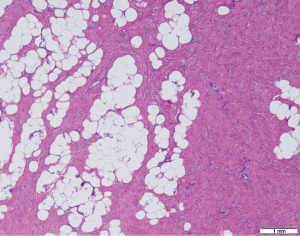
A multidisciplinary discussion on spinal surgery, vascular surgery, and interventional and general surgery was conducted. Based on the three-dimensional reconstruction technique, we could define the surrounding anatomic features to facilitate adequate tumor removal. The surgical plan included a two-pronged approach, including a transgluteal approach and a sacrococcygeal approach. The patient was placed in the left lateral position under general anesthesia. Due to the large size of the tumor and its proximity to the internal iliac vein, the risk of intraoperative bleeding was high. Thus, balloon implantation of the abdominal aorta was performed by the interventional team on the day of surgery. An orthopedist monitored the sciatic nerve during the treatment to ensure it was unharmed. First, a surgical incision was made on the skin parallel to the gluteus maximus fibers, and another incision was made where the mass protruded the most, corresponding to the sciatic nerve course. The subcutaneous deep fascia was then cut layer by layer to bluntly separate the gluteus maximus muscle fibers and expose the yellowish mass (Figure 4A). The capsule of the mass was intact and separated from the surrounding tissues without signs of malignancy. The tumor vessels were ligated in turn and were found to be connected to the pelvic tumor through the greater ischial foramina. It was found that the tumor had squeezed the sciatic nerve. The boundary between the tumor and the nerve was clear, and the nerve was protected during the operation (Figure 4B). After removal of the tumor at the greater ischiatic foramina, irrigation and gauze filling of the surgical area were performed by the general surgeon. The skin, subcutaneous tissue, superficial fascia, and deep fascia were incised layer by layer approximately 2 cm from the right side of the sacrococcygeal bone, parallel to the spinal incision. After a consultation at the operating table with the spine surgeon, the coccygeal bones were excised by an ultrasound osteotome device, and the apex of the coccygeal bone was excised along the periosteum. Part of the tumor was exposed on the right anterior side of the sacrum and coccygeal bone, and the tumor was completely resected along the tumor envelope. No rectal wall injury was observed. The residual cavity was rinsed with iodine saline, and two multichannel drainage tubes were placed in a curved shape. The end of the tube that was not inserted into the cavity was left to protrude through the skin of the right buttock and was fixed by a suture. Finally, the incisions were sutured in layers. Pathological evaluation revealed the tumor to be a lobulated mass of adipose tissue measuring 360 mm × 215 mm in size (Figure 4C). Histopathological evaluations confirmed a benign lipoma with localized high fibrous tissue and fat necrosis. No signs of malignancy were identified (Figure 5). Because the bulk tissue of the tumor was morphologically and microscopically benign and tumor characteristics unlike those of malignant liposarcomas, we did not examine the MDM2 gene. After surgery, the patient’s constipation subsided, and the numbness in the right lower limb was significantly reduced. The patient healed without incident and was released 13 days later. Six months following the operation, a single CT scan was suggested. All procedures performed in this study were in accordance with the relevant institution’s ethical standards and the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.

Discussion
Superficial lipomas are a common type of benign adipose tissue tumor (5). Deep lipomas, however, are uncommon and need to be distinguished from well-differentiated liposarcomas to receive specific care and follow-up (6). CT and MRI scans are useful tools for differentiating between benign and malignant tumors, and their characteristic imaging manifestations are crucial for the diagnosis of adipose tumors such as lipomas or liposarcomas.
The thickening of the septa, associated nonadipose masses, and a proportion of nonadipose tissue of more than 25% of the lesion assist in differentiating liposarcomas from lipomas (7). In the case reported here, the lesion was predominantly composed of fat and exhibited few thin nonenhancing low-signal intervals. The lack of a significant nonfatty component or thickened septa ruled out the possibility of a liposarcoma. Histopathologic examinations are essential to eliminating the possibility of liposarcomas because they provide a definitive diagnoses and ensure that treatment is appropriately targeted. Ultrasound-guided puncture biopsy of the right gluteal mass and postoperative histopathology examinations revealed benign neoplastic tissue, thus ruling out the possibility of malignancy and confirming the diagnosis of a benign tumor.
Retroperitoneal lipomas are often asymptomatic before they induce abdominal swelling or discomfort due to the blockage or displacement of surrounding organs and tissues (8). When they reach a large size, as in our case, they can cause pelvic organ displacement or compression of the sciatic nerve, thus resulting in symptoms. The term “inverse sciatic hernia” is used to describe lipomatous SHs in the gluteal region that pass through the sciatic foramen into the pelvis. It should be noted that this is not the same as nonlipomatous SHs, which occur when the contents of the abdominal or pelvic cavity bulge into the gluteal area through the sciatic foramen (9).
Various treatment approaches have been reported for SH, but a consensus regarding the best approach is lacking. Surgical approaches described in the literature include a transgluteal incision, a transabdominal incision, a combined abdominal and gluteal approach, an extraperitoneal approach, an abdominoperineal approach, the Kocher-Langenbeck approach, and the laparoscopic approach. Immediate surgical treatment is essential for SHs that result in symptoms or those that present with incarcerated or strangulated contents (10).
A transabdominal approach is highly recommended for patients experiencing intestinal blockage or requiring exploratory laparotomy due to unclear abdominal or pelvic symptoms (11). However, if the hernias are simple or reducible, they can be treated using a transgluteus maximus muscle approach when a radiological diagnosis has been made and proper preparation completed (12). In this approach, the muscle of the buttock can be divided along a line that runs from the major trochanter to the center of the sacrum, which corresponds to the path of the piriform muscle (11).
In our case, because the patient’s lipoma was compressing the sciatic nerve and was accompanied by numbness in the right lower limb, it was necessary to operate to prevent further damage to the sciatic nerve. The pelvic portion of the tumor was large and could not be resected in a single operation via the gluteal approach. However, if the combined transgluteal abdominal approach had been used, it might have produced postoperative complications such as intestinal adhesion due to the patient’s increased age.
Well-established preoperative examinations, including pelvic CT and MRI, allowed us to clarify the anatomical relationship between the lipoma and the pelvic organs, blood vessels, and nerves in the buttocks. Such examinations ensured that we could remove the lipoma via pelvic osteotomy and the combined transgluteal and sacrococcygeal approaches. Compared to the combined transgluteal abdominal approach, the combined sacrococcygeal-gluteal approach greatly minimizes injury to the patient and allows for the rapid recovery of the smaller incision. The transgluteal approach carries the risk of injury to blood vessels and nerves, particularly if localized scar tissue is present. However, the transgluteal approach is an essential part of combined surgery and can completely remove small tumors located in the retroperitoneum via the sciatic foramen. Based on the preoperative MRI and CT scans, the size of the tumor and its surrounding anatomical structures could be clearly observed. The tumor was a dumbbell-shaped lipoma that extended through the sciatic foramen magnum.
The preoperative MRI and CT scans provided a reference for our subsequent surgical approach and allowed the tumor to be adequately and safely resected in a single session. Magnetic resonance neuroimaging was able to reveal compression of the sciatic nerve. We found that in this case, we could adopt pelvic osteotomy and a combined transgluteal-sacrococcygeal approach to remove the tumor in a single stage, thus avoiding laparotomy (Figure 6). Using this surgical method, we intraoperatively identified a large lipoma passing through the greater sciatic foramen and compressing the sciatic nerve. Following surgery, the patient’s constipation resolved, and the numbness in the right lower limb was significantly reduced. Thus, we believe that this surgical approach is an effective method for lipomatous SH, particularly when the lipoma is too large to be removed through the sciatic foramen.

Acknowledgments
Funding: This study was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1214/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institution and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Martel L. Pointede hernie ischiatique: impotence fonctionelle du membre inferieur pendant 5 mois operation Guerison. Loire Med 1900;19:165-74.
- Javid PJ, Brooks DC. Maingot’s Abdominal Operations. New York: McGraw Hill. Hernias 2007; pp:103-139.
- Pimenta R, Matos RM, Proença R, Pereira HR, Pinto R. Giant buttock lipoma with an atypical presentation as a sciatic hernia--case report. Acta Reumatol Port 2014;39:91-3. [PubMed]
- López-Tomassetti Fernández EM, Hernández JR, Esparragon JC, García AT, Jorge VN. Intermuscular lipoma of the gluteus muscles compressing the sciatic nerve: an inverted sciatic hernia. J Neurosurg 2012;117:795-9. [Crossref] [PubMed]
- Al-Ali MHM, Salih AM, Ahmed OF, Kakamad FH, Mohammed SH, Hassan MN, Sidiq SH, Mustafa MQ, Najar KA, Abdullah IY. Retroperitoneal lipoma; a benign condition with frightening presentation. Int J Surg Case Rep 2019;57:63-6. [Crossref] [PubMed]
- Casali PG, Abecassis N, Aro HT, Bauer S, Biagini R, Bielack S, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018;29:iv51-67. [Crossref] [PubMed]
- Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors: distinction of lipoma and well-differentiated liposarcoma. Radiology 2002;224:99-104. [Crossref] [PubMed]
- Weniger M, D’Haese JG, Kunz W, Pratschke S, Guba M, Werner J, Angele MK. En-bloc resection of a giant retroperitoneal lipoma: a case report and review of the literature. BMC Res Notes 2015;8:75. [Crossref] [PubMed]
- Kaur N, Kaur N, Chhabra HS, Singh M, Singh P. A case report of sciatic hernia as a cause of sciatica and lower back pain: Diagnostic dilemma for family physicians. J Family Med Prim Care 2022;11:3304-7. [Crossref] [PubMed]
- Yu PC, Ko SF, Lee TY, Ng SH, Huang CC, Wan YL. Small bowel obstruction due to incarcerated sciatic hernia: ultrasound diagnosis. Br J Radiol 2002;75:381-3. [Crossref] [PubMed]
- Losanoff JE, Basson MD, Gruber SA, Weaver DW. Sciatic hernia: a comprehensive review of the world literature (1900-2008). Am J Surg 2010;199:52-9. [Crossref] [PubMed]
- Hayashi N, Suwa T, Kimura F, Okuno A, Ishizuka M, Kakizaki S, Kawakami H. Radiographic diagnosis and surgical repair of a sciatic hernia: report of a case. Surg Today 1995;25:1066-8. [Crossref] [PubMed]


